Abstract
We report a 66-year-old woman with complex regional pain syndrome (CRPS) 1 treated with combined medical and active physical therapy. She was diagnosed with CRPS 1 following partial shoulder prosthesis due to proximal humerus fracture. Despite continuous medication and physical therapy, there was no improvement in her pain and functional outcome. Her overall pain was decresed by stellate ganglion block 3 times in two weeks conducted during the second month of the follow-up period. Following the ganglion blockades, pain and the other symptoms were decreased intermittently but range of motion (ROM) and functional status were not satisfied as much as expected. After the third month of follow-up, her passive and active ROM of the shoulder joint was increased after application of manipulation under general anesthesia. In conclusion, because CRPS 1 remains one of the most difficult pain syndromes, early diagnosis and treatment are important to have adequate functional results from physical therapy. Manipulation under general anesthesia may be an additional effective treatment tool to obtain functional improvement in some patients diagnosed with CRPS 1.
Go to : 
CRPS is a progressive disease characterized by severe pain, swelling and changes in the skin [1]. CRPS most often affects one of the arms, legs, hands or feet, with pain often spreading to the entire arm and leg. Typical features include dramatic changes in the color and temperature of the skin over the affected limb or body part accompanied by intense burning pain, skin sensitivity, swelling, sweating and restricted range of motion (ROM). The two types of CRPS are as follows: Type I (previously known as reflex sympathetic dystrophy syndrome) occurs after illness of injury directly damage the nerves in your affected limb; Type II, once referred to as causalgia, follows a distinct nerve injury. About 90% percent of CRPS cases are type I. Many CRPS cases occur after forceful trauma to the arm or leg.
In this study, we aimed to evaluate the clinical outcome of a conservative rehabilitation program for the treatment of CRPS after shoulder prosthesis.
A 66-year-old female had partial shoulder prosthesis following proximal humerus fracture. Post-op 2nd day, she began passive range of motion (ROM) and isometric strengthening exercises in the physical therapy department. Home exercises were given twice a day and each exercise was done with 20 repetitions. A cold pack was applied after exercise in the clinic and was recommended for application at home after exercise. The shoulder was placed in a sling for 4 weeks following surgery.
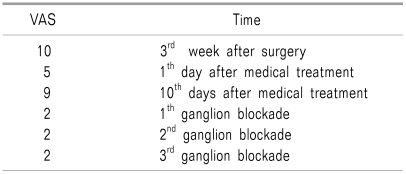
Post-op 3rd week, she complained of progressive pain, causalgia, and burning starting from the elbow and extending to the hand (visual analogue scale, VAS:10) and mild restricted ROM was observed. She was diagnosed with reflex sympathetic dystrophy (RSD) and medical treatment, such as nonsteroidal anti-inflammatory drugs and paracetamol, were given, and transcutaneous electrical nerve stimulation and contrast bath therapy were added to the physical therapy program; however, intensity and frequency of exercises were reduced. Contrast bath therapy, also known as hot/cold immersion therapy, is a form of treatment where a limb or the entire body is immersed in ice water followed by the immediate immersion of the limb or body in warm water in order to reduce edema and inflammation. Her complaints did not change after 2 weeks of supportive medication and physical therapy, so she was directed to the pain clinic.
She was diagnosed by the pain specialist as having CRPS type I (new term for RSD) by clinical examination under the diagnostic criteria of burning pain, allodynia, skin color and temperature changes, swelling, decreased ROM, trophic changes in nail or skin and weakness. Infrared thermography was done, as well. She was prescribed gabapentin (900 mg/day), tramadol (37.5 mg/day), vitamin C (500 mg/day), and magnesium (300 mg/day) in addition to previous medication. Numbness, pricking, edema, and strong pain decreased after that and effective physical therapy was started (VAS:5). There were some improvements in symptoms up until ten days after the new medication was begun. At that point, the patient complained of progressive tingling sensation, pain, and pricking along the arm (VAS:9).
Active assisted ROM exercises were continued as much as possible, but pain, swelling and sensitivity only allowed limited exercise. The home exercise program was also affected.
The two months following surgery symptoms did not improve by physical therapy and medication and a sympathetic block of the stellate ganglion was performed by the pain specialist. Symptoms, especially pain, noticably improved (VAS:2). Dosage of gabapentin was intermittently increased from 900 to 2,400 mg/day, and vitamin C (500 mg/day) and magnesium (300 mg/day) were continued. The patient's complaints dramatically decreased after the first course of ganglion blockade, but after 2 days, pain started again with moderate intensity (VAS:4). Because of these pain attacks, ROM and muscle strength gains were not as much as expected after surgery. Therefore, ROM, strenghtening and stretchening exercises and contrast bath therapy were applied as much as possible. A second stellate ganglion blockade was applied (VAS:2) after 4 days following the first stellate blockade and the third course (VAS:1) was applied after 1 week. Tramadol (37.5 mg/day), gabapentin (600 mg/day), contrast bath and physical therapy program were continued following blockades.
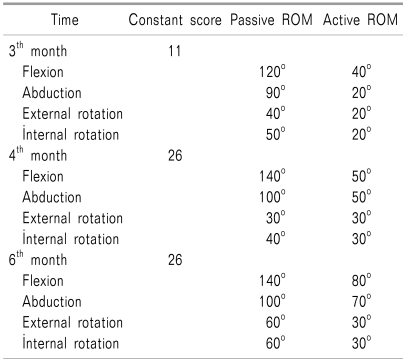
After 3 months, passive flexion, abduction, external rotation and internal rotation were 120°, 90°, 40° and 50°, respectively, and active were 40°, 20°, 20° and 50°, respectively. Functional status of the patient was assessed by Constant Score. The Constant Score is a functional outcome measurement consisting of four variables used to assess shoulder function, with a maximum score of 100. At the end of the 3 months, Constant Score and VAS were 11 and 2, respectively. Her clinic-based therapy program was discontinued and she was advised to continue home exercises twice a day. She continued taking gabapentin (600 mg/day), vitamin C (500 mg/day) and magnesium (300 mg/day) during the following 3 months.
At the end of the 4th month, improvements, especially in active and passive flexion, made through the home exercise program were not enough. Manipulation was applied under general anesthesia by her surgeon, and an intensive rehabilitation program was started 3 times a week. Manipulation under anesthesia was applied once and the procedure was forceful flexion, abduction and external rotation, respectively. The sixth-month results of forward flexion (Fig. 1), abduction, external, internal rotation and Constant score are given in Table 1; VAS is given in Table 2.
Go to : 
The International Association for the Study of Pain named and divided CRPS into type 1 and type 2. Type 1 is similar to RSD without nerve injury after soft tissue injury, and type 2 is similar to causalgia after nerve injury. CRPS is a neurogenic pain caused by trauma, fracture, operation, nerve injury, etc, and is characterized by various types of pain (tingling, allodynia, hypersentitive to pain etc), functional loss of autonomous nerves and motor nerves, and by edema and dystrophy change. There is no single proven diagnostic tool, but taking a detailed history and understanding the chief complaint, along with the use of simple radiography, 3-phase bone scanning and infrared thermography, can help diagnose CRPS. However, the most important thing is the clinical decision, with the exclusion of other diagnoses such as Raynaud syndrome, osteomyelitis cellulitis, Dupuytren contracture, and atypical romatoid arthritis [2]. Early diagnosis and treatment is crucial for prognosis of orthopedic trauma and effective physical therapy. Patients can have persistent impairments at 2 or more years after onset [3]. If the purpose of the treatment is to gain ROM, muscle strength and improved functional results, the symptoms of swelling, burning pain, and allodynia should be solved.
Pain is the most studied symptom of CPRS, and there are many treatment methods explained in the literature. Schwartzman et al. [4] found ketamine was much more effective than placebo. Ketamine is the most tried analgesic but it has no demonstrable effect on functional results [5]. Ketamine infusion with peripheral nerve block has been used for CPRS I after foot trauma [6], while Finch et al. [7] advised topical ketamine treatment.
Physical therapy always contributed with medical treatment so that specific effect of physical therapy was not known [8]. Gellman stated that physical therapy with ganglion blockage can be effective [9]. In our case, we conducted physical therapy with medical treatment; however, satisfying improvement was not achieved so ganglion blockade was performed three times in two weeks to reduce symptoms and to apply effective physical therapy. It is important to know when and how often ganglion blockage should be performed. Ackerman and Zhang [10] advised to apply it as soon as symptoms start.
In our case, time between surgery and stellate ganglion blockade was 2 months. This period was very crucial for rehabilitation of the shoulder prosthesis. However, CRPS symptoms prevented effective physiotherapy, and we therefore could not get good functional results.
CRPS may follow shoulder surgery. If there is unexpected pain, tingling and allodynia suspected, clinicians should consider CRPS. It is necessary to provide these patients with a multidisciplinary approach and understand that the treatment is most importantly directed toward restoration of full function of the affected area. In conclusion, to diagnose CRPS as early as possible and treat more effectively and accurately is important to apply effective physical therapy and attain good functional results.
Go to : 
References
1. Baron R. Mcmahon SB, Koltzenburg M, editors. Complex regional pain syndrome. Text book of pain. 2006. 5th ed. Elsevier, Churchill Livingstone;p. 1011–1027.
2. Doury P, Dequeker J. Klippel JH, Dieppe PA, editors. Algodystrophy/Reflex sympathetic dystrophy syndrome. Rheumatology. 1998. London: Mosby;p. 1–8.
3. de Mos M, Huygen FJ, van der Hoeven-Borgman M, Dieleman JP, Ch Stricker BH, Sturkenboom MC. Outcome of the complex regional pain syndrome. Clin J Pain. 2009; 25:590–597. PMID: 19692800.

4. Schwartzman RJ, Erwin KL, Alexander GM. The natural history of complex regional pain syndrome. Clin J Pain. 2009; 25:273–280. PMID: 19590474.

5. Sigtermans MJ, van Hilten JJ, Bauer MC, Arbous MS, Marinus J, Sarton EY, et al. Ketamine produces effective and long-term pain relief in patients with Complex Regional Pain Syndrome Type 1. Pain. 2009; 145:304–311. PMID: 19604642.

6. Everett A, Mclean B, Plunkett A, Buckenmaier C. A unique presentation of complex regional pain syndrome type I treated with a continuous sciatic peripheral nerve block and parenteral ketamine infusion: a case report. Pain Med. 2009; 10:1136–1139. PMID: 19744217.

7. Finch PM, Knudsen L, Drummond PD. Reduction of allodynia in patients with complex regional pain syndrome: a double-blind placebo-controlled trial of topical ketamine. Pain. 2009; 146:18–25. PMID: 19703730.

8. Daly AE, Bialocerkowski AE. Does evidence support physiotherapy management of adult Complex Regional Pain Syndrome Type One? A systematic review. Eur J Pain. 2009; 13:339–353. PMID: 18619873.

9. Gellman H. Reflex sympathetic dystrophy: alternative modalities for pain management. Instr Course Lect. 2000; 49:549–557. PMID: 10829209.
10. Ackerman WE, Zhang JM. Efficacy of stellate ganglion blockade for the management of type 1 complex regional pain syndrome. South Med J. 2006; 99:1084–1088. PMID: 17100029.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download