This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The first sacral nerve root block (S1NRB) is a common procedure in pain clinic for patients complaining of low back pain with radiating pain. It can be performed in the office based setting without C-arm. The previously suggested method of locating the needle entry point begins with identifying the posterior superior iliac spine (PSIS). Then a line is drawn between two points, one of which is 1.5 cm medial to the PSIS, and the other of which is 1.5 cm lateral and cephalad to the ipsilateral cornu. After that, one point on the line, which is 1.5 cm cephalad to the level of the PSIS, is considered as the needle entry point. The purpose of this study was to analyze the location of needle entry point and palpated PSIS in S1NRB.
Methods
Fifty patients undergoing C-arm guided S1NRB in the prone position were examined. The surface anatomical relationships between the palpated PSIS and the needle entry point were assessed.
Results
The analysis revealed that the transverse and vertical distance between the needle entry point and PSIS were 28.7 ± 8.8 mm medially and 3.5 ± 14.0 mm caudally, respectively. The transverse distance was 27.8 ± 8.3 mm medially for male and 29.5 ± 9.3 mm medially for female. The vertical distance was 1.0 ± 14.1 mm cranially for male and 8.1 ± 12.7 mm caudally for female.
Conclusions
The needle entry point in S1NRB is located on the same line or in the caudal direction from the PSIS in a considerable number of cases. Therefore previous recommended methods cannot be applied to many cases.
Go to :

Keywords: first sacral nerve root block, needle entry point, posterior superior iliac spine
INTRODUCTION
Transsacral nerve block through sacral foramen is a common procedure for patients complaining of low back pain with radiating pain, and it is mostly performed through the first sacral foramen (S1 foramen) [
1].
With regard to the first sacral nerve root block (S1NRB), the previously suggested method of locating the needle entry point begins with identifying the posterior superior iliac spine (PSIS) and the sacral cornu on the ipsilateral side [
2]. Then a line is drawn between two points, one of which is 1.5 cm medial to the PSIS, and the other of which is 1.5 cm lateral and cephalad to the ipsilateral cornu. After that, one point on the line, which is 1.5 cm cephalad to the level of the PSIS, is considered as the needle entry point. Finally, the block needle is introduced until it penetrates the posterior foramen to the transsacral canal. Although this method has the advantage of being performed without the fluoroscopic device, it has a high possibility of failure because the S1 foramen has a variety of locations, which vary from person to person, and there is considerable pain and discomfort upon needle insertion. To solve these technical difficulties, other methods like using a computed tomography (CT) or magnetic resonance imaging (MRI) are being introduced [
3,
4]. However, since one of the most available imaging aids is the C-arm fluoroscope, S1NRB is used in most cases with the C-arm.
This study aims to analyze distances and directions between the needle entry point on the skin during C-arm guided S1NRB and palpated PSIS. Our results will then be compared to those previously published.
Go to :

MATERIALS AND METHODS
After informed consent was obtained, in the pain center of our hospital from April to August in 2007 fifty patients undergoing C-arm guided S1NRB were enrolled in this study. The following four groups of patients were excluded from this study:
Patients who have a history of spinal operations
Patients who had a serious compression fracture of the spine
Patients whose PSIS was difficult to find because of excessive obesity
Patients whose S1 foramen was not noticeable on radiographs
The patient was placed in a prone position with a pillow (8 cm in height) under the lower abdomen to reduce lumbar lordosis. The same physician was expected to find the PSIS on the surface of the iliac bone and mark the midpoint. The site of entry is visualized by adjusting the fluoroscopic beam to align the posterior foramen with the anterior foramen by rotating the C-arm cephalad and slightly laterally. From this point, a 22-gauge, 60-mm disposable nerve block needle (K-3 Lancet point, Unisis Corp., Tokyo, Japan) was inserted to have a tunnel view [
5]. The proper depth of the block needle was predicted in the lateral radiograph and, finally, the accuracy of needle placement was ensured by fluoroscopic visualization after injecting Omnipaque (Amersham Health, Cork, Ireland).
The distance from the PSIS to the needle entry point was measured horizontally (medially) and vertically (cranially or caudally) (
Fig. 1). SPSS version 13.0 (SPSS Inc. Chicago, IL, USA) was used for statistical analysis, and the sum and subtraction of the mean and standard deviation were described. Comparisons between male and female were done by independent sample t-test, and a
P value of < 0.05 was considered statistically significant.
 | Fig. 1This figure shows the measurements in this study. A represents the transverse distance between the posterior superior iliac spine by palpation and the needle entry point during C-arm guided S1 nerve root block. B represents the vertical distance between the PSIS by palpation and the needle entry point during C-arm guided S1 nerve root block. 
|
Go to :

RESULTS
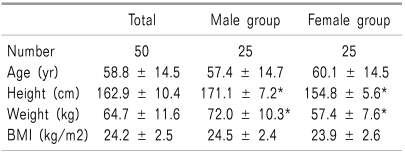
Age, height, and weight of patients are shown in
Table 1. Age and BMI (Body Mass Index) between male and female patients did not differ significantly, but height and weight differed significantly between the two groups (
P < 0.05). The midpoint of the PSIS was designated as 0 on both the x- and y-axis, and the range of the S1 foramen was distributed as indicated in
Fig. 2.
 | Fig. 2The distribution of the needle entry point during C-arm guided S1 nerve root block from the posterior superior iliac spine by palpation. *Represents duplicated data (male and female each). 
|
Table 1
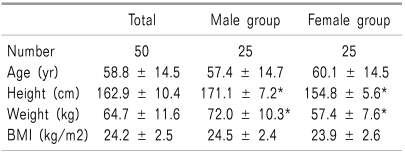

The position of the block needle through the S1 foramen was at the point which is horizontally (medially) average 28.7 ± 8.8 mm and vertically (caudally) average 3.5 ± 14.0 mm from the PSIS in all study participants. There were 18 cases (Male:Female, 11:7) where the block needle position was located in the cranial direction from the PSIS, 3 cases (Male:Female, 2:1) where the block needle position was located on the same line with the PSIS and 29 cases (Male:Female, 12:17) the block needle was located in the caudal direction from the PSIS. It was concluded that the location of the block needle through the S1 foramen was on the same line or in the caudal direction in a considerable number of cases.
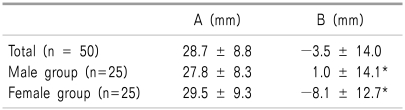
Comparison of average according to gender is shown in
Table 2. In male patients, needle location through the S1 foramen was at the point horizontally (medially) average 27.8 ± 8.3 mm and vertically (cranially) average 1.0 ± 14.1 mm from the PSIS. In female patients, this point was horizontally (medially) average 29.5 ± 9.3 mm and vertically (caudally) average 8.1 ± 12.7 mm from the PSIS.
Table 2
Surface Anatomical Relationships between the Posterior Superior Iliac Spine (PSIS) by Palpation and the Needle Entry Point during C-arm Guided S1 Nerve Root Block
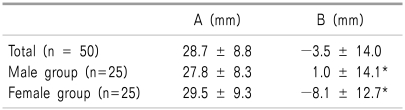

The horizontal distance from the PSIS to the block needle through the S1 foramen did not significantly differ between male and female (P = 0.514), but the female S1 foramen was located more medially from the PSIS compared to male. In contrast, the vertical distance from the PSIS to the block needle through the S1 foramen significantly differed between genders (P = 0.02), and the female S1 foramen was located more caudally from the PSIS compared to male.
Go to :

DISCUSSION
In general, a nerve root block is performed to diagnose and treat pain in patients suffering from low back pain with radiating pain. In the extraforaminal approach, a needle is inserted and advanced into the intervertebral foramen. The ideal location of the needle tip is just caudal to the pedicle and lateral to the line connecting the centers of the pedicles. At this point, the patient may experience a sciatic pain.
It is usually explained that blind transsacral nerve block, which is performed without radiation imaging equipment, is performed after the palpation of the PSIS. In the nerve block, a physician presses a certain point from the PSIS, designating it as a reference point. Subsequently, the physician tries inserting a needle into the sacral foramen. This method is usually performed to outpatients at a pain clinic. This is accomplished by feeling the needle entry and observing patients who complain of radiating pain at a certain entry point [
2]. However, previous data or reference on blind transsacral nerve block is unclear, and this technique is performed in different ways, according to hands-on experience. It is also important to perform this procedure safely by decreasing the frequency of needle injection in order to avoid risk of nerve root damage and arterial bleeding.
The relation between the location of the S1 foramen and the PSIS differs in published literature. Some reports claim that the location of S1 foramen begins with identifying the PSIS. Then a needle entry point can be measured by drawing a line between two points, one of which is 1.5 cm away in a medial direction from the PSIS, and the other of which is 1.5 cm away in a lateral and cranial direction coming from the ipsilateral sacral cornu. After that, one point on the line 1.5 cm away from the PSIS in the cranial direction was expected as a needle entry point [
2]. It was also reported that the dorsal S1 foramen was at the point on the medial line about 1 cm away from the PSIS [
6]. According to Hansan [
7], the S1 foramen exists in the position which is laterally 2.5 ± 0.2 cm and cranially 3.5 ± 0.4 cm for male and 3.1 ± 0.5 cm for female from the midpoint of the line which connects both PSISs.
From previous studies, it is known that the S1 foramen is located cranially from the PSIS. However, this study shows that the S1 foramen of a considerable number of patients is located caudally from PSIS. Unfortunately, it's difficult to explain why this disparity occurs because the evidence supporting previous studies is insufficient. Our results may differ from others for a few reasons. Hansan's study was based on an autopsy, but we used C-arm guided nerve root block and palpated PSIS in patients. There were also fewer participants in Hansan's study. Therefore, to some degree, previously known methods of predicting the location of the S1 foramen are more likely to fail to find it.
In reference to the PSIS, the location of the S1 foramen was located more medially and caudally in female than in male in our study. From existing data, it is known that the sacrum of female is wider and shorter than that of male [
8]. According to a recent study [
9], the width of the sacrum of female was about 0.6 cm wider than that of male. The width of the sacrum for male was 10.2 ± 0.7 cm and 10.8 ± 0.6 cm for female. However, according to Asher's study [
10], the distance between the S1 foramen was narrower in female than in male (47.4 ± 3.8 mm and 48.8 ± 5.0 mm, respectively), corresponding to the result that female S1 foramen is closer to the medial direction in our study.
This study showed that the horizontal (medial) locations of the S1 foramen from the PSIS were 27.8 ± 8.3 mm for male and 29.5 ± 9.3 mm for female, with smaller standard deviations than the vertical locations. However, vertical locations of the S1 foramen from the PSIS were 1.0 ± 14.1 mm for male and -8.1 ± 12.7 mm for female, with a larger standard deviation in comparison to the horizontal locations. This result implies that the horizontal location of the S1 foramen is easy to predict because of a small standard deviation, but its vertical location is hard to predict anatomically because of the large standard deviation.
There are a few limitations in this study. The angle made by the needle entry point on the skin and the needle entering the S1 foramen needs further consideration. Another consideration is the angles and locations of radiation imaging equipment. There is also the issue of anatomical differences in the S1 foramen according to gender, age, and obesity, as well as reliability of accurately locating the PSIS. All of these variables could have affected our results.
We conclude that the S1 foramen is located in a medial direction from the PSIS, with a considerable number of cases showing the S1 foramen is on the same line or in the caudal direction from the PSIS, contradicting previous reports. Therefore previous recommended methods cannot be applied to many cases.
Go to :

ACKNOWLEDGMENTS
The authors are grateful to Dong-Su Jang, (Medical Illustrator, Medical Research Support Section, Yonsei University College of Medicine, Seoul, Korea) for his help with the figures.
Go to :

References
1. Wolff AP, Groen GJ, Crul BJ. Diagnostic lumbosacral segmental nerve blocks with local anesthetics: a prospective double-blind study on the variability and interpretation of segmental effects. Reg Anesth Pain Med. 2001; 26:147–155. PMID:
11251139.

2. Buckley FP. Loeser JD, Butler SH, Chapman CR, Turk DC, editors. Regional anesthesia with local anesthetics. Bonica's management of pain. 2000. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;p. 1924.
3. Ojala R, Vahala E, Karppinen J, Klemola R, Blanco-Sequeiros R, Vaara T, et al. Nerve root infiltration of the first sacral root with MRI guidance. J Magn Reson Imaging. 2000; 12:556–561. PMID:
11042636.

4. Quinn SF, Murtagh FR, Chatfield R, Kori SH. CT-guided nerve root block and ablation. AJR Am J Roentgenol. 1988; 151:1213–1216. PMID:
3263774.

5. Finch PM, Taylor JM. Waldman SD, Winnie AP, editors. Functional anatomy of the spine. Interventional pain management. 1996. Philadelphia: WB Saunders;p. 39–64.
6. Phillip OB, Denise JW. Michael JC, Phillip OB, editors. The lower extremity: Somatic blockade. Neural blockade in clinical anesthesia and management of pain. 1998. 3rd ed. Philadelphia: Lippincott-Raven;p. 377–378.
7. Hasan ST, Shanahan DA, Pridie AK, Neal DE. Surface localization of sacral foramina for neuromodulation of bladder function. An anatomical study. Eur Urol. 1996; 29:90–98. PMID:
8821698.

8. Cheng JS, Song JK. Anatomy of the sacrum. Neurosurg Focus. 2003; 15:E3. PMID:
15350034.

9. Başaloğlu H, Turgut M, Taşer FA, Ceylan T, Başaloğlu HK, Ceylan AA. Morphometry of the sacrum for clinical use. Surg Radiol Anat. 2005; 27:467–471. PMID:
16211321.

10. Asher MA, Strippgen WE. Anthropometric studies of the human sacrum relating to dorsal transsacral implant designs. Clin Orthop Relat Res. 1986; 203:58–62. PMID:
3955998.

Go to :






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download