A fifty-year-old, female patient underwent a severe pain at the cervical part and the left upper extremity from 1 day before her visit to the hospital and MRI was carried out. However, since the patient continuously moved due to the severe pain, the imaging was stopped after only the image of a part of the sagittal plane was taken. It was decided that the MRI should be carried out after pain control, and the patient was sent to the department of pain medicine. By the visual analogue scale, the pain was evaluated to be level 3 at the neck and level 9-10, which was very severe, at the left upper extremity. The Spurling sign was positive (+) and mild muscular weakness was found. It was decided to perform an epidural nerve block in order to control the pain. Under the C-arm guidance, the epidural nerve block was tried in the sitting position. The epidural space was found by the loss-of-resistance technique with air and 0.5 ml of a contrast material was injected to confirm the epidural space. Then, 2.5 ml of the contrast material was injected additionally and its diffusion to the C2-C3 position was verified. After that, 0.75% lidocaine 3 ml was injected and the epidural nerve block was carried out. For 1 hour following the nerve block, EKG, SpO2, blood pressure, and consciousness of the patient were monitored. The MRI was resumed since the pain was reduced to the degree where the patient was able to take the supine position for more than 10 minutes. In the T2 image of the sagittal plane that was taken for the second time, the C3-C4 and C5-C6 herniated disc were suspected (
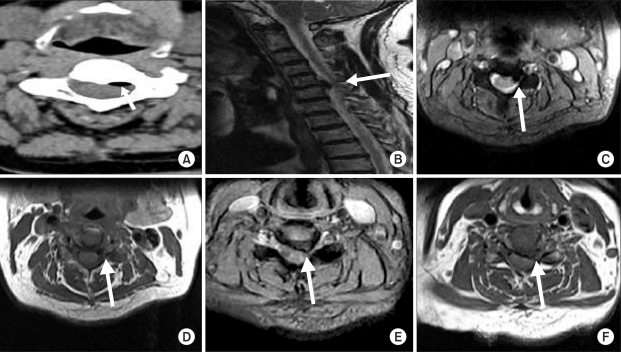
Fig. 1). However, the C3-C4 lesion which was suspected as the herniated disc was considered to be an air shadow in the CT cross-sectional image that was taken for the operation (
Fig. 2A). The T2 image of the sagittal plane that was partially taken before the nerve block was compared in order to identify the lesion, and the result showed that it was a new shadow that had not existed before the nerve block procedure (
Fig. 2B). Nerve root compression was found at the left C6 in the electromyogram that had been performed in advance, but no C3-C4 herniated disc was found before the nerve block. The shadow looked as if it was by air in the CT image and the shadow in the C3-C4 intervertebral space (
Fig. 2C, D) was different from the shadow of the C5-C6 herniated disc in the T1 and T2 cross-sectional images (
Fig. 2E, F). Therefore, we concluded that the shadow was an artifact by air and decided to carry out only the operation for the C5-C6 herniated disc. The patient underwent a C5-C6 anterior cervical discectomy and fusion (ACDF) during the next day and received an MRI 2 days after the operation. No air shadow was found in the C3-C4 intervertebral space in the postoperative MRI (
Fig. 3). The pain of the patient was greatly reduced so that the visual analogue scale could be 0 to 1 on the 8th day after the operation and thus the patient was discharged.
 | Fig. 1T2 sagittal image after cervical epidural block shows low signal intensity lesion at C3-C4 and C5-C6. These lesion are considered herniated disc. 
|
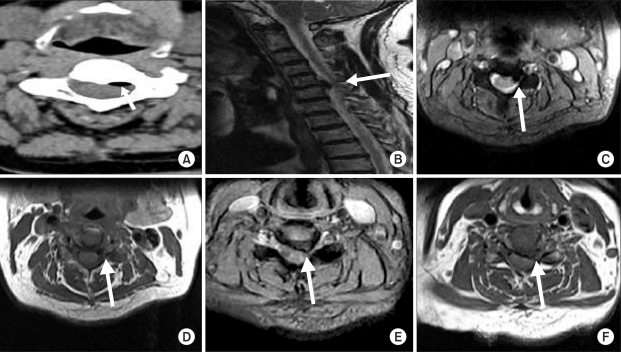 | Fig. 2CT axial image (A) shows low density lesion behind C3-C4 disc. At CT, it seems like the air, not herniated disc. Low signal intensity lesion behind C3-C4 disc seems new compared MRIs before and after cervical epidural block. There is no lesion behind C3-C4 disc in MRI before cervical epidural block (B). (C) and (D) show air as a low signal intensity. By contrast, (E) and (F) show C5-C6 herniated disc relatively higher intensity than lesion behind C3-C4. 
|
 | Fig. 3Post-op. T2 sagittal image. There is no air behind C3-C4 disc. 
|





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download