1. Backonja MM. Defining neuropathic pain. Anesth Analg. 2003; 97:785–790. PMID:
12933403.

2. Barkin RL, Barkin SJ, Barkin DS. Perception, assessment, treatment, and management of pain in the elderly. Clin Geriatr Med. 2005; 21:465–490. PMID:
15911202.

3. Wallace JM. Update on pharmacotherapy guidelines for treatment of neuropathic pain. Curr Pain Headache Rep. 2007; 11:208–214. PMID:
17504648.

4. Watkins LR, Milligan ED, Maier SF. Glial activation: a driving force for pathological pain. Trends Neurosci. 2001; 24:450–455. PMID:
11476884.

5. White FA, Jung H, Miller RJ. Chemokines and the pathophysiology of neuropathic pain. Proc Natl Acad Sci USA. 2007; 104:20151–20158. PMID:
18083844.

6. Bennett GJ. A neuroimmune interaction in painful peripheral neuropathy. Clin J Pain. 2000; 16(3 Suppl):S139–S143. PMID:
11014458.

7. Laffitte E, Revuz J. Thalidomide: an old drug with new clinical applications. Expert Opin Drug Saf. 2004; 3:47–56. PMID:
14680461.

8. Teo SK, Stirling DI, Zeldis JB. Thalidomide as a novel therapeutic agent: new uses for an old product. Drug Discov Today. 2005; 10:107–114. PMID:
15718159.

9. Laffitte E. The revival of thalidomide: an old drug with new indications. Rev Prat. 2006; 56:1977–1983. PMID:
17274497.
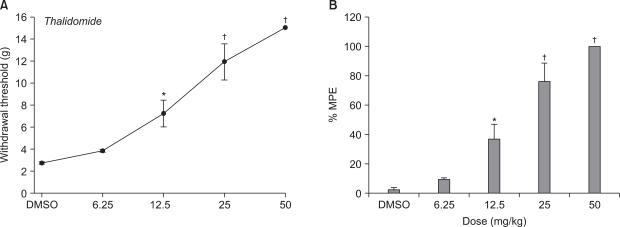
10. Ribeiro RA, Vale ML, Ferreira SH, Cunha FQ. Analgesic effect of thalidomide on inflammatory pain. Eur J Pharmacol. 2000; 391:97–103. PMID:
10720640.

11. Rocha AC, Fernandes ES, Quintão NL, Campos MM, Calixto JB. Relevance of tumour necrosis factor-alpha for the inflammatory and nociceptive responses evoked by carrageenan in the mouse paw. Br J Pharmacol. 2006; 148:688–695. PMID:
16702985.

12. George A, Marziniak M, Schäfers M, Toyka KV, Sommer C. Thalidomide treatment in chronic constrictive neuropathy decreases endoneurial tumor necrosis factor-alpha, increases interleukin-10 and has long-term effects on spinal cord dorsal horn met-enkephalin. Pain. 2000; 88:267–275. PMID:
11068114.

13. Xu JT, Xin WJ, Zang Y, Wu CY, Liu XG. The role of tumor necrosis factor-alpha in the neuropathic pain induced by Lumbar 5 ventral root transection in rat. Pain. 2006; 123:306–321. PMID:
16675114.

14. Rajkumar SV, Fonseca R, Witzig TE. Complete resolution of reflex sympathetic dystrophy with thalidomide treatment. Arch Intern Med. 2001; 161:2502–2503. PMID:
11700165.

15. Ching DW, McClintock A, Beswick F. Successful treatment with low-dose thalidomide in a patient with both Behçet's disease and complex regional pain syndrome type I: case report. J Clin Rheumatol. 2003; 9:96–98. PMID:
17041438.

16. Arnér S, Meyerson BA. Lack of analgesic effect of opioids on neuropathic and idiopathic forms of pain. Pain. 1988; 33:11–23. PMID:
2454440.

17. Dellemijn P. Are opioids effective in relieving neuropathic pain? Pain. 1999; 80:453–462. PMID:
10342407.

18. Gimbel JS, Richards P, Portenoy RK. Controlled-release oxycodone for pain in diabetic neuropathy: a randomized controlled trial. Neurology. 2003; 60:927–934. PMID:
12654955.

19. Raja SN, Haythornthwaite JA, Pappagallo M, Clark MR, Travison TG, Sabeen S, et al. Opioids versus antidepressants in postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 2002; 59:1015–1021. PMID:
12370455.

20. Zimmermann M. Ethical guidelines for investigations on experimental pain in conscious animals. Pain. 1983; 16:109–110. PMID:
6877845.

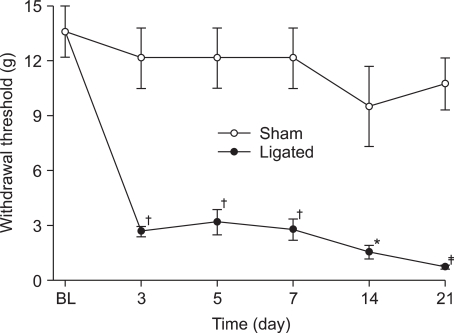
21. Kim SH, Chung JM. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain. 1992; 50:355–363. PMID:
1333581.

22. Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994; 53:55–63. PMID:
7990513.

23. DeLeo JA, Yezierski RP. The role of neuroinflammation and neuroimmune activation in persistent pain. Pain. 2001; 90:1–6. PMID:
11166964.

24. Myers RR, Campana WM, Shubayev VI. The role of neuroinflammation in neuropathic pain: mechanisms and therapeutic targets. Drug Discov Today. 2006; 11:8–20. PMID:
16478686.

25. Sampaio EP, Sarno EN, Galilly R, Cohn ZA, Kaplan G. Thalidomide selectively inhibits tumor necrosis factor alpha production by stimulated human monocytes. J Exp Med. 1991; 173:699–703. PMID:
1997652.

26. Moreira AL, Sampaio EP, Zmuidzinas A, Frindt P, Smith KA, Kaplan G. Thalidomide exerts its inhibitory action on tumor necrosis factor alpha by enhancing mRNA degradation. J Exp Med. 1993; 177:1675–1680. PMID:
8496685.

27. Turk BE, Jiang H, Liu JO. Binding of thalidomide to alpha1-acid glycoprotein may be involved in its inhibition of tumor necrosis factor alpha production. Proc Natl Acad Sci USA. 1996; 93:7552–7556. PMID:
8755512.

28. Vale ML, Cunha FQ, Brito GA, Benevides VM, Ferreira SH, Poole S, et al. Anti-nociceptive effect of thalidomide on zymosan-induced experimental articular incapacitation. Eur J Pharmacol. 2006; 536:309–317. PMID:
16597438.

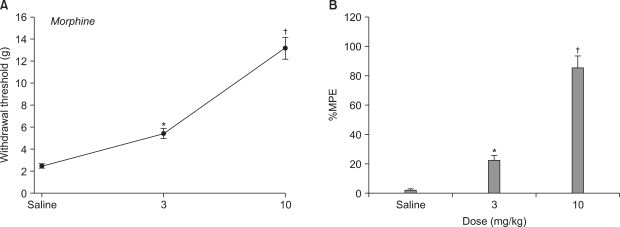
29. Bian D, Nichols ML, Ossipov MH, Lai J, Porreca F. Characterization of the antiallodynic efficacy of morphine in a model of neuropathic pain in rats. Neuroreport. 1995; 6:1981–1984. PMID:
8580422.

30. Lee YW, Chaplan SR, Yaksh TL. Systemic and supraspinal, but not spinal, opiates suppress allodynia in a rat neuropathic pain model. Neurosci Lett. 1995; 199:111–114. PMID:
8584236.

31. Ossipov MH, Lopez Y, Nichols ML, Bian D, Porreca F. Inhibition by spinal morphine of the tail-flick response is attenuated in rats with nerve ligation injury. Neurosci Lett. 1995; 199:83–86. PMID:
8584249.

32. Yu W, Hao JX, Xu XJ, Wiesenfeld-Hallin Z. Comparison of the anti-allodynic and antinociceptive effects of systemic; intrathecal and intracerebroventricular morphine in a rat model of central neuropathic pain. Eur J Pain. 1997; 1:17–29. PMID:
15102425.

33. Zhao C, Tall JM, Meyer RA, Raja SN. Antiallodynic effects of systemic and intrathecal morphine in the spared nerve injury model of neuropathic pain in rats. Anesthesiology. 2004; 100:905–911. PMID:
15087626.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download