This article has been
cited by other articles in ScienceCentral.
Abstract
Occipital neuralgia is a form of headache that involves the posterior occiput in the greater or lesser occipital nerve distribution. Pain can be severe and persistent with conservative treatment. We present a case of intractable occipital neuralgia that conventional therapeutic modalities failed to ameliorate. We speculate that, in this case, the cause of headache could be the greater occipital nerve entrapment by the obliquus capitis inferior muscle. After steroid and local anesthetic injection into obliquus capitis inferior muscles under fluoroscopic and sonographic guidance, the visual analogue scale was decreased from 9-10/10 to 1-2/10 for 2-3 weeks. The patient eventually got both greater occipital neurectomy and partial resection of obliquus capitis inferior muscles due to the short term effect of the injection. The successful steroid and local anesthetic injection for this occipital neuralgia shows that the refractory headache was caused by entrapment of greater occipital nerves by obliquus capitis inferior muscles.
Go to :

Keywords: greater occipital nerve, obliquus capitis inferior muscle, occipital neuralgia
Occipital neuralgia refers to a specific headache, such as a chronic, piercing pain similar to electric shock or pulsation that occurs in the neck area, cephalic area, and back of the ear. The areas where the pain appears are in connection with the track area of the greater occipital nerve and lesser occipital nerve and above nerves run from spine towards back head.
Occipital neuralgia may be caused by an anatomical pathological process that occurs in connection with nerve roots of the upper cervical spine [
1] and may rarely be caused by dural arterio-venous fistula of spine head joints [
2], cavernous angioma of hindbrain [
3], tumor [
4,
5], and herpes zoster virus infection [
6-
9].
With the basis of symptoms from patients who suffer from occipital neuralgia that does not respond to any other treatment, physical examination, and diagnostic radiographic inspection findings, the authors doubted of greater occipital nerve entrapment of obliquus capitis inferior. We, thereby, present this case as a patient's pain that has been relieved by the blocking of the obliquus capitis inferior muscle using local anesthetic and steroid under sonographic guidance and a C-arm type television image intensification system.
CASE REPORT
A 56-year-old male patient visited the hospital due to a consistent cervical headache that intensifies convulsively. This headache has been occurring in a frequency of once in 6 months beginning 7 years ago; however, 5 years ago, an intense occipital neuralgia occurred after the patient struggled while carrying a heavy object with his head. The condition of occipital neuralgia then was the sense of being squashed constantly. The areas of pain stayed in the fronto-occipital and back neck regions, and the pain was most severe in both sides of the lower margin of the inferior obliquus capitis muscle. When the head was tilted back, he felt the pain lessened slightly and when the head was bent, the pain increased. When the patient moved around, the headache worsened and when the patient laid on the back, the pain was reduced. The pain lasted for 3 days or once in a week then, yet, a year ago, before the patient's initial visit to the hospital, pain occurred almost consistently. When the headache worsened, it lasted from 24 hours to 48 hours and the visual analogue scale (VAS) was then approximately 10/10. When the pain was intense, the patient was not able to eat, could not sleep all night, and consistently vomited. After the occurrence of such symptoms, a radiographic examination and neurological examination, including magnetic resonance imaging of the cervical spine region and cephalic, were executed in other hospitals, yet there was no specific findings that could determine the cause of the pain.
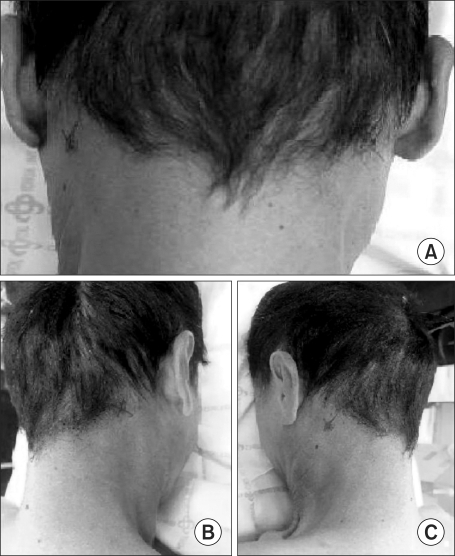
In the simple cervical spine radiography and magnetic resonance imaging examination that was executed under the the Department of Neurology and Department of Rehabilitation and Neurosurgery's presumptive diagnosis of myofacial pain syndrome, cervical herniation of intervertebral disc, tension headache, occipital neuralgia, there were no specific findings except for cervical 5-6 protrusion disc, left 4-5, 5-6, 6-7 cervical uncovertebral joint hypertrophy, and minimal foraminal stenosis for left 4-5, 5-6, 6-7 cervical. As there was no improvement in the symptoms with the oral administration of benzodiazepine and ergotamine, under the Department of Neurology and Department of Rehabilitation's diagnosis of tension headache and migraine, the patient was referred to a pain clinic. Inferred from a physical examination executed in the pain clinic and symptoms of the patient (
Fig. 1), diagnostic greater occipital nerve blockage of both sides, utilizing local anesthetic, was executed. After drawing an imaginary line that connects to the external occipital protuberance to the mastoid process of the patient, in a position where the patient was laid in a prone position, a drug was injected in the greater occipital nerve that passes medial occipital artery in medial 1/3 point. After blocking the nerve, there was an improvement in the symptoms by 10-20% of the Symptom Relief Scale, which lasted for approximately 2 to 3 days. Thereafter, though pulsed Radiofrequency ablation followed by C2 ganglion block was executed, 10-20% maintained as the symptom improvement. In consideration that the patient generally complains of his pain as being located in the lower margin of the inferior obliquus capitis muscle among track areas of the greater occipital nerve, a drug was injected in the inferior obliquus capitis muscle through a C-arm television image intensification system utilizing a local anesthetic and triamcinolone (
Fig. 2). After sanitizing the posterior cervical, the treatment area, as well as its surrounding skin, with betadin, when the patient was laid in a prone position, location of each C2 spinous process and C1 transverse process was verified in anterior-posterior view and lateral view through C-arm fluoroscopy. In order to avoid injury of the vertebral artery and spinal cord, it was processed with a needle in the lateral medial border of the C2 vertebral arch as an injection point. After locating the middle part of the C1 transverse process and C2 spinous process with contrast material on the side, the drug was injected. After such treatment, the patient's pain was reduced from VAS 10 to 0-1 in the first week and up to 1-2 in the 2
nd week, yet thereafter, the pain reoccurred, which went up to VAS 10. To treat, blockage of inferior obliquus capitis muscle was executed under sonographic guidance (
Fig. 3). The treatment was executed in a condition where the patient was laid in a prone position and a sonographic searcher was placed in the middle line of occiput, which made the long axis sections visible; furthermore, the C1 and C2 spinous process were verified, and by moving the researcher laterally, the C1 transverse process was verified. After verifying the inferior obliquus capitis muscle that traverses the C2 spinous process and C1 transverse process with sonograph a drug was injected. After the treatment, pain was controlled to a state where VAS 1-2 was maintained for more than 3 weeks. The patient was satisfied with the reduction in pain but commented on difficulty of possibility in its recurrence after 3 months when medical treatment and botox injection treatment done in 3 to 4 week intervals are executed. Therefore, after discussion with Neurosurgery, resection for both sides of greater occipital neurectomy and partial resection of the obliquus capitis inferior muscle were executed (
Fig. 4,
5), and according to its follow up for 2 months, there was nearly no pain on the visual analogue scale, which was 0-1/10 in everyday life, exercise, and work.
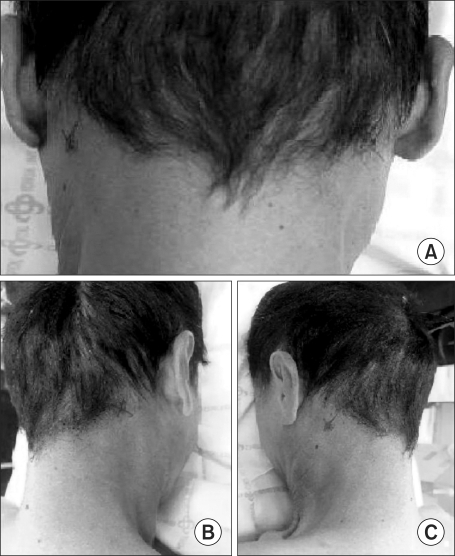 | Fig. 1The area about which the patient complains. (A) We can see both Xs of the patient's posterior neck. (B) Right aspect of posterior neck. (C) Left aspect of posterior neck. 
|
 | Fig. 2Fluoroscopic imaging. Lateral view (A) and anterio-posterior view (B) show spinal needle placement adjacent to the obliquus capitis inferior muscle. 
|
 | Fig. 3Long axis view - ultrasonographic image of injection in the obliquus capitis inferior muscle. Probe was placed in the midline between spinous process of the axis and left transverse process of the first cervical vertebrae. The arrow shows needle placement in the left obliquus capitis inferior muscle. a: spinous process of 1st cervical vertebrae, b: spinous process of 2nd cervical vertebrae. 
|
 | Fig. 4Intraoperative picture. The arrow indicates the left obliquus capitis inferior muscle removed during operation. 
|
 | Fig. 5The pathologic finding of the greater occipital nerve. Degenerated peripheral nerve trunk with axonal swelling and myelin digestion chambers. 
|
Go to :

DISCUSSION
Occipital neuralgia may be defined as a combination of symptoms that occur according to track area of the laryngeal nerve. The causes of such occipital neuralgia are stimulus of the greater occipital nerve origin due to inflammation of C1-C2 nerve ganglion [
10], entrapment of the greater occipital nerve as per muscles and aponeurosis that could be passed in the track path of the greater occipital nerve, or as per entrapment of the greater occipital nerve by muscles around the occiput [
11]. Local inflammation or infection, gout, diabetes, vascular inflammation and the state of the head consistently in anteroinferior directions may also have connections to occurrence of occipital neuralgia.
The greater occipital nerve, which is the main cause of such occipital neuralgia, starts in between the atlas and axis, comes down laterally, and rises up by coiling toward the lower margin of the inferior obliquus capitis muscle. It goes up tilted in upper medial among the inferior obliquus capitis muscle, rectus capitis posterior, and semispinalis, and it goes through the semispinalis and trapezius [
12]. The greater occipital nerve is responsible for the sense of skin in the upper side of the neck and occiput.
The greater occipital nerve is weak in entrapment by muscles that exist in the upper side of the back of the neck and craniobasal. Especially, location where entrapment or stimulation by muscle easily occurs, may be stated as a C2 dorsal branch in between the atlas and axis [
10,
13], inferior obliquus capitis muscle, and semispinalis that meet in the track path of the greater occipital nerve and the aponeurosis area of the trapezius muscle that the greater occipital nerve goes through. So to speak, it can be entrapped by muscles that are adjacent or that pass through according to the track path. Especially, the inferior obliquus capitis muscle, which is estimated as the cause of occipital neuralgia as for the patient of this case, is originated from the spinous process of the axis, attaches to the spinous process of the atlas and is responsible for the rotation function of the median atlantoaxial joint.
The patient of this case has been working for decades as a shoemaker, which involves working with his head bent and through this, there was presumably tension of the posterior neck muscle, especially chronic tension in the inferior obliquus capitis muscle.
Piriformis syndrome, a representative muscle entrapment syndrome, is secreted with inflammatory substances, such as prostaglandins, histamine, bradykinin, and serotonin from the inflamed muscle, and these stimulate the sciatic nerve, which results in a cycle of pain-fibrillation-inflammation-stimulation [
14,
15]. Cases that are similar to the above, such as inflammatory substances caused due to friction of the inferior obliquus capitis muscle and greater occipital nerve throughout decades, are thought to contribute to the cause of the pain about which the patient complained.
Diagnosis of occipital neuralgia can be determined when damage of nerve roots or the greater occipital nerve, or disease are considered as causes of the symptom [
16]. Nerve block using local anesthetic is one of the diagnostic methods and medication methods of occipital neuralgia that can be executed most easily and quickly [
17].
Since the patient complained of area where the inferior obliquus capitis muscle was met among the track areas of the greater occipital nerve as being the most painful area, the inferior obliquus capitis muscle was blocked using a local anesthetic and steroid under the C-arm television image intensification system. After such treatment, the patient's pain, which had originally been estimated in VAS as 10/10, was reduced in the 1st week to 1/10 and in the 2nd week to 1-2/10. Blockage of the inferior obliquus capitis muscle, in a later stage, was executed in sonographic guidance, as that avoids the hassle of going into an operation room and does not raise concern in radiation exposure. This, as well, led to pain reduction and duration in a similar aspect. The patient was satisfied with the reduction in pain, yet complained of difficulty in the possibility of its reoccurrence after 3 months when medication and botox injection treatment done every 3-5 week intervals are executed. Therefore, after discussion with the hospital's the Neurosurgery Department, resection of both greater occipital neurectomy and partial resection of the obliquus capitis inferior muscle were executed.
The fact that anatomical pathological lesions of the inferior obliquus capitis muscle or greater occipital nerve, which are estimated to be causes of the symptoms, cannot be verified is the limitation on the thesis of this case. There was a limitation in estimating anatomical variations with magnetic resonance imaging executed upon the patient Muscle lesions have a big difference as per individuals, and there are many cases that both muscles are compared as diagnosed; however, it was difficult to compare in this case, as the patient complained of headache on both sides. To alleviate this problem, positron emission tomography-computed tomography (PET/CT), which can clearly display changes in physiological chemical metabolism, has been considered, and researchers, including Sung [
18], announced that in terms of botox treatment for patients with idiopathic cervical muscle strain, PET/CT can potentially be helpful in recognizing the muscles that have myodystonia. However, its execution in this case was not feasible, as the hospital was not equipped with PET/CT and the patient was unable to afford it due to his economic situation.
Though there were diverse limitations, as there was an improvement in symptoms in the inferior obliquus capitis muscle blocks for a patient who had occipital neuralgia that previously showed no improvement in any other treatment, surgical treatment was executed. We, thereby, are presenting obliquus capitis muscle block methods under the C-arm television image intensification system and sonographic guidance as a means of alleviating pain in patients who experience occipital neuralgia".
Go to :







 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download