Abstract
Background
An independent medical examination (IME) is a critical process for awarding reparation for injury. However, conducting an IME in pain medicine is very difficult, not only because pain is a subjective symptom, but also because there are no proper objective methods to demonstrate it. This study was conducted to compare IME reports and the court decisions on the disability status of the patients.
Methods
We analyzed 79 IME reports and 25 corresponding court decisions on the disability status of patients. The diagnoses, causal relationships between the patients' status and the trauma, McBride's degree of disability, the American Medical Association's impairment ratings, the estimated annual cost for future treatment, and the necessity of care-giving were compared and analyzed.
Results
The diagnoses in the 79 cases were complex regional pain syndrome (CRPS) type I (58 cases), CRPS type II (7 cases), peripheral neuropathy (5 cases), myofascial pain syndrome (4 cases), herniated intervertebral disc (2 cases), and fibromyalgia (1 case). The types of accidents were road traffic accidents (50 cases), military injuries (14 cases), industrial accidents (11 cases), and others (4 cases). The IME reports and the court decisions stated considerably different McBride's degrees of disability (P = 0.014). However, there was no significant difference in the estimated cost for future treatment between the IME reports and the court decisions (P = 0.912).
Go to : 
Road traffic accidents and industrial accidents can cause a large amount of physical damage and complicate the lives of the victims. More and more reparation laws have been set up and the legal process of determining the degree of impairment requires objectivity, therefore, the court requires independent medical examinations (IMEs) during the lawsuit. Although the pain disorders are not clearly recognized as impairment [1], however, there have been continuous efforts to expand the scope of impairment to include pain [2]. To reflect the current needs, the court's requests for the IME to the physicians have been increased in the area of pain medicine. However, it is difficult to objectify the amount of pain from which patients suffer because the currently available specific tests are limited. Moreover, the issue of pain assessed on the IMEs involves the victim's financial compensation and secondary gain. That is why there so much emphasis has been placed on the accuracy of the physician's IME.
Moreover, in Korea, there is no consensus on a rational standard for IMEs [3]. In pain medicine, IMEs are conducted by individual pain specialists, so there is no uniform guideline to follow and the information on the court decisions on IMEs is not shared. Physicians do not get trained in writing up IME reports, so they do not have a proper understanding of the legal value or legal interpretation of these evaluations.
Therefore, we conducted a comparative study on the IME reports and legal decision in pain medicine to determine how patients with pain are evaluated, and how the evaluations are legally interpreted, with the purpose of this study results to serve as data for future IME evaluations in pain medicine.
Go to : 
After approval from our institute review board, we conducted a comparative study on the IME reports and the court decision from January 2006 to September 2009. Consecutive 79 IMEs (from 3 tertiary hospitals in the Seoul and Gyeonggi area) and 25 court decisions were reviewed. Fifty-four court cases were excluded because they were withdrawn suits, cases where a compromise solution was suggested, and unsettled cases. We got copies of the court decisions from the Supreme Court's homepage (http://www.scourt.go.kr/decide/DecideList.work) and compared them against the corresponding IME copies acquired from their respective hospitals.
The IMEs and court decisions were analyzed for the victim's gender, the age at the time of the injury, the cause for injury, the diagnosis stated in the IMEs, McBride's degree of disability and its categories [4], the American Medical Association's (AMA) impairment ratings [5], the estimated annual cost for future treatment, the estimated duration of the treatment period, the necessity of the implanting spinal cord stimulator (SCS), the necessity of care-giving and the required duration, the necessity for care-giving depending on the diagnosis, and whether the life expectancy decreases.
The statistical analysis was done with the SPSS statistics® ver. 17.0 (SPSS Inc., Chicago, USA). The mean comparisons between the IME reports and corresponding courts decision on the loss of ability to work and cost for future treatment were performed using the paired t-test after checking normality by the Kolmogorov-Smirov test. The Kruskal-Wallis test was performed for comparing the McBride's degree of disability, the AMA impairment ratings, the future annual treatment cost estimation, and the necessity for care-giving according to the diagnoses. The results are expressed as mean ± standard deviation. P values < 0.05 were considered statistically significant.
Go to : 
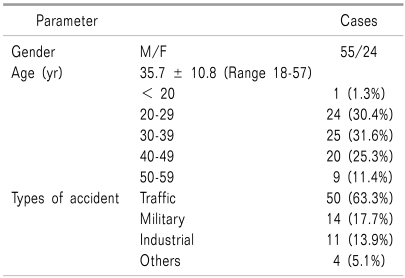
Out of the 79 people assessed, 55 were male and 24 were female. Their ages were 35.7 ± 10.8 (range from 18 to 57) years. There were 50 cases (63.3%) of road traffic accidents, 14 cases (17.7%) were military injuries, 11 cases (13.9%) were work injuries, and 4 cases (5.1%) were miscellaneous (Table 1).
The diagnoses were 58 cases of complex regional pain syndrome (CRPS) type I (73.4%), 7 cases of CRPS type II (8.9%), 5 cases of peripheral neuropathy (6.3%), 4 cases of myofascial pain syndrome (5.1%), 2 cases of herniated intervertebral disc (2.5%), 1 case of fibromyalgia (1.3%) and the diagnoses of remaining 2 cases (2.5%) were unknown.
There were statements on the casual relationship in 43 cases out of the 79 IMEs (54.4%). Among the 43 cases, 3 cases reported that the causal relationship was unclear, 34 cases recognized the causal relationship, but the degree of the causal effects was not definitely stated. Only 6 cases concretely stated the degree of the causal effects of the accident, of which 4 cases stated that the trauma was 100% due to the accident. In 2 cases of IMEs, the trauma was 30% and 70% attributed to the accident due to the pre-existing conditions of the each patient.
In the court decision, only 16 cases out of 25 (64.0%) stated the degree of the causal effects of the accidents, with a mean of 68.8 ± 19.5% (Fig. 1). In case of the patient's status was not totally due to the accident, it was attributed to the effects of pre-existing conditions or the negligence of the injured party. The reasons why the CRPS was not totally due to the accident were 1) CRPS is a rare disease 2) the accidents were negligible, the pain and damage were exaggerated by the patients and 3) it is considered unfair to request full reparation for the CRPS patients from the defending party.
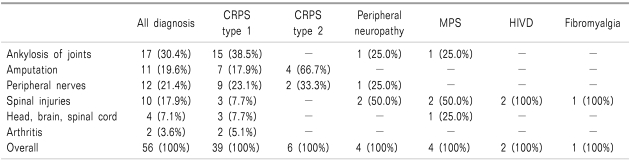
The degree of disability by the McBride System was mentioned in 56 IMEs. In 2 cases, 2 categories of McBride's system were applied together. Out of the 17 categories [4], the applicable categories in the IMEs were 17 cases of ankylosis of joints (30.4%), 11 cases of amputation (19.6%), 12 cases of peripheral nerves (21.4%), 10 cases of spinal injuries (17.9%), 4 cases of head/brain/spinal cord injuries (7.1%) and 2 cases of arthritis (3.6%).
For the CRPS type 1 which was the most frequent diagnosis, the McBride's degree of disability was mentioned in 39 cases, among which the most commonly applied categories were ankylosis joints in 15 cases (38.5%) amputation in 7 cases (17.9%), peripheral nerves in 9 cases (23.1%), spinal injuries in 3 cases (7.7%), head/brain/spinal cord injuries in 3 cases (7.7%) and arthritis in 2 cases (5.1%).
For the cases of CRPS type II, McBride's degree of disability was mentioned in 6 cases; amputation was most commonly applied in 4 of these 6 cases (66.7%), and peripheral nerve injury was applied in 2 of 6 cases (33.3%, Table 2).
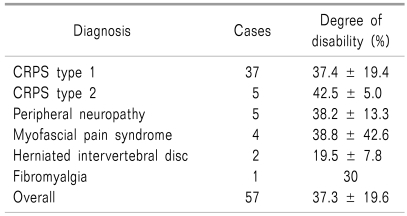
The degree of disability was on average 37.3 ± 19.6% (range from 0 to 100%). There was no significant difference for the degree of disability amongst the diagnoses (P = 0.482, Table 3). There were 19 of the cases where the McBride's degree of disability was mentioned in both the IME and the court decision. The loss of ability to work on the IME and court decisions were on average 40.4 ± 24.0% and 26.1 ± 21.5%, respectively, which showed a significant statistical difference (P = 0.014).
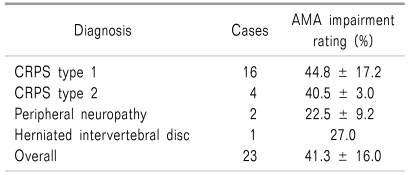
Twenty-three IMEs mentioned the degree of physical disability based on the American Medical Association's (AMA) impairment ratings (29.1%) with the average AMA impairment of 41.3 ± 16.0%. There was no significant difference of the impairment amongst the different diagnoses (P = 0.237, Table 4).
Out of 14 military injuries of soldiers who received trauma in military service and demand special privileges and support by the enforced ordinance, only 12 mentioned the degree of disability in the IME; 6 cases were level 5 (50.0%), 5 cases were level 6 (41.7%) and 1 case was level 7 (8.3%).
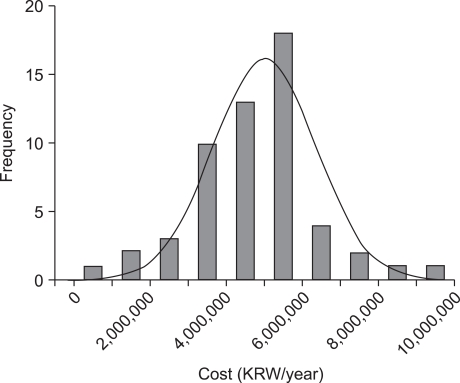
The annual cost for future treatment and the expected duration of treatment were mentioned in 55 IMEs (69.6%). The average amount was 4,805,244 KRW/year (range from 338,480 to 9,093,380 KRW/year (Fig. 2). The expected duration of treatment was mentioned in 47 of the cases (59.5%). 'Life-long treatment' was stated the most frequently for 43 cases. Treatments lasting 1 year, 2 years, 3 years and 5 years were all mentioned once.
We compared the differences in the costs for future treatment for each diagnosis; CRPS type I was 5,083,681 KRW/year, CRPS type II was 4,744,395 KRW/year, peripheral neuropathy was 4,626,000 KRW/year, myofascial pain syndrome was 2,863,403 KRW/year and herniated disc was 2,177,920 KRW/year. The cost differences between the diagnoses were not statistically significantly (P = 0.770).
Court decisions that recognized future treatment costs were around an average of 4,901,786 KRW/year (range from 2,232,832 to 10,072,720 KRW/year), showing no statistical difference with those estimated by the IMEs (P = 0.912).
Before an IME was conducted, 28 cases already had SCS implanted, among which 4 cases of SCS were removed due to no effect. Therefore at the time of IMEs the remaining 24 cases had permanent SCS.
Thirty cases of IMEs stated that there was a need for implanting SCS and 5 cases stated that it was unnecessary.
Despite the anesthesiologist's opinion that there was a need for the implantation of a SCS, the court ruled in 2 cases that it was unnecessary on the basis of the evaluation by a physician from a different field.
Forty-three IMEs mentioned the necessity of care-giving. Twenty-three cases stated that there was no need (53.5%), 2 cases stated that 12 hours/day of care-giving were needed (4.7%), 13 cases stated that 8 hours/day of care-giving were needed (30.2%) and 5 cases stated that 4 hours/day were needed (11.6%). Only 3 cases altogether concretely mentioned the periods of care-giving (only 1 case for 1 year and 2 cases for 3 years). And there was no significant difference for the necessity of care-giving amongst the diagnoses (P = 0.644).
Fifteen court decisions mentioned the necessity of care-giving, among which 9 stated there was no need (60.0%), 3 cases stated 8 hours/day of care-giving were needed (20.0%), 2 stated 4 hours/day were needed (13.3%) and 1 case stated that 2 hours/day of care-giving were needed (6.7%). Only 4 court decisions mentioned the period of care-giving; 2 cases of care-giving for 3 years, 1 case of 400 days of care-giving and then 1 case of care-giving for 3 months.
Forty-nine (62.0%) IMEs stated that no decrease in life expectancy was considered due to pain, and remaining 38% of IME reports did not mention on that subject.
Go to : 
There has been a recent increase in law suits in the field of pain medicine and in the request of IMEs, which is good news that the awareness of the field of pain medicine is increasing. However, pain physicians now must own up to the responsibilities of the attention they are receiving. There have been debates on the objectivity of IMEs due to the physician's lack of understanding of and the gravity of the pain disorders.
The difficulties of writing up an IME report are the following: first, there is a lack of experience in conducting IMEs, the pain evaluation is very dependent on the patient's own complaints of the pain and specific objective test with positive results are rare. Even with the same diagnosis in pain disorder, the severity of pain varies and manifests differently for every patient. As a consequence, it is difficult to clearly distinguish and interpret the patient'sv complaints. Second, the injured party of a road traffic accident stays in the hospital longer than the defendant, and even after the complications and subjective symptoms have been resolved, the injured party stays at the hospital usually 3 times as long as long as the defendant [6]. Therefore, the IME physician must discern the examinee's compensation-related secondary gain as the examinee's interests are tied to the IME results. Third, regulations on the details of IMEs are very limited and the evaluation standards are complicated. That is why there are huge differences in IME reports depending on the IME physician and the IME medical department [3]. Due to the large differences, the courts have difficulties of trusting the IMEs, so sometimes they ask for re-evaluations to many different physicians. During our reviewing the court decision, one court chose one IME report over another because "it made a more objective evaluation of the patient's physical condition, including the calculation of pre-existing conditions attributing to the loss of the ability to work."
Besides the problems stated above, physicians are not taught how to write up an IME report, which makes the process of writing one up difficult in the first place. Because diagnosing and treatment are the main job of physicians, IMEs cause a loss in times and they require a lot of thinking.
The keys points of an IME are 1) the existence of the causal relationship, 2) the degree of disability and 3) the estimation of future treatment cost. These three are important in calculating the reparation cost.
The recognition of the existence of the causal relationship was stated in 43 cases, of which only 6 cases stated the exact degree of causal effects. Another study on the IMEs reported to the court in the field of psychiatry [7] stated the causal relationship between the accident to the injury were concretely stated only in a third of the cases, and this most likely because it was hard to accurately assess the causal relationship. The patient's past medical insurance records can be referenced to determine the relevance of the current symptoms and pre-existing conditions. The casual relationship can then be more accurately assessed with putting aside the patient's pre-existing conditions.
There was a significant difference in the loss of ability to work between the IMEs and the court decisions on McBride's degree of disability. The bases of low estimation on degree of disability by the court decisions were 1) the damage was so small and there was conclusively no recognizable evidence of damage 2) there were no abnormal findings on the on the laboratory test, and the symptoms were very subjective because of psychological damage, and 3) due to pre-existing conditions, the causal relationship between the injury and the symptoms cannot be 100% acknowledged. We must admit that pain cannot be proven by a perfectly objective examination, yet for a pain specialist's opinion to be seriously received in court, pain medicine must be promoted and more objective examinations must be conducted and pre-existing conditions must be more carefully reviewed. In one court decision, the IME physician applied a McBride's occupational grading #6, but it was corrected to #5 by the court because it was "more appropriate". Therefore, when writing up IMEs, clarifying the physician's evaluation on the McBride's categories and the occupational grading will reduce misunderstanding.
For the evaluations of future treatment costs, there was no significant difference in the court estimation from that of the physician's. One fact to note though, is that the court decision on the treatment cost is not based on the equation (annual treatment cost × treatment period), but instead the court uses the Hoffman's calculation system in figuring out the total cost needed. Therefore, the IME physician only needs to figure out the annual treatment cost.
Court decisions differed from each other on the estimation of cost for oral medication and interventional procedures when the battery needs to be changed in the patient with effective implanted SCS. The court recognized 30-100% of the estimated cost for drugs and intervention on IME reports due to the SCS. This percentage shows that further studies and a more concrete basis for proof are needed.
There is no basis for deciding the duration future treatment when it was a certain limited period, so this requires further discuss. As a rule, to receive reparation and compensation, the disability must be permanent. In some circumstances, a temporary disability is applicable, but this is limited to spinal injury and thus temporary disability should not be applied to other injuries [3]. The estimated period for temporary disabilities can be based on arbitrary decisions of the IME physician, so the objectivity and the reenactment of the decisions on the temporary disabilities raise problems.
Other factors to consider are that 30 IMEs (38.0%) required a SCS for improvement of patient's status; however, it appears unreasonable that the rule for calculating the degree of disability should be done after the patient's reaching the state of maximal medical improvement and the stable state of being unable to expect improvement or change [8]. When the examinee needs a SCS for improvement, his disability should be reassessed after the SCS implantation and its effectiveness checked.
IMEs require significant improvement in several aspects. First, the field of pain medicine must specify the basis for IME evaluations. Past IME reports should be compiled, the most standard cases should be listed, and a basis for disabilities should be established. Second, the physicians conducting IMEs should be educated with special training. As of now, there are not many physicians who are educated on or experienced with IMEs. In fact, few medical societies in Korea have provided training programs on conducting IMEs. 'The Korean Pain Society - IME Workshop 2009' was inspirational and such workshops should be continuously hosted in the future. Third, the time and effort put into writing up an IME should be properly compensated [9]. As of now, only a small fee is charged for the physical examination in an IME report, but physicians require a rectification of this system. The current law, (Supreme Court Regulations Concerning the Standard for Appointing an IME Physician and Estimating the Evaluation Cost Rule No.1211) sets the evaluation fee at 200,000-300,000 KRW. However, there is a consensus that this is far too low, and it needs to be increased. Of course, the rule states that "the physician should submit their request for the increase to the court and explain their reason in concrete terms before performing the evaluation when the evaluation cannot be performed under the established fee". So, active usage of this statement should be made. We encourage this, because IME physicians experience mental stress when writing up IMEs. This is partially due to the fact that McBride's degree of disability or the AMA impairment ratings are not simple enough, especially for pain medicine. For example, it is more difficult to determine disability with pain than what percentage of disability would be corresponding to the certain limitation of joint movement. Also, after the IME, courts often request back-checks to confirm the veracity of the evaluation with no compensation for them. Finally, measures to protect physicians should be established. There are cases where the plaintiff or defendant shortcuts the court and makes direct contact with the IME physician inappropriately. In the worst case, they even make physical threats against the physician.
In conclusion, IMEs should be conducted fairly with the maximum objective proof. Specialists in pain medicine should also show more interest in physical examinations and compensation medicine. IME physicians should study the IME reports presented at courts and compare them with the court decisions in order to achieve greater consistency of evaluations and to reduce the differences in opinion on the degree of disability.
Go to : 
References
1. Kim YC. The evaluation of permanent impairment in chronic pain patients. Korean J Pain. 2007; 20:1–7.

2. Jang SH, Rah UW, Kim YC, Park YS, Jo D, Kim YC. Development of Korean academy of medical sciences guideline-rating the impairment in pain. J Korean Med Sci. 2009; 24(Suppl 2):S330–S337. PMID: 19503691.

3. Lee SD, Yi SR. Practical guidelines of physical impairment and disability evaluation. 2005. Seoul: Joongang Moonhwa Co;p. 3–9.
4. McBride ED. Disability evaluation and principles of treatment of compensable injuries. 1963. 6th ed. Philadelphia: JB Lippincott;p. 68–103.
5. Cocchiarella L, Andersson GB. Guides to the evaluation of permanent impairment. 2001. 5th ed. Chicago: American medical association Press;p. 1–16. p. 336–337. p. 343–347. p. 495p. 553p. 565–591.
6. Kim MW, Kim JS, Lim MK. A study on epidemiologic characteristics and factors associated with excess hospitalization of the patients injured by traffic accident. Korean J Epidemiol. 1998; 20:279–287.
7. Park KC, Suh T, Ahn DJ, Kim YC, Rho SH, Jung HY, et al. Analysis of 220 reports for courts by Korean pschiatrists about mental and behavioral disabilities after motor vehicle accidents. Mental Health Research. 2002; 21:14–33.
8. Rondinelli RD. Guides to the evaluation of permanent impairment. 2008. 6th ed. Chicago: American medical association Press;p. 23–24.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download