Abstract
Background
Facet joint have been implicated as a source of chronic low back pain. Radiofrequency denervation has demonstrated the most solid evidence. To increase safety and efficacy of treatment, computed tomography (CT) guidance injection has been used in several disease. The purpose of this study was to evaluate the efficacy of CT-guided radiofrequency rhizotomy in the treatment of facet joint pain.
Methods
A total of 40 patients were randomized to undergo radiofrequency facet joint denervation under CT guidance or C-arm guidance. All patients were examined visual analogue scale (VAS) score before treatment, 1 month, and 3 months after treatment.
The lumbar zygapophyseal joint has been implicated as one of the causes of chronic low back pain. Percutaneous radiofrequency rhizotomy is used to treat chronic facet origin pain. Because imaging-guided techniques should lead to better outcomes and reduced complication rates, imaging-guided procedures are becoming more popular. However, C-arm guidance could be carried a risk of inadvertent damage to the nerve root or other organs in severe anatomic variant patients. A new fluoroscopic computed tomography (CT) guidance technique makes this technique of radiofrequency rhizotomy even easier. To reduce complications and enhance treatment efficacy, CT is commonly used for several procedures. Although many studies have been reported that use a CT guided interventional procedure [1-5], there are few reports of CT-guided lumbar rhizotomy for chronic pain in adults.
The aim of our study was to evaluate the role of CT-guided radiofrequency rhizotomy of the lumbar medical branch in the management of facet joint pain.
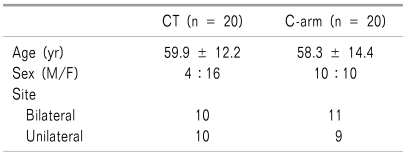
We performed a randomized, prospective study involving 40 patients. The study was conducted with the full approval of the Institutional Review Board. All patients had local paraspinal tenderness and pain on hyperextension and no finding of neurologic defect. All patients underwent a neurologic examination, and CT or magnetic resonance imaging (MRI) was performed. The inclusion criteria were as follows: diagnosis of lumbar facet pain, over 18 years of age, and unilateral or bilateral lumbar facet pain greater than 1 month in duration without any radiating symptoms. The exclusion criteria were as follows: negative response to local anesthetic block, presence of neurological deficit, neurogenic intermittent claudication, and bleeding problem or active infection.
Diagnostic blocks were performed with intermittent fluoroscopic visualization using a 22 gauge, 3.5-inch spinal needle on a minimum 2 medical branches. Each medial branch nerve was infiltrated with 1 ml of 1% lidocaine. Subjects who obtained a greater than 50% pain reduction as assessed using the visual analogue scale (VAS) score for at least 2 hours after each diagnostic block were considered positive.
Patients were assigned to receive either C-arm or CT group. C-arm patients received lumbar medial branch radiofrequency thermocoagulation under c-arm fluoroscopy. The CT group received lumbar medical branch radiofrequency thermocoagulation under computerized tomography.
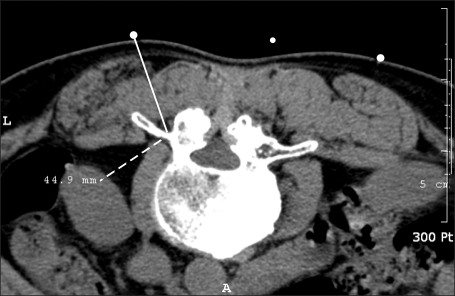
All patients were placed in the prone position with a pillow under the abdomen. In the c-arm group, c-arm fluoroscopy in an oblique position was used for radiographic visualization of the targeted facet joints. A radiofrequency (RF) cannula with a 10 cm, 5 mm active tip was advanced into the superomedial edges of the posterior surfaces of the transverse process of the target nerve (Fig. 1). At each level, correct placement was verified by motor and sensory stimulation. Sensory and motor stimulation was applied at 50 Hz and 2 Hz. The sensory and motor stimulation threshold was required to be less than 0.5 V and at least 2 V, respectively. Approximately 0.5 ml of 2% mepivacaine was injected through each electrode to obtain local anesthesia. Radiofrequency thermocoagulation lesioning was performed at 80℃ for 90 seconds.
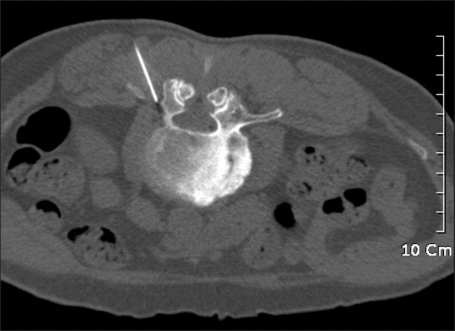
CT-guided rhizotomy was performed under a CT scanner (Philips Brilliance Big Bore, Philips, USA) with 3 mm thick slice without angulation of the gantry. The CT tube voltage and tube current were 120 kVp and 60 mA. With the patient in the prone position on the CT table, a marking device wire was placed to the on lower back and several images are obtained at the level of interest to determine the entry site. Then the safest and shortest route to the junction of the superomedial aspect of the transverse processes with superior articular processes was designed on the CT image, and the distance between the insertion point and the final point was measured. The insertion point was marked using the marking device. Skin and subcutaneous tissue were anesthetized with 1 ml of 2% lidocaine at each procedure site. A 22-gauge 10 cm, 5 mm active tip RF cannula was inserted, and the needle was advanced under quick-check CT fluoroscopy (120 kVp, 30 mA). When the needle tip was located at the final resting position, the sensory and motor stimulation test was applied at 50 Hz and 2 Hz (Fig. 2, 3). After the needle tip was confirmed to be in the proper location, radiofrequency lesioning was performed at 80℃ for 90 seconds.
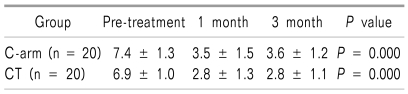
The efficacy of rhizotomy was evaluated with the visual analogue scale before and after the procedure. A paired t-test and Wilcoxon signed rank test were used to compare the pre- and post-treatment results of the average VAS. To compare the means among two groups, the Mann-Whitney test was used.
A total of 40 patients received CT-guidance or C-arm guidance treatment equally divided between the two groups. All patients (20 patients received CT-guidance and 20 patients received C-arm guidance) completed the study (Table 1). For the C-arm group the mean age was 59.9 years whereas the average age of CT group was 58.3 years. There were no differences between the both groups with respect to gender, age and VAS score. No adverse events were encountered during procedure, and no complications were documented three months post procedure. With respect to VAS score, the CT group had relative improvement over the three month interval, on average of 2.8 ± 1.1, and C-arm group, by 3.6 ± 1. There was no significant difference between the CT and C-arm groups in pre- and post-treatment VAS score (Table 2). In both groups, a significant improvement over the 3 months interval was observed in the patients' VAS scores (P = 0.000).
This study demonstrated that radiofrequency lumbar facet rhizotomy under CT guidance showed significant pain relief, but there was no difference in pain relief compared with fluoroscopic guidance radiofrequency lesioning.
Low back pain affects two thirds of the adult population [6]. Lumbar facet syndrome has been implicated as one of the chronic low back pain. Therapeutic lumbar facet joint nerve blocks provide significant pain relief and improvement in functional status [7]. In addition, image-guided radiofrequency lesioning is commonly used for the management of facet origin pain [8-10]. Manejias et al. [11] reported that radiofrequency denervation in non to mild lumbar stenosis patients with chronic zygapophysial joint medicated low back pain improved pain in the long-term.
However, patients who undergo fluoroscopically guided percutaneous radiofrequency denervation of the lumbar facet can develop complications [12]. The RF procedure coagulates the nerve that mediates the patient's pain and thereby provides pain relief [13]. When the precise location of the superior articular process and transverse process junction is difficult to find in patients with severe osteophyte and/or postoperative patients, there is a risk for RF-mediated ventral rami thermal injury if the RF cannular slips more ventrally. Complications include localized pain at the RF denervation sites and neuritic pain.
Under CT, a needle can be precisely placed within the target region [1,14]. Recently CT guidance procedures have been was used to reduce complication and improve of treatment efficacy [4]. CT has been shown to allow highly accurate needle guidance in a number of procedures, including biopsies, drainages, and selective lumbar nerve root blocks, and the use of intermittent fluoroscopy and a low mA setting allows the radiation dose to the patient and radiologist to be minimized [2]. CT guidance is especially helpful in lumbar facet rhizotomy, because when the needle is inserted, an approach can be planned to access the target level and avoid any osseous structure.
Visualization of the spinal contents before insertion of the needle also enables recognition of potential causes of inaccurate needle placement or procedure failure. The technique is fast, safe, and highly accurate in proving appropriate needle placement. Koizuka et al. [15] reported three patients with chronic low back pain underwent CT guided percutaneous RF facet rhizotomy, and the pain score of the 3 patients was reduced without any complications.
In present study, RF treatment provided significantly greater relief of low back pain in both group. However the VAS score improved in CT group than in the c-arm group although no significant difference in pain relief or complications was found. In our opinion, CT-guided RFL offers the clinician a precision target, may be helpful in preventing painful contact with nerve or bone structures, and is of special importance for patients with severe osteophyte and postoperative patients.
Radiation exposure is a major disadvantage of CT-guided interventions. Localization of the target, the advanced needle, the injected contrast agent can be routinely performed with less than 10 axial CT scans. The effective dose in CT depends largely on the number of slices and the chosen mA product. In our study, 30 mA were used for quick check methods. Our experiences with the new helical CT scanners show that this can be further reduced to 25 mA with sufficient information in the bone window. Paulson et al. [2] reported that by using a low-milliampere technique and a quick-check method, CT fluoroscopic time and radiation exposure can be minimized.
Our study has some limitation. First, outcome was measured only by the patients's satisfaction, there was no functional outcome measurement. Second, in present study could not evaluate the radiation exposures during C-arm guidance procedure.
To our knowledge, this current study is the first randomized trial comparing the effectiveness of CT-guidance and C-arm guidance treatment. Our study found no significant difference in pain relief between groups. However VAS score did were more decreased in the CT group. Therefore CT-guidance radiofrequency denervation may be safely and easily be performed by using quick-check CT fluoroscopy
References
1. Tay VK, Fitridge R, Tie ML. Computed tomography fluoroscopy-guided chemical lumbar sympathectomy: simple, safe and effective. Australas Radiol. 2002; 46:163–166. PMID: 12060154.

2. Paulson EK, Sheafor DH, Enterline DS, McAdams HP, Yoshizumi TT. CT fluoroscopy--guided interventional procedures: techniques and radiation dose to radiologists. Radiology. 2001; 220:161–167. PMID: 11425990.

3. Silverman SG, Tuncali K, Adams DF, Nawfel RD, Zou KH, Judy PF. CT fluoroscopy-guided abdominal interventions: techniques, results, and radiation exposure. Radiology. 1999; 212:673–681. PMID: 10478231.

4. Wagner AL. Selective lumbar nerve root blocks with CT fluoroscopic guidance: technique, results, procedure time, and radiation dose. AJNR Am J Neuroradiol. 2004; 25:1592–1594. PMID: 15502144.
5. Wagner AL. CT fluoroscopy-guided epidural injections: technique and results. AJNR Am J Neuroradiol. 2004; 25:1821–1823. PMID: 15569755.
7. Manchikanti L, Manchikanti KN, Manchukonda R, Cash KA, Damron KS, Pampati V, et al. Evaluation of lumbar facet joint nerve blocks in the management of chronic low back pain: preliminary report of a randomized, double-blind controlled trial: clinical trial NCT00355914. Pain Physician. 2007; 10:425–440. PMID: 17525777.
8. Kroll HR, Kim D, Danic MJ, Sankey SS, Gariwala M, Brown M. A randomized, double-blind, prospective study comparing the efficacy of continuous versus pulsed radiofrequency in the treatment of lumbar facet syndrome. J Clin Anesth. 2008; 20:534–537. PMID: 19041042.

9. Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine. 2008; 33:1291–1297. PMID: 18496338.

10. van Wijk RM, Geurts JW, Wynne HJ, Hammink E, Buskens E, Lousberg R, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005; 21:335–344. PMID: 15951652.

11. Manejias EM, Hu J, Tatli Y, Lutz GE. Lumbar zygapophysial joint radiofrequency denervation: a long-term clinical outcome study. HSS J. 2008; 4:180–187. PMID: 18815863.

12. Kornick C, Kramarich SS, Lamer TJ, Todd Sitzman B. Complications of lumbar facet radiofrequency denervation. Spine. 2004; 29:1352–1354. PMID: 15187637.

13. Dreyfuss P, Schwarzer AC, Lau P, Bogduk N. Specificity of lumbar medial branch and L5 dorsal ramus blocks. A computed tomography study. Spine. 1997; 22:895–902. PMID: 9127924.

14. Gevargez A, Groenemeyer D, Schirp S, Braun M. CT-guided percutaneous radiofrequency denervation of the sacroiliac joint. Eur Radiol. 2002; 12:1360–1365. PMID: 12042940.

15. Koizuka S, Saito S, Kawauchi C, Takizawa D, Goto F. Percutaneous radiofrequency lumbar facet rhizotomy guided by computed tomography fluoroscopy. J Anesth. 2005; 19:167–169. PMID: 15875137.

Fig. 1
Radiofrequency electrode is placed in at the angle between the superior articular process and the transverse process of the 3th (A) and 4th (B) lumbar vertebra.

Fig. 2
Initial scout image shows the superior articular process and transverse process. The distance tool is used to calculate an appropriate skin entry site.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download