2. Sauleda J, Núñez B, Sala E, Soriano JB. 2018; Idiopathic pulmonary fibrosis: epidemiology, natural history, phenotypes. Med Sci (Basel). 6:110. DOI:
10.3390/medsci6040110. PMID:
30501130. PMCID:
PMC6313500.

3. B Moore B, Lawson WE, Oury TD, Sisson TH, Raghavendran K, Hogaboam CM. 2013; Animal models of fibrotic lung disease. Am J Respir Cell Mol Biol. 49:167–179. DOI:
10.1165/rcmb.2013-0094TR. PMID:
23526222. PMCID:
PMC3824038.

6. Tashiro J, Rubio GA, Limper AH, Williams K, Elliot SJ, Ninou I, Aidinis V, Tzouvelekis A, Glassberg MK. 2017; Exploring animal models that resemble idiopathic pulmonary fibrosis. Front Med (Lausanne). 4:118. DOI:
10.3389/fmed.2017.00118. PMID:
28804709. PMCID:
PMC5532376.

7. Sugimoto N, Suzukawa M, Nagase H, Koizumi Y, Ro S, Kobayashi K, Yoshihara H, Kojima Y, Kamiyama-Hara A, Hebisawa A, Ohta K. 2019; IL-9 blockade suppresses silica-induced lung inflammation and fibrosis in mice. Am J Respir Cell Mol Biol. 60:232–243. DOI:
10.1165/rcmb.2017-0287OC. PMID:
30240278.

8. Cheresh P, Morales-Nebreda L, Kim SJ, Yeldandi A, Williams DB, Cheng Y, Mutlu GM, Budinger GR, Ridge K, Schumacker PT, Bohr VA, Kamp DW. 2015; Asbestos-induced pulmonary fibrosis is augmented in 8-oxoguanine DNA glycosylase knockout mice. Am J Respir Cell Mol Biol. 52:25–36. DOI:
10.1165/rcmb.2014-0038OC. PMID:
24918270. PMCID:
PMC4370253.

9. Upagupta C, Shimbori C, Alsilmi R, Kolb M. 2018; Matrix abnormalities in pulmonary fibrosis. Eur Respir Rev. 27:180033. DOI:
10.1183/16000617.0033-2018. PMID:
29950306.

12. Wu H, Yu Y, Huang H, Hu Y, Fu S, Wang Z, Shi M, Zhao X, Yuan J, Li J, Yang X, Bin E, Wei D, Zhang H, Zhang J, Yang C, Cai T, Dai H, Chen J, Tang N. 2020; Progressive pulmonary fibrosis is caused by elevated mechanical tension on alveolar stem cells. Cell. 180:107–121.e17. DOI:
10.1016/j.cell.2019.11.027. PMID:
31866069.

13. Togami K, Yamaguchi K, Chono S, Tada H. 2017; Evaluation of permeability alteration and epithelial-mesenchymal transition induced by transforming growth factor-β1 in A549, NCI-H441, and Calu-3 cells: development of an in vitro model of respiratory epithelial cells in idiopathic pulmonary fibrosis. J Pharmacol Toxicol Methods. 86:19–27. DOI:
10.1016/j.vascn.2017.02.023. PMID:
28259823.

14. Chen YW, Huang SX, de Carvalho ALRT, Ho SH, Islam MN, Volpi S, Notarangelo LD, Ciancanelli M, Casanova JL, Bhattacharya J, Liang AF, Palermo LM, Porotto M, Moscona A, Snoeck HW. 2017; A three-dimensional model of human lung development and disease from pluripotent stem cells. Nat Cell Biol. 19:542–549. DOI:
10.1038/ncb3510. PMID:
28436965. PMCID:
PMC5777163.

15. Porotto M, Ferren M, Chen YW, Siu Y, Makhsous N, Rima B, Briese T, Greninger AL, Snoeck HW, Moscona A. 2019; Authentic modeling of human respiratory virus infection in human pluripotent stem cell-derived lung organoids. mBio. 10:e00723–19. DOI:
10.1128/mBio.00723-19. PMID:
31064833. PMCID:
PMC6509192.

16. Heo HR, Kim J, Kim WJ, Yang SR, Han SS, Lee SJ, Hong Y, Hong SH. 2019; Human pluripotent stem cell-derived alveolar epithelial cells are alternatives for in vitro pulmotoxicity assessment. Sci Rep. 9:505. DOI:
10.1038/s41598-018-37193-3. PMID:
30679658. PMCID:
PMC6346100.

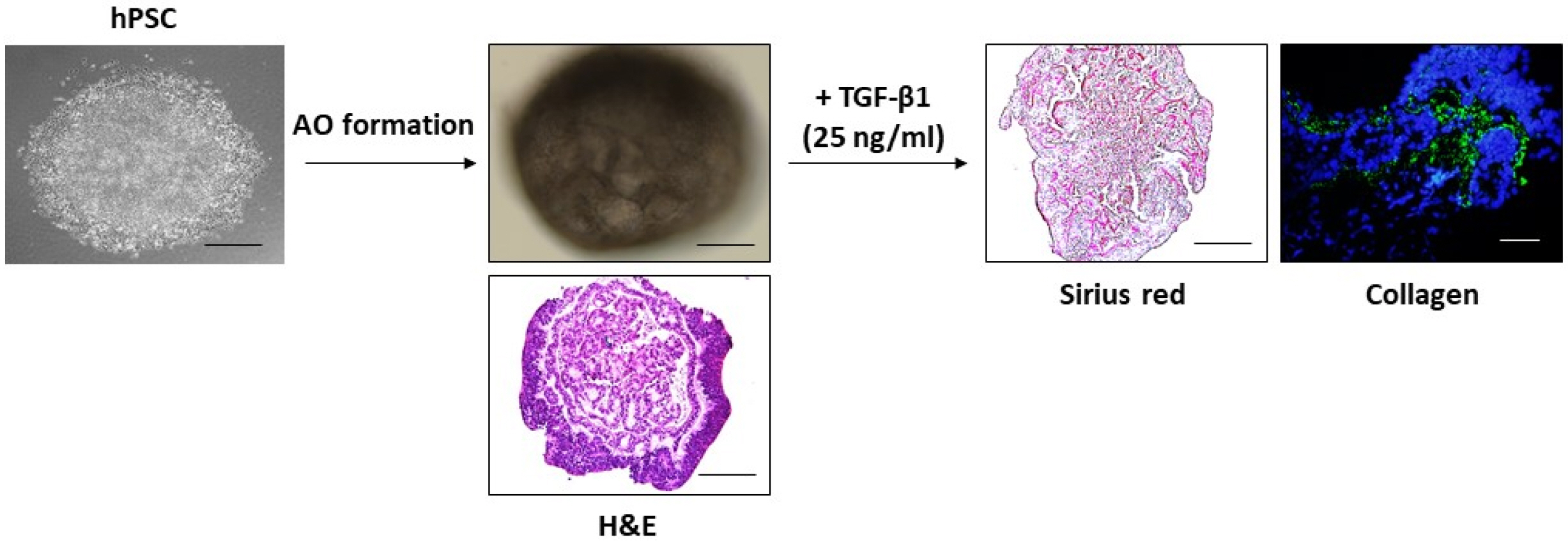
17. Strikoudis A, Cieślak A, Loffredo L, Chen YW, Patel N, Saqi A, Lederer DJ, Snoeck HW. 2019; Modeling of fibrotic lung disease using 3D organoids derived from human pluripotent stem cells. Cell Rep. 27:3709–3723.e5. DOI:
10.1016/j.celrep.2019.05.077. PMID:
31216486. PMCID:
PMC6594401.

18. Kearns NA, Genga RM, Ziller M, Kapinas K, Peters H, Brehm MA, Meissner A, Maehr R. 2013; Generation of organized anterior foregut epithelia from pluripotent stem cells using small molecules. Stem Cell Res. 11:1003–1012. DOI:
10.1016/j.scr.2013.06.007. PMID:
23917481.

19. Snoeck HW. 2015; Modeling human lung development and disease using pluripotent stem cells. Development. 142:13–16. DOI:
10.1242/dev.115469. PMID:
25516965.

20. Nikolić MZ, Sun D, Rawlins EL. 2018; Human lung development: recent progress and new challenges. Development. 145:dev163485. DOI:
10.1242/dev.163485. PMID:
30111617. PMCID:
PMC6124546.

22. McCauley HA, Wells JM. 2017; Pluripotent stem cell-derived organoids: using principles of developmental biology to grow human tissues in a dish. Development. 144:958–962. DOI:
10.1242/dev.140731. PMID:
28292841. PMCID:
PMC5358106.

23. Green MD, Chen A, Nostro MC, d'Souza SL, Schaniel C, Lemischka IR, Gouon-Evans V, Keller G, Snoeck HW. 2011; Generation of anterior foregut endoderm from human embryonic and induced pluripotent stem cells. Nat Biotechnol. 29:267–272. DOI:
10.1038/nbt.1788. PMID:
21358635. PMCID:
PMC4866999.

24. Gkatzis K, Taghizadeh S, Huh D, Stainier DYR, Bellusci S. 2018; Use of three-dimensional organoids and lung-on-a-chip methods to study lung development, regeneration and disease. Eur Respir J. 52:1800876. DOI:
10.1183/13993003.00876-2018. PMID:
30262579.

25. Barkauskas CE, Chung MI, Fioret B, Gao X, Katsura H, Hogan BL. 2017; Lung organoids: current uses and future promise. Development. 144:986–997. DOI:
10.1242/dev.140103. PMID:
28292845. PMCID:
PMC5358104.

26. Nikolić MZ, Caritg O, Jeng Q, Johnson JA, Sun D, Howell KJ, Brady JL, Laresgoiti U, Allen G, Butler R, Zilbauer M, Giangreco A, Rawlins EL. 2017; Human embryonic lung epithelial tips are multipotent progenitors that can be expanded in vitro as long-term self-renewing organoids. Elife. 6:e26575. DOI:
10.7554/eLife.26575. PMID:
28665271. PMCID:
PMC5555721.

27. Miller AJ, Dye BR, Ferrer-Torres D, Hill DR, Overeem AW, Shea LD, Spence JR. 2019; Generation of lung organoids from human pluripotent stem cells in vitro. Nat Protoc. 14:518–540. DOI:
10.1038/s41596-018-0104-8. PMID:
30664680. PMCID:
PMC6531049.

28. Kaushik G, Ponnusamy MP, Batra SK. 2018; Concise review: current status of three-dimensional organoids as preclinical models. Stem Cells. 36:1329–1340. DOI:
10.1002/stem.2852. PMID:
29770526. PMCID:
PMC6158106.

29. Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, Clevers H. 2007; Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 449:1003–1007. DOI:
10.1038/nature06196. PMID:
17934449.

30. Sato T, van Es JH, Snippert HJ, Stange DE, Vries RG, van den Born M, Barker N, Shroyer NF, van de Wetering M, Clevers H. 2011; Paneth cells constitute the niche for Lgr5 stem cells in intestinal crypts. Nature. 469:415–418. DOI:
10.1038/nature09637. PMID:
21113151. PMCID:
PMC3547360.

31. Forbester JL, Goulding D, Vallier L, Hannan N, Hale C, Pickard D, Mukhopadhyay S, Dougan G. 2015; Interaction of salmonella enterica serovar Typhimurium with intestinal organoids derived from human induced pluripotent stem cells. Infect Immun. 83:2926–2934. DOI:
10.1128/IAI.00161-15. PMID:
25964470. PMCID:
PMC4468523.

32. Rodansky ES, Johnson LA, Huang S, Spence JR, Higgins PD. 2015; Intestinal organoids: a model of intestinal fibrosis for evaluating anti-fibrotic drugs. Exp Mol Pathol. 98:346–351. DOI:
10.1016/j.yexmp.2015.03.033. PMID:
25828392. PMCID:
PMC5915372.

33. Janssens S, Schotsaert M, Karnik R, Balasubramaniam V, Dejosez M, Meissner A, García-Sastre A, Zwaka TP. 2018; Zika virus alters DNA methylation of neural genes in an organoid model of the developing human brain. mSystems. 3:e00219–17. DOI:
10.1128/mSystems.00219-17. PMID:
29435496. PMCID:
PMC5801341.

34. Sacramento CQ, de Melo GR, de Freitas CS, Rocha N, Hoelz LV, Miranda M, Fintelman-Rodrigues N, Marttorelli A, Ferreira AC, Barbosa-Lima G, Abrantes JL, Vieira YR, Bastos MM, de Mello Volotão E, Nunes EP, Tschoeke DA, Leomil L, Loiola EC, Trindade P, Rehen SK, Bozza FA, Bozza PT, Boechat N, Thompson FL, de Filippis AM, Brüning K, Souza TM. 2017; The clinically approved antiviral drug sofosbuvir inhibits Zika virus replication. Sci Rep. 7:40920. DOI:
10.1038/srep40920. PMID:
28098253. PMCID:
PMC5241873.

35. Smits LM, Reinhardt L, Reinhardt P, Glatza M, Monzel AS, Stanslowsky N, Rosato-Siri MD, Zanon A, Antony PM, Bellmann J, Nicklas SM, Hemmer K, Qing X, Berger E, Kalmbach N, Ehrlich M, Bolognin S, Hicks AA, Wegner F, Sterneckert JL, Schwamborn JC. 2019; Modeling Parkinson's disease in midbrain-like organoids. NPJ Parkinsons Dis. 5:5. DOI:
10.1038/s41531-019-0078-4. PMID:
30963107. PMCID:
PMC6450999.

36. Raja WK, Mungenast AE, Lin YT, Ko T, Abdurrob F, Seo J, Tsai LH. 2016; Self-organizing 3D human neural tissue derived from induced pluripotent stem cells recapitulate Alzheimer's disease phenotypes. PLoS One. 11:e0161969. DOI:
10.1371/journal.pone.0161969. PMID:
27622770. PMCID:
PMC5021368.

37. Ouchi R, Togo S, Kimura M, Shinozawa T, Koido M, Koike H, Thompson W, Karns RA, Mayhew CN, McGrath PS, McCauley HA, Zhang RR, Lewis K, Hakozaki S, Ferguson A, Saiki N, Yoneyama Y, Takeuchi I, Mabuchi Y, Akazawa C, Yoshikawa HY, Wells JM, Takebe T. 2019; Modeling steatohepatitis in humans with pluripotent stem cell-derived orga-noids. Cell Metab. 30:374–384.e6. DOI:
10.1016/j.cmet.2019.05.007. PMID:
31155493. PMCID:
PMC6687537.

38. Aguisanda F, Yeh CD, Chen CZ, Li R, Beers J, Zou J, Thorne N, Zheng W. 2017; Neural stem cells for disease modeling of Wolman disease and evaluation of therapeutics. Orphanet J Rare Dis. 12:120. DOI:
10.1186/s13023-017-0670-9. PMID:
28659158. PMCID:
PMC5490176.

39. Nie YZ, Zheng YW, Miyakawa K, Murata S, Zhang RR, Sekine K, Ueno Y, Takebe T, Wakita T, Ryo A, Taniguchi H. 2018; Recapitulation of hepatitis B virus-host interactions in liver organoids from human induced pluripotent stem cells. EBioMedicine. 35:114–123. DOI:
10.1016/j.ebiom.2018.08.014. PMID:
30120080. PMCID:
PMC6156717.

40. Dekkers JF, Wiegerinck CL, de Jonge HR, Bronsveld I, Janssens HM, de Winter-de Groot KM, Brandsma AM, de Jong NW, Bijvelds MJ, Scholte BJ, Nieuwenhuis EE, van den Brink S, Clevers H, van der Ent CK, Middendorp S, Beekman JM. 2013; A functional CFTR assay using primary cystic fibrosis intestinal organoids. Nat Med. 19:939–945. DOI:
10.1038/nm.3201. PMID:
23727931.

42. Wilkinson DC, Alva-Ornelas JA, Sucre JM, Vijayaraj P, Durra A, Richardson W, Jonas SJ, Paul MK, Karumbayaram S, Dunn B, Gomperts BN. 2017; Development of a three-dimensional bioengineering technology to generate lung tissue for personalized disease modeling. Stem Cells Transl Med. 6:622–633. DOI:
10.5966/sctm.2016-0192. PMID:
28191779. PMCID:
PMC5442826.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download