1. Cahill TJ, Choudhury RP, Riley PR. 2017; Heart regeneration and repair after myocardial infarction: translational opportunities for novel therapeutics. Nat Rev Drug Discov. 16:699–717. DOI:
10.1038/nrd.2017.106. PMID:
28729726.

2. Ghiroldi A, Piccoli M, Cirillo F, Monasky MM, Ciconte G, Pappone C, Anastasia L. 2018; Cell-based therapies for cardiac regeneration: a comprehensive review of past and ongoing strategies. Int J Mol Sci. 19:3194. DOI:
10.3390/ijms19103194. PMID:
30332812. PMCID:
PMC6214096.

3. Arnous S, Mozid A, Martin J, Mathur A. 2012; Bone marrow mononuclear cells and acute myocardial infarction. Stem Cell Res Ther. 3:2. DOI:
10.1186/scrt93. PMID:
22264393. PMCID:
PMC3340546.

4. Colicchia M, Jones DA, Beirne AM, Hussain M, Weeraman D, Rathod K, Veerapen J, Lowdell M, Mathur A. 2019; Umbilical cord-derived mesenchymal stromal cells in cardiovascular disease: review of preclinical and clinical data. Cytotherapy. 21:1007–1018. DOI:
10.1016/j.jcyt.2019.04.056. PMID:
31540804.

5. Fisher SA, Brunskill SJ, Doree C, Mathur A, Taggart DP, Martin-Rendon E. 2014; Stem cell therapy for chronic ischaemic heart disease and congestive heart failure. Cochrane Database Syst Rev. (4):CD007888. DOI:
10.1002/14651858.CD007888.pub2. PMID:
28012165. PMCID:
PMC6463978.

6. Clifford DM, Fisher SA, Brunskill SJ, Doree C, Mathur A, Watt S, Martin-Rendon E. 2012; Stem cell treatment for acute myocardial infarction. Cochrane Database Syst Rev. (2):CD006536. DOI:
10.1002/14651858.CD006536.pub3. PMID:
26419913.

7. Can A, Yigman Z. Bolontrade MF, Garcia MG, editors. 2017. Mesenchymal stem/stromal cells from neonatal tissues. Mesenchymal stromal cells as tumor stromal modulators. Academic Press;London: p. 65–101. DOI:
10.1016/B978-0-12-803102-5.00003-3. PMID:
28583752. PMCID:
PMC6136314.

8. Can A, Celikkan FT, Cinar O. 2017; Umbilical cord mesenchy-mal stromal cell transplantations: a systemic analysis of clinical trials. Cytotherapy. 19:1351–1382. DOI:
10.1016/j.jcyt.2017.08.004. PMID:
28964742.

9. Can A, Ulus A, Topal Celikkan F, Mungan C, Sucu M, Kurtoglu M, Simsek E, Cinar O. Preliminary results of the human umbilical cord mesenchymal stromal cell (HUC-MSC) transplantation in myocardial ischemia (HUC-HEART Trial). Paper presented at: International Society for Stem Cell Research (ISSCR) Annual Meeting. 2017 June 14-17; Boston, MA, USA.
10. Bartolucci J, Verdugo FJ, González PL, Larrea RE, Abarzua E, Goset C, Rojo P, Palma I, Lamich R, Pedreros PA, Valdivia G, Lopez VM, Nazzal C, Alcayaga-Miranda F, Cuenca J, Brobeck MJ, Patel AN, Figueroa FE, Khoury M. 2017; Safety and efficacy of the intravenous infusion of umbilical cord mesenchymal stem cells in patients with heart failure: a phase 1/2 randomized controlled trial (RIMECARD Trial [Randomized Clinical Trial of Intravenous Infusion Umbilical Cord Mesenchymal Stem Cells on Cardiopathy]). Circ Res. 121:1192–1204. DOI:
10.1161/CIRCRESAHA.117.310712. PMID:
28974553. PMCID:
PMC6372053.

11. Zhao XF, Xu Y, Zhu ZY, Gao CY, Shi YN. 2015; Clinical observation of umbilical cord mesenchymal stem cell treatment of severe systolic heart failure. Genet Mol Res. 14:3010–3017. DOI:
10.4238/2015.April.10.11. PMID:
25966065.

12. Musialek P, Mazurek A, Jarocha D, Tekieli L, Szot W, Kostkiewicz M, Banys RP, Urbanczyk M, Kadzielski A, Trystula M, Kijowski J, Zmudka K, Podolec P, Majka M. 2015; Myocardial regeneration strategy using Wharton's jelly mesenchymal stem cells as an off-the-shelf 'unlimited' therapeutic agent: results from the acute myocardial infarction first-in-man study. Postepy Kardiol Interwencyjnej. 11:100–107. DOI:
10.5114/pwki.2015.52282. PMID:
26161101. PMCID:
PMC4495125.

13. Gao LR, Chen Y, Zhang NK, Yang XL, Liu HL, Wang ZG, Yan XY, Wang Y, Zhu ZM, Li TC, Wang LH, Chen HY, Chen YD, Huang CL, Qu P, Yao C, Wang B, Chen GH, Wang ZM, Xu ZY, Bai J, Lu D, Shen YH, Guo F, Liu MY, Yang Y, Ding YC, Yang Y, Tian HT, Ding QA, Li LN, Yang XC, Hu X. 2015; Intracoronary infusion of Wharton's jelly-derived mesenchymal stem cells in acute myocardial infarction: double-blind, randomized controlled trial. BMC Med. 13:162. DOI:
10.1186/s12916-015-0399-z. PMID:
26162993. PMCID:
PMC4499169.

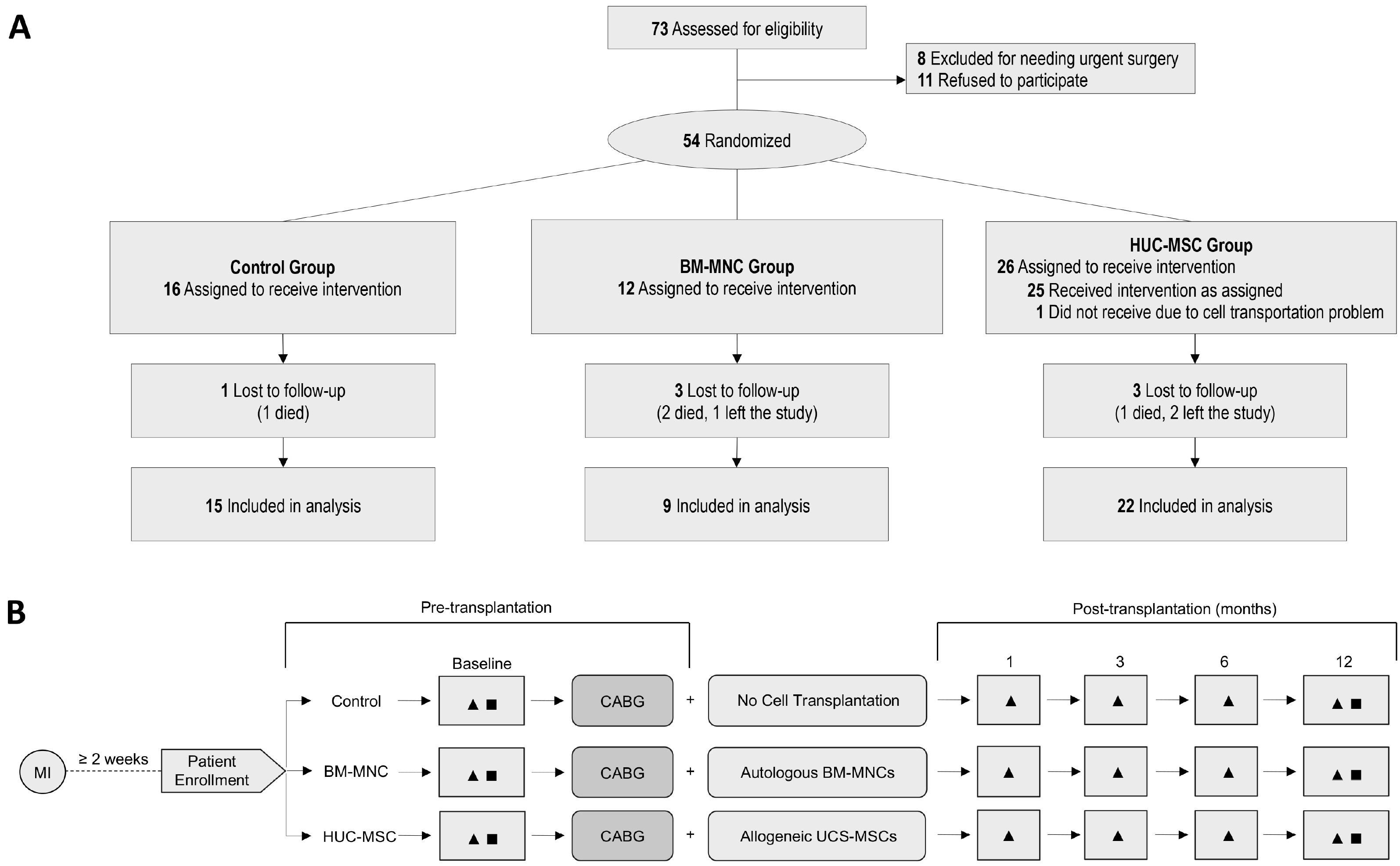
14. Can A, Ulus AT, Cinar O, Topal Celikkan F, Simsek E, Akyol M, Canpolat U, Erturk M, Kara F, Ilhan O. 2015; Human umbilical cord mesenchymal stromal cell transplantation in myocardial ischemia (HUC-HEART Trial). A study protocol of a phase 1/2, controlled and randomized trial in combination with coronary artery bypass grafting. Stem Cell Rev Rep. 11:752–760. DOI:
10.1007/s12015-015-9601-0. PMID:
26123356.

15. Bilal M, Haseeb A, Sher Khan MA. 2015; Intracoronary infusion of Wharton's jelly-derived mesenchymal stem cells: a novel treatment in patients of acute myocardial infarction. J Pak Med Assoc. 65:1369.
16. Li X, Hu YD, Guo Y, Chen Y, Guo DX, Zhou HL, Zhang FL, Zhao QN. 2015; Safety and efficacy of intracoronary human umbilical cord-derived mesenchymal stem cell treatment for very old patients with coronary chronic total occlusion. Curr Pharm Des. 21:1426–1432. DOI:
10.2174/1381612821666141126100636. PMID:
25427243.

17. Celikkan FT, Mungan C, Sucu M, Ulus AT, Cinar O, Ili EG, Can A. 2019; Optimizing the transport and storage conditions of current Good Manufacturing Practice-grade human umbilical cord mesenchymal stromal cells for transplantation (HUC-HEART Trial). Cytotherapy. 21:64–75. DOI:
10.1016/j.jcyt.2018.10.010. PMID:
30455106.

18. Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, Ficaro EP, Freeman MR, Hendel RC, Jain D, Leonard SM, Nichols KJ, Polk DM, Soman P. 2010; Single photon-emission computed tomography. J Nucl Cardiol. 17:941–973. DOI:
10.1007/s12350-010-9246-y. PMID:
20552312.

19. Dilsizian V, Bacharach SL, Beanlands RS, Bergmann SR, Delbeke D, Dorbala S, Gropler RJ, Knuuti J, Schelbert HR, Travin MI. 2016; ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J Nucl Cardiol. 23:1187–1226. DOI:
10.1007/s12350-016-0522-3. PMID:
27392702.

20. Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB. 1985; The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 132:919–923. PMID:
3978515. PMCID:
PMC1345899.
21. Kancharla K, Weissman G, Elagha AA, Kancherla K, Samineni S, Hill PC, Boyce S, Fuisz AR. 2016; Scar quantification by cardiovascular magnetic resonance as an independent predictor of long-term survival in patients with ischemic heart failure treated by coronary artery bypass graft surgery. J Cardiovasc Magn Reson. 18:45. DOI:
10.1186/s12968-016-0265-y. PMID:
27430331. PMCID:
PMC4950709.

22. Obrzut S, Jamshidi N, Karimi A, Birgersdotter-Green U, Hoh C. 2010; Imaging and modeling of myocardial metabolism. J Cardiovasc Transl Res. 3:384–396. DOI:
10.1007/s12265-010-9170-1. PMID:
20559785. PMCID:
PMC2899022.

23. Michler RE, Rouleau JL, Al-Khalidi HR, Bonow RO, Pellikka PA, Pohost GM, Holly TA, Oh JK, Dagenais F, Milano C, Wrobel K, Pirk J, Ali IS, Jones RH, Velazquez EJ, Lee KL, Di Donato M. 2013; Insights from the STICH trial: change in left ventricular size after coronary artery bypass grafting with and without surgical ventricular reconstruction. J Thorac Cardiovasc Surg. 146:1139–1145.e6. DOI:
10.1016/j.jtcvs.2012.09.007. PMID:
23111018. PMCID:
PMC3810307.

24. Karantalis V, DiFede DL, Gerstenblith G, Pham S, Symes J, Zambrano JP, Fishman J, Pattany P, McNiece I, Conte J, Schulman S, Wu K, Shah A, Breton E, Davis-Sproul J, Schwarz R, Feigenbaum G, Mushtaq M, Suncion VY, Lardo AC, Borrello I, Mendizabal A, Karas TZ, Byrnes J, Lowery M, Heldman AW, Hare JM. 2014; Autologous mesenchymal stem cells produce concordant improvements in regional function, tissue perfusion, and fibrotic burden when administered to patients undergoing coronary artery bypass grafting: The Prospective Randomized Study of Mesenchy-mal Stem Cell Therapy in Patients Undergoing Cardiac Surgery (PROMETHEUS) trial. Circ Res. 114:1302–1310. DOI:
10.1161/CIRCRESAHA.114.303180. PMID:
24565698. PMCID:
PMC4104798.

25. Fang Z, Yin X, Wang J, Tian N, Ao Q, Gu Y, Liu Y. 2016; Functional characterization of human umbilical cord-derived mesenchymal stem cells for treatment of systolic heart failure. Exp Ther Med. 12:3328–3332. DOI:
10.3892/etm.2016.3748. PMID:
27882158. PMCID:
PMC5103788.

26. Ramkisoensing AA, Pijnappels DA, Askar SF, Passier R, Swildens J, Goumans MJ, Schutte CI, de Vries AA, Scherjon S, Mummery CL, Schalij MJ, Atsma DE. 2011; Human embryonic and fetal mesenchymal stem cells differentiate toward three different cardiac lineages in contrast to their adult counterparts. PLoS One. 6:e24164. DOI:
10.1371/journal.pone.0024164. PMID:
21931658. PMCID:
PMC3170333.

27. Liu CB, Huang H, Sun P, Ma SZ, Liu AH, Xue J, Fu JH, Liang YQ, Liu B, Wu DY, Lü SH, Zhang XZ. 2016; Human umbilical cord-derived mesenchymal stromal cells improve left ventricular function, perfusion, and remodeling in a porcine model of chronic myocardial ischemia. Stem Cells Transl Med. 5:1004–1013. DOI:
10.5966/sctm.2015-0298. PMID:
27334487. PMCID:
PMC4954453.

28. Santos Nascimento D, Mosqueira D, Sousa LM, Teixeira M, Filipe M, Resende TP, Araújo AF, Valente M, Almeida J, Martins JP, Santos JM, Bárcia RN, Cruz P, Cruz H, Pinto-do-Ó P. 2014; Human umbilical cord tissue-derived mesenchymal stromal cells attenuate remodeling after myocardial infarction by proangiogenic, antiapoptotic, and endogenous cell-activation mechanisms. Stem Cell Res Ther. 5:5. DOI:
10.1186/scrt394. PMID:
24411922. PMCID:
PMC4055157.

29. Huang J, Zhang Z, Guo J, Ni A, Deb A, Zhang L, Mirotsou M, Pratt RE, Dzau VJ. 2010; Genetic modification of mesenchymal stem cells overexpressing CCR1 increases cell viability, migration, engraftment, and capillary density in the injured myocardium. Circ Res. 106:1753–1762. DOI:
10.1161/CIRCRESAHA.109.196030. PMID:
20378860. PMCID:
PMC2884066.

30. Brunskill SJ, Hyde CJ, Doree CJ, Watt SM, Martin-Rendon E. 2009; Route of delivery and baseline left ventricular ejection fraction, key factors of bone-marrow-derived cell therapy for ischaemic heart disease. Eur J Heart Fail. 11:887–896. DOI:
10.1093/eurjhf/hfp101. PMID:
19654139.

31. Ang KL, Chin D, Leyva F, Foley P, Kubal C, Chalil S, Srinivasan L, Bernhardt L, Stevens S, Shenje LT, Galiñanes M. 2008; Randomized, controlled trial of intramuscu-lar or intracoronary injection of autologous bone marrow cells into scarred myocardium during CABG versus CABG alone. Nat Clin Pract Cardiovasc Med. 5:663–670. DOI:
10.1038/ncpcardio1321. PMID:
18711405.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download