1. Ong KY. What’s new in the Global Initiative for Asthma 2018 report and beyond. Allergo J Int. 2019; 28(2):63–72.

2. Kuruvilla ME, Lee FE, Lee GB. Understanding asthma phenotypes, endotypes, and mechanisms of disease. Clin Rev Allergy Immunol. 2019; 56(2):219–233. PMID:
30206782.

3. Corren J, Weinstein S, Janka L, Zangrilli J, Garin M. Phase 3 study of reslizumab in patients with poorly controlled asthma: effects across a broad range of eosinophil counts. Chest. 2016; 150(4):799–810. PMID:
27018175.

4. Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012; 380(9842):651–659. PMID:
22901886.

5. Zeiger RS, Schatz M, Li Q, Chen W, Khatry DB, Gossage D, et al. High blood eosinophil count is a risk factor for future asthma exacerbations in adult persistent asthma. J Allergy Clin Immunol Pract. 2014; 2(6):741–750. PMID:
25439366.

6. Tran TN, Khatry DB, Ke X, Ward CK, Gossage D. High blood eosinophil count is associated with more frequent asthma attacks in asthma patients. Ann Allergy Asthma Immunol. 2014; 113(1):19–24. PMID:
24846699.

7. Price DB, Rigazio A, Campbell JD, Bleecker ER, Corrigan CJ, Thomas M, et al. Blood eosinophil count and prospective annual asthma disease burden: a UK cohort study. Lancet Respir Med. 2015; 3(11):849–858. PMID:
26493938.

8. Zeiger RS, Schatz M, Dalal AA, Chen W, Sadikova E, Suruki RY, et al. Blood eosinophil count and outcomes in severe uncontrolled asthma: a prospective study. J Allergy Clin Immunol Pract. 2017; 5(1):144–153.e8. PMID:
27665383.

9. Kim TB, Park CS, Bae YJ, Cho YS, Moon HB. COREA Study Group. Factors associated with severity and exacerbation of asthma: a baseline analysis of the Cohort for Reality and Evolution of Adult Asthma in Korea (COREA). Ann Allergy Asthma Immunol. 2009; 103(4):311–317. PMID:
19852195.

10. Park SY, Jung H, Kim JH, Seo B, Kwon OY, Choi S, et al. Longitudinal analysis to better characterize asthma-COPD overlap syndrome: findings from an adult asthma cohort in Korea (COREA). Clin Exp Allergy. 2019; 49(5):603–614. PMID:
30657218.

11. Park SY, Jung HW, Lee JM, Shin B, Kim HJ, Kim MH, et al. Novel trajectories for identifying asthma phenotypes: a longitudinal study in Korean asthma cohort, COREA. J Allergy Clin Immunol Pract. 2019; 7(6):1850–1857.e4. PMID:
30794966.

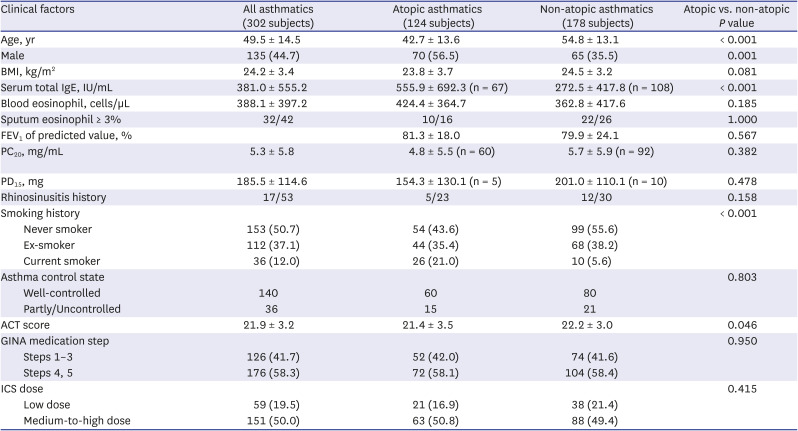
12. Jang AS, Kim SH, Kim TB, Park HW, Kim SH, Chang YS, et al. Impact of atopy on asthma and allergic rhinitis in the cohort for reality and evolution of adult asthma in Korea. Allergy Asthma Immunol Res. 2013; 5(3):143–149. PMID:
23638312.

13. Adinoff AD, Rosloniec DM, McCall LL, Nelson HS. Immediate skin test reactivity to Food and Drug Administration-approved standardized extracts. J Allergy Clin Immunol. 1990; 86(5):766–774. PMID:
2229841.

14. Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006; 117(3):549–556. PMID:
16522452.

15. Hogan AD, Bernstein JA. GINA updated 2019: landmark changes recommended for asthma management. Ann Allergy Asthma Immunol. 2020; 124(4):311–313. PMID:
31734328.
16. Nelson RK, Bush A, Stokes J, Nair P, Akuthota P. Eosinophilic asthma. J Allergy Clin Immunol Pract. 2020; 8(2):465–473. PMID:
31786254.

17. Chongmelaxme B, Chaiyakunapruk N, Dilokthornsakul P. Association between adherence and severe asthma exacerbation: a systematic review and meta-analysis. J Am Pharm Assoc (2003). 2020; 60(5):669–685.e2. PMID:
32192946.

18. Stern L, Berman J, Lumry W, Katz L, Wang L, Rosenblatt L, et al. Medication compliance and disease exacerbation in patients with asthma: a retrospective study of managed care data. Ann Allergy Asthma Immunol. 2006; 97(3):402–408. PMID:
17042149.

19. Tran TN, Zeiger RS, Peters SP, Colice G, Newbold P, Goldman M, et al. Overlap of atopic, eosinophilic, and T
H2-high asthma phenotypes in a general population with current asthma. Ann Allergy Asthma Immunol. 2016; 116(1):37–42. PMID:
26707771.

20. Katz LE, Gleich GJ, Hartley BF, Yancey SW, Ortega HG. Blood eosinophil count is a useful biomarker to identify patients with severe eosinophilic asthma. Ann Am Thorac Soc. 2014; 11(4):531–536. PMID:
24606022.

21. Casciano J, Krishnan J, Dotiwala Z, Li C, Sun SX. Clinical and economic burden of elevated blood eosinophils in patients with and without uncontrolled asthma. J Manag Care Spec Pharm. 2017; 23(1):85–91. PMID:
28025926.

22. Cho JY, Miller M, Baek KJ, Han JW, Nayar J, Lee SY, et al. Inhibition of airway remodeling in IL-5-deficient mice. J Clin Invest. 2004; 113(4):551–560. PMID:
14966564.

23. Esteban-Gorgojo I, Antolín-Amérigo D, Domínguez-Ortega J, Quirce S. Non-eosinophilic asthma: current perspectives. J Asthma Allergy. 2018; 11:267–281. PMID:
30464537.

24. Chipps BE, Jarjour N, Calhoun WJ, Iqbal A, Haselkorn T, Yang M, et al. A comprehensive analysis of the stability of blood eosinophil levels. Ann Am Thorac Soc. 2021; 18(12):1978–1987. PMID:
33891831.

25. Jung JW, Kim SH, Kwon JW, Kim TW, Kang HR, Park HW, et al. Clinical characteristics and long-term outcomes related to sputum eosinophilia in Korean asthmatics. Asia Pac Allergy. 2011; 1(1):16–24. PMID:
22053292.

26. Toledo-Pons N, van Boven JFM, Muncunill J, Millan A, Roman-Rodriguez M, Lopez-Andrade B, et al. Impact of blood eosinophil variability in asthma: a real-life population study. Ann Am Thorac Soc. Forthcoming. 2021; DOI:
10.1513/AnnalsATS.202103-409OC.

27. Chen YY, Khoury P, Ware JM, Holland-Thomas NC, Stoddard JL, Gurprasad S, et al. Marked and persistent eosinophilia in the absence of clinical manifestations. J Allergy Clin Immunol. 2014; 133(4):1195–1202. PMID:
23987798.

28. Rothenberg ME, Hogan SP. The eosinophil. Annu Rev Immunol. 2006; 24(1):147–174. PMID:
16551246.

29. An J, Lee JH, Sim JH, Song WJ, Kwon HS, Cho YS, et al. Serum eosinophil-derived neurotoxin better reflect asthma control status than blood eosinophil counts. J Allergy Clin Immunol Pract. 2020; 8(8):2681–2688.e1. PMID:
32304842.

30. Evans PM, O’Connor BJ, Fuller RW, Barnes PJ, Chung KF. Effect of inhaled corticosteroids on peripheral blood eosinophil counts and density profiles in asthma. J Allergy Clin Immunol. 1993; 91(2):643–650. PMID:
8436777.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download