INTRODUCTION
The coronavirus disease 2019 (COVID-19) is an infection caused by a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), first detected in Wuhan in December 2019, which rapidly spread around the world. As of May 30, 2021, a cumulative total of 169 million cases and 3.5 million deaths have been reported worldwide since the start of the outbreak.
1 In South Korea, the onset of the first case was on January 20, 2020. Until May 30, 2021, 130,876 confirmed cases were identified and 1,957 deaths occurred due to COVID-19.
2 As the pandemic continues to spread, the Ministry of Health and Welfare (MOHW) of South Korea focused on an increase in diagnostic capacity and the medical response to manage COVID-19, including redesigned healthcare service provision by the government at the national level.
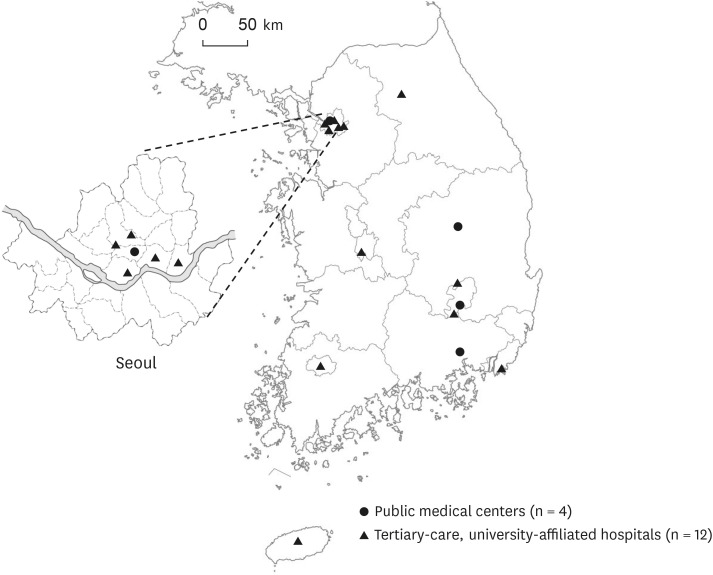
3 Public medical centers in each lesions were prepared for patients with mild to moderate COVID-19, and large public medical centers and tertiary-care hospitals, which are usually university-affiliated in each region, were prepared for patients with severe or critical COVID-19.
4 As the global COVID-19 pandemic continues, it is a serious question whether the capacity of the current healthcare system can keep pace with the pandemic.
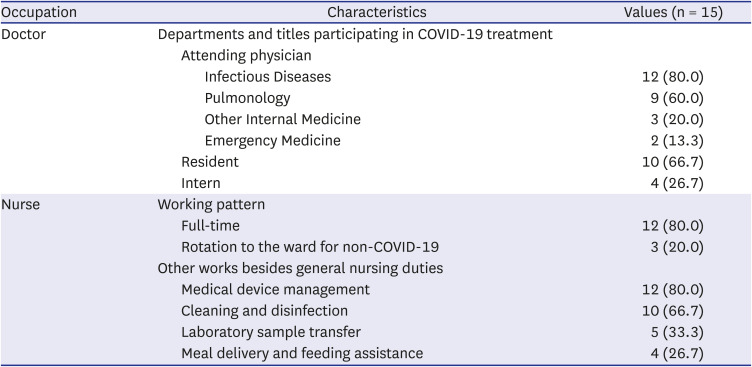
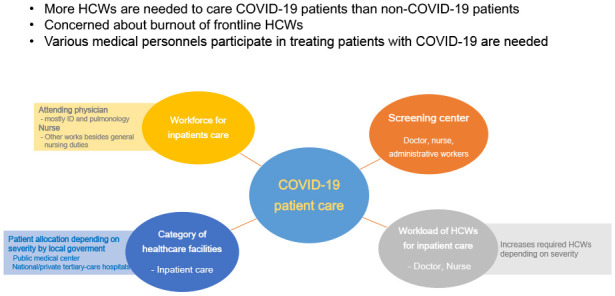
5 In Korea, most of the public medical centers and tertiary-care hospitals have COVID-19 screening clinics and quarantine wards for inpatients with COVID-19. Moreover, personal protective equipment (PPE) used in protecting the HCWs from SARS-CoV-2 transmission significantly increases the burden on HCWs. As additional work was operated with the existing healthcare workers (HCWs) without additional workforce in most healthcare facilities, overloading of the work of HCWs occurred. Therefore, it is no wonder that caring for patients with COVID-19 increases workload and consequently requires more manpower than patients not having COVID-19. However, so far, there has been no research on the actual workforce needed to care for COVID-19 patients. Despite that most hospitals in Korea are operating screening centers for diagnosis and wards for treatment, there is no helpful information regarding the workforce of HCWs managing COVID-19 in each hospital; therefore, it is necessary to investigate the actual workforce and workload of HCWs in COVID-19 management to implement a method that can efficiently minimize the fatigue of HCWs. We performed this research to analyze the current workload of HCWs responding to COVID-19.
DISCUSSION
Since South Korea had experienced the Middle-East respiratory syndrome coronavirus (MERS-CoV) outbreak in 2015, the government and many hospitals have been prepared for the next outbreak of unknown respiratory infectious disease; however, preparations, such as healthcare personnel and facilities, were not enough.
8 When the explosive outbreak at the epicenter occurred, we experienced a shortage of medical resources. With the efforts of the Korean government and medical professionals, national and private tertiary-care university-affiliated hospitals and national medical centers were mobilized to prepare beds for patients with severe COVID-19 and the non-hospital facilities for isolating asymptomatic patients or patients with mild symptoms were opened. At the time this study was conducted, the medical system was in a relatively stable status. National or private tertiary-care hospitals equipped with negative pressure intensive care units and medical experts in respiratory and infectious diseases (ID) were designated for severe or critical patients, and public medical centers with negative pressure units were designated for mild to moderate patients. This study revealed that the difference in the number of HCWs allocated according to the severity of COVID-19 is large. Patients with severe or critical COVID-19 needed a high-flow nasal cannula (HFNC) or ventilator management.
9 Patients with COVID-19 who are receiving HFNC or mechanical ventilation should be closely monitored by sufficient medical personnel. Actually, compared to the Korean nursing rating system’s highest level, which is above 2 for critical care or 0.5 for general care,
10 more nursing personnel were needed when treating severe patients with COVID-19. This is the first study to arithmetically investigate the HCWs required to treat inpatients with COVID-19. The numbers presented in this study do not represent the required medical personnel. Since many frontline HCWs are already suffering from burnout,
7 this result is expected to be used as a reference when deploying medical personnel in the event of a continuous COVID-19 outbreak and any other pandemic in the near future. During the COVID-19 outbreak, many ID physicians reported that supporting medical staff that directly cares for patients with COVID-19 was a more urgent requirement than dealing with issues arising due to lack of devices.
7
The healthcare workforce comprises various specialties, each with an assigned duty and sometimes they do extra work that they do not usually do; especially, this study showed that nurses in COVID-19 isolation wards did work that they do not usually do. And, Park et al.
7 showed that ID physicians experienced burnout more during the COVID-19 outbreak. Work overload may lead to physical and mental exhaustion causing HCWs burnout. As with the general ward, medical personnel other than doctors and nurses (such as cleaning staff, paramedicine and nurse-assistant) are also needed in the COVID-19 ward. Most of them tend to avoid work because of the fear of uncertainty and the stigma of caring for COVID-19 patients; therefore, adequate and active training regarding patients with epidemic infectious diseases is needed for all medical personnel. If various medical personnel participate in treating patients with COVID-19, the burden that was placed on frontline HCWs could be reduced.
As the COVID-19 pandemic continues, the roles of ID physicians have been emphasized. ID physicians have acted as coordinators and are at the forefront response to the outbreak, provide patient care, and have been in charge of various roles, such as infection control, administration, education and research without additional personnel.
7 As of 2019, only 275 physicians acquired ID as a sub-specialty in Korea.
11 In this study, although public medical centers treat many patients with COVID-19, there were no ID physicians, except in a national medical center. It is necessary to strategically expand healthcare personnel capable of coping with pandemic infectious diseases through the national system.
South Korea achieved compulsory universal health coverage of its population in 1989 and merged all health insurance societies into a single payer, the National Health Insurance (NHI), in 2000.
12 All patients have access to all health services which are covered by the NHI. Although more than 90% of health facilities are private, they are required to participate in the NHI system with the same contract conditions for both public and private providers set by NHI law.
13 As the Korean health system has developed very rapidly in a short period, health utilization has grown tremendously as well. However, due to direct accessibility to any healthcare facilities in any time, fee-for-service payment system, and low medical cost, the amount of health utilization came to exceed the capacity of the healthcare workforce.
14 Even before the COVID-19 pandemic, Korean HCWs were already suffering from heavy workload and the effect of the reformed nurse staffing policy on employment of nurses in Korea.
15
Screening centers in each hospital operated in various forms. When the explosive outbreak developed in early 2020, a key component of the Korean government’s response was to rapidly establish a widespread diagnostic capacity. Due to insufficient national guidelines according to each hospital’s circumstances, it was difficult to proceed with setting up a center and find the essential HCWs. At the beginning of the COVID-19 outbreak in Korea, only doctors collected respiratory specimens, however, at the time of this study, more than half of the hospitals were collecting respiratory specimens via trained nurses. Looking at the workforce of the screening centers, the total workforce on weekdays is nine on average. Additionally, many screening centers operate not only on weekdays, but also on Saturdays and even Sundays. During the infectious disease pandemic, it would be helpful if the government could help expand not only facilities or medical devices but also healthcare personnel.
HCWs were infected with COVID-19 due to accidental exposures to patients with COVID-19 inside or outside the hospital. After many hospitals were repeatedly closed and HCWs were quarantined in Korea, the PPE level was raised in all situations and locations in hospitals; however, since it is impossible to prevent all accidental exposures to SARS-Cov-2 outside the hospital, COVID-19 infections by HCWs continued to occur. In this study, HCWs were more often infected with COVID-19 due to accidental exposure inside or outside the hospital, not during the treatment process for patients with COVID-19. All four HCWs contracted COVID-19 while working in quarantine wards in the hospitals of Daegu city and Gyeongsangnam-do province at the beginning of the epidemic in early 2020. Based on the evidence of this study, current PPE recommendation for COVID-19 in Korea might be adequate. Since protecting HCWs from COVID-19 has posed a great importance to maintain fundamental patient care and healthcare system,
16 hence, daily monitoring of HCWs for COVID-19 associated symptoms and epidemic exposure risk is crucial in each hospitals.
This study had some limitations. This is a study on the domestic HCWs workforce during the response to the COVID-19 in Korea; therefore, it should be compared according to the medical environment of each country. Although this study numerically compared only the medical personnel required to cope with the COVID-19 outbreak, operating methods for workforce may vary widely from hospital to hospital; however, this study is valuable as it is the first study to describe the workforce and burden of medical personnel during an infectious disease pandemic.
Korea Disease Control and Prevention Agency, experts in infectious diseases, pulmonology, emergency medicine, laboratory medicine, infection control department of each hospital and various healthcare providers are still striving to overcome the outbreak of COVID-19. The dedication of HCWs has helped them cope with the COVID-19 pandemic so far. We do not know when the pandemic will end; however, it seems that the current countermeasures need to be continued for a while. This study consistently shows that there is a need to supplement more sufficient medical personnel. To do this, it is necessary to take measures by sustainable medical personnel based on national policies; a direct financial support from NHI for medical personnel mobilized in crisis situations, a system that can mobilize medical personnel in cases of emergency and a continuous recruiting health care professionals in order to support patient and infection control, etc.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download