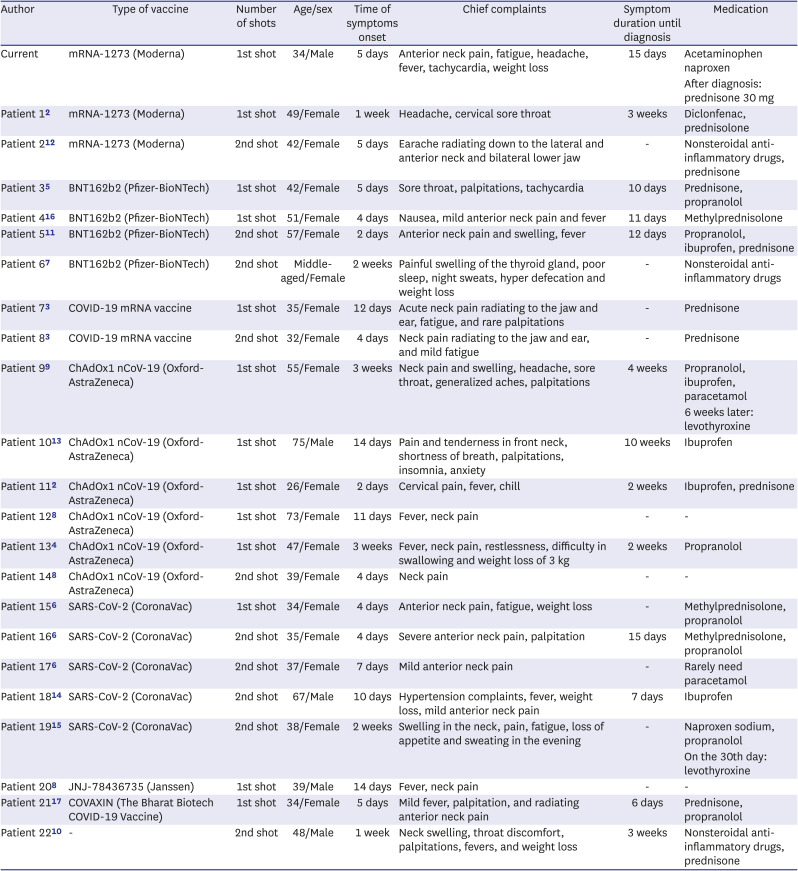
1. Bragazzi NL, Hejly A, Watad A, Adawi M, Amital H, Shoenfeld Y. ASIA syndrome and endocrine autoimmune disorders. Best Pract Res Clin Endocrinol Metab. 2020; 34(1):101412. PMID:
32265102.
2. Bornemann C, Woyk K, Bouter C. Case report: two cases of subacute thyroiditis following SARS-CoV-2 vaccination. Front Med (Lausanne). 2021; 8:737142. PMID:
34504856.
3. Chatzi S, Karampela A, Spiliopoulou C, Boutzios G. Subacute thyroiditis after SARS-CoV-2 vaccination: a report of two sisters and summary of the literature. Hormones (Athens). 2021; 1–3. PMID:
32827123.
4. Das L, Bhadada SK, Sood A. Post-COVID-vaccine autoimmune/inflammatory syndrome in response to adjuvants (ASIA syndrome) manifesting as subacute thyroiditis. J Endocrinol Invest. 2021; 1–3.
5. Franquemont S, Galvez J.. Subacute thyroiditis after mRNA vaccine for COVID-19. J Endocr Soc. 2021; 5(Suppl 1):A956–A957.
6. İremli BG, Şendur SN, Ünlütürk U. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine: postvaccination ASIA syndrome. J Clin Endocrinol Metab. 2021; 106(9):2600–2605. PMID:
34043800.
7. Jeeyavudeen MS, Patrick AW, Gibb FW, Dover AR. COVID-19 vaccine-associated subacute thyroiditis: an unusual suspect for de Quervain's thyroiditis. BMJ Case Rep. 2021; 14(11):e246425.
8. Lee KA, Kim YJ, Jin HY. Thyrotoxicosis after COVID-19 vaccination: seven case reports and a literature review. Endocrine. 2021; 74(3):470–472. PMID:
34637073.
9. Oyibo SO. Subacute thyroiditis after receiving the adenovirus-vectored vaccine for coronavirus disease (COVID-19). Cureus. 2021; 13(6):e16045. PMID:
34235030.
10. Patel KR, Cunnane ME, Deschler DG. SARS-CoV-2 vaccine-induced subacute thyroiditis. Am J Otolaryngol. 2022; 43(1):103211. PMID:
34534760.
11. Schimmel J, Alba EL, Chen A, Russell M, Srinath R. Letter to the editor: thyroiditis and thyrotoxicosis after the SARS-CoV-2 mRNA vaccine. Thyroid. 2021; 31(9):1440. PMID:
34030467.
12. Plaza-Enriquez L, Khatiwada P, Sanchez-Valenzuela M, Sikha A. A case report of subacute thyroiditis following mRNA COVID-19 vaccine. Case Rep Endocrinol. 2021; 2021:8952048. PMID:
34777881.
13. Ratnayake GM, Dworakowska D, Grossman AB. Can COVID-19 immunisation cause subacute thyroiditis? Clin Endocrinol (Oxf). Forthcoming 2021. DOI: 10.1111/cen.14555.
14. Şahin Tekin M, Şaylısoy S, Yorulmaz G. Subacute thyroiditis following COVID-19 vaccination in a 67-year-old male patient: a case report. Hum Vaccin Immunother. 2021; 17(11):4090–4092. PMID:
34196589.
15. Saygılı ES, Karakilic E. Subacute thyroiditis after inactive SARS-CoV-2 vaccine. BMJ Case Rep. 2021; 14(10):e244711.
16. Siolos A, Gartzonika K, Tigas S. Thyroiditis following vaccination against COVID-19: report of two cases and review of the literature. Metabol Open. 2021; 12:100136. PMID:
34693241.
17. Soltanpoor P, Norouzi G. Subacute thyroiditis following COVID-19 vaccination. Clin Case Rep. 2021; 9(10):e04812. PMID:
34631062.
18. Desailloud R, Hober D. Viruses and thyroiditis: an update. Virol J. 2009; 6(1):5. PMID:
19138419.
19. Ohsako N, Tamai H, Sudo T, Mukuta T, Tanaka H, Kuma K, et al. Clinical characteristics of subacute thyroiditis classified according to human leukocyte antigen typing. J Clin Endocrinol Metab. 1995; 80(12):3653–3656. PMID:
8530615.
20. Watad A, David P, Brown S, Shoenfeld Y. Autoimmune/inflammatory syndrome induced by adjuvants and thyroid autoimmunity. Front Endocrinol (Lausanne). 2017; 7:150. PMID:
28167927.
21. Brancatella A, Ricci D, Viola N, Sgrò D, Santini F, Latrofa F. Subacute thyroiditis after Sars-COV-2 infection. J Clin Endocrinol Metab. 2020; 105(7):dgaa276. PMID:
32436948.
22. Ruggeri RM, Campennì A, Siracusa M, Frazzetto G, Gullo D. Subacute thyroiditis in a patient infected with SARS-COV-2: an endocrine complication linked to the COVID-19 pandemic. Hormones (Athens). 2021; 20(1):219–221. PMID:
32676935.
23. Chakravarthy K, Strand N, Frosch A, Sayed D, Narra LR, Chaturvedi R, et al. Recommendations and guidance for steroid injection therapy and COVID-19 vaccine administration from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2021; 14:623–629. PMID:
33716511.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download