Abstract
Congenital sialo-cutaneous fistula arising from the accessory parotid gland is extremely rare. Although the fistula tract can be successfully excised after making a skin incision along the skin tension line around the fistula opening, a facial scar inevitably remains. We here report a case of sialo-cutaneous fistula that was treated with chemocauterization with trichloroacetic acid (TCA). TCA cauterization is an easy and effective option for the treatment of congenital fistula from an accessory parotid gland, especially from the aesthetic point of view.
The accessory parotid gland, or the accessory parotid, is a nodule of normal salivary tissue that is separate from the main parotid gland and it is located on the masseter muscle, and it is connected to Stensen's duct at that level (1). Although accessory parotid gland is a common variation (2), a fistula from an accessory parotid gland to the facial skin is extremely rare (3, 4). It was reported that congenital fistula from an accessory parotid gland could be diagnosed with performing CT sialography or CT fistulography (5).
We report a case of congenital fistula arising from an accessory parotid gland and it was treated by chemocauterization of the fistula with trichloroacetic acid (TCA), and this was accompanied with a botulinum toxin injection to the accessory gland parenchyma.
A 1-yr-old girl presented with a salivary discharge at the facial skin of her right cheek. CT sialography was done and a sialo-cutaneous fistula from an accessory parotid gland was diagnosed (Fig. 1). She also had a skin tag on the tragus of the right ear. At that time, surgical excision was considered at a later age. At the age of five, she visited the outpatient clinic for definitive treatment. The clinical examination demonstrated a 1 mm-sized opening located at the facial skin 1 cm lateral to the angle of mouth. The salivary discharge was clear and serous. The salivary flow rate was calculated by a cotton ball test. It revealed that the flow from the accessory gland was about 10% of the total flow of a parotid gland. According to our previous experience (5), fistulectomy was scheduled, but aesthetic considerations for the young girl made the surgical plan change to more conservative management. Under general anesthesia, the 6 cm-long fistula tract was identified with a lacrimal probe. Intraoperative ultrasonography was done to demarcate the accessory parotid gland. Although the accessory gland was too small to be clearly identified, 16 IU of botulinum toxin was injected to the accessory gland under ultrasound guidance. After thin adhesive film was attached on the buccal skin around the fistula opening to prevent spillage of corrosive agent from unwanted skin injury, about 2 mL of 40% TCA solution was injected into the tract with a small metal suction tip (Fig. 2). Thirty seconds later, all the solution was removed with suction and squeezing. This procedure of TCA cauterization was repeated twice. There was no immediate complication postoperatively.
After several days, a tensely inflated sialocele formed and the opening was found to be completely closed up. Aspiration was done with long subcutaneous tunneling from behind so as not to make an iatrogenic sialo-cutaneous fistula. After 4 sessions of weekly aspiration, the sialocele did not recur. During one year follow-up, there was no more salivary leakage or sialocele. Moreover, the aesthetic result was very satisfactory.
Because congenital fistula from an accessory parotid gland is a very rare condition, there is no proven treatment of choice for this type of lesion. There is a case report that a fistula was managed by open translocation to the oral cavity using Delore's method (3).
In our previous experience (5), a 5-yr-old girl with a congenital cutaneous fistula from an accessory parotid gland was successfully treated with excision of the accessory parotid gland and duct. Although the skin incision was performed along the skin tension line, a scar on the face inevitably remained.
To prevent facial scarring, TCA chemocauterization of the fistula tract was considered. TCA is a potent cauterizing agent that has been used for chemical peeling and the treatment of papilloma. What we use in practice is neutralized by the serum and it is systemically non-toxic. We have performed cases of TCA cauterization for the treatment of pyriform sinus fistula, and we reported on its feasibility (6). TCA permeates into the fistula and makes it possible to close the entire fistula tract.
In this case, the fistula opening was obliterated with TCA cauterization in the early postoperative days. This might have happened because granulation tissues and necrotic tissue debris from injured epithelium of the tract blocked the relatively long fistulous tract.
Botulinum toxin injection to minimize salivary secretion (7) was thought to be ineffective in this case because of the difficulty in demarcating the small accessory parotid gland. Although sialocele occurred repeatedly, it was controlled completely with repeated aspiration for about one month. It might be very important to make a long subcutaneous tunnel while aspirating the accumulated saliva not to make a new uncontrollable sialo-cutaneous fistula.
TCA solution is a well known chemical peeling agent. The level 35-50% TCA is the spectrum of medium-depth peeling, and 45% or 50% TCA corresponds to a wounding level of mid to deep reticular dermis (8). So it would be hardly possible for 40% TCA to penetrate the epithelialized fistulous tract and to injure the nerves and vessels.
In conclusion, TCA cauterization is an easy and effective option for the treatment of congenital fistula from the accessory parotid gland, especially from the aesthetic point of view.
References
1. Currarino G, Votteler TP. Lesions of the accessory parotid gland in children. Pediatr Radiol. 2006; 1. 36(1):1–7. PMID: 16284760.

2. Frommer J. The human accessory parotid gland: its incidence, nature, and significance. Oral Surg Oral Med Oral Pathol. 1977; 5. 43(5):671–676. PMID: 266146.

3. Yamasaki H, Tashiro H, Watanabe T. Congenital parotid gland fistula. Int J Oral Maxillofac Surg. 1986; 8. 15(4):492–494. PMID: 3091733.

4. Jernstrom P, Prietto CA. Accessory parotid gland tissue at base of neck. Arch Pathol. 1962; 6. 73:473–480. PMID: 14451707.
5. Moon WK, Han MH, Kim IO, Sung MW, Chang KH, Choo SW, et al. Congenital fistula from ectopic accessory parotid gland: diagnosis with CT sialography and CT fistulography. AJNR Am J Neuroradiol. 1995; 4. 16(4 Suppl):997–999. PMID: 7611095.
6. Kim KH, Sung MW, Koh TY, Oh SH, Kim IS. Pyriform sinus fistula: management with chemocauterization of the internal opening. Ann Otol Rhinol Laryngol. 2000; 5. 109(5):452–456. PMID: 10823473.

7. Ellies M, Laskawi R, Rohrbach-Volland S, Arglebe C, Beuche W. Botulinum toxin to reduce saliva flow: selected indications for ultrasound-guided toxin application into salivary glands. Laryngoscope. 2002; 1. 112(1):82–86. PMID: 11802043.

Fig. 1
Initial findings of CT-sialography. (A-D) Fistula tract from the outside opening of the right anterior cheek to the accessory gland at the anterior aspect of the right parotid gland.
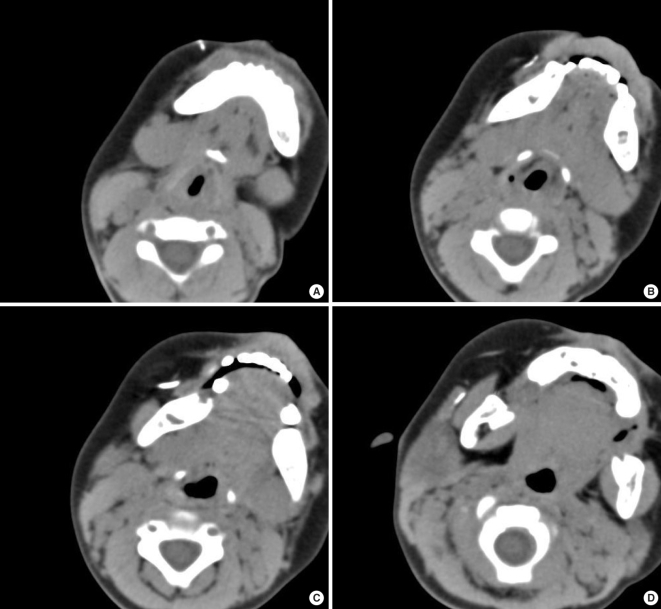
Fig. 2
Chemocauterization of a sialo-cutaneous fistula with trichloroacetic acid (TCA) solution. (A) Intraoperative findings. A small metal suction tip was inserted through the fistula opening. A lacrimal probe, held by a surgeon, indicated the end of the suction tip. The length of the fistula tract was about 6 cm. Two mL of 40% TCA solution was injected for chemocauterization of the tract. (B) Postoperative findings after 2 month. The fistula opening was completely closed and only a small dimple remained. The cosmetic result was very satisfactory.





 Citation
Citation Print
Print


 XML Download
XML Download