Abstract
Objectives
Vascular tinnitus is the most common form of pulsatile tinnitus, particularly when the tinnitus corresponds with the pulse of patients. In this study, we reviewed the 10-year clinical data on vascular tinnitus of our tinnitus clinic to investigate the frequency of the underlying etiologies, to introduce a diagnostic protocol, and to evaluate the treatment outcomes.
Methods
We retrospectively collected the data of 57 patients who were diagnosed as vascular tinnitus between April 2001 and December 2011. Careful history taking, otoscopy, thorough physical examinations, audiometry, laboratory tests, as well as radiologic examinations were performed according to our diagnostic protocol to find the origin of pulsatile tinnitus. Treatment options were individualized based on the specific etiology, and the outcomes were assessed using patient's subjective reports at the follow-up interviews.
Results
High jugular bulb was the most common cause (47.4%) of vascular tinnitus, and venous hum was the next (17.5%). Dural arteriovenous fistula, intracranial aneurysm, atherosclerotic carotid artery disease, and hypertension were less common causes. Vascular tinnitus was alleviated in most patients after the appropriate treatment: surgical intervention, tinnitus retraining therapy, reassurance, and medications.
Conclusion
Vascular tinnitus can be successfully diagnosed by the regular use of the suggested protocol. Many patients with vascular tinnitus have treatable underlying etiologies. Treatment of those etiologies or at least counseling about the tinnitus itself can benefit the patients with troublesome vascular tinnitus.
Vascular tinnitus is the most common form of pulsatile tinnitus, especially when the sound corresponds well with the patient's pulse. Vascular tinnitus is an uncommon otologic symptom; the incidence has been reported to be approximately 4% in patients with tinnitus [1]. It originates from vascular etiologies and may occur by the result of turbulence in the blood flow. The sound produced by the turbulence is transmitted to the inner ear and causes tinnitus percept. According to the vascular structures of origin, vascular tinnitus can be classified as arterial or venous type [2]. In the clinical practice of treating tinnitus patients, the diagnosis of vascular tinnitus is challenging due to its rarity and no standardized diagnostic protocol. Therefore, the otolaryngologist is likely to misdiagnose it as idiopathic subjective tinnitus. Because significant intracranial conditions can evoke vascular tinnitus, a diagnostic failure may lead to a serious outcome.
In the present study, we summarized the 10-year data on vascular tinnitus of our tinnitus clinic to investigate the frequency of the underlying etiologies, to introduce a diagnostic protocol, and to evaluate the treatment outcomes.
The clinical data on 57 patients with pulsatile tinnitus who presented to our tinnitus clinic between April 2001 and December 2011 were retrospectively reviewed by a single tinnitus specialist (SNP). This study was approved by the Institutional Review Board of Seoul St. Mary's Hospital (KC12RISE0250).
A detailed history of pulsatile tinnitus was taken, and the standardized interview form and validated tinnitus questionnaires were administered to the patients to score the subjective tinnitus severity. These self-rating scores included awareness (AW, percent of time aware of tinnitus during the waking hours), 10-point visual analogue scale for tinnitus loudness (LD)/annoyance (AN)/effect on daily life (EOL), and tinnitus handicap inventory (THI). The initial diagnostic approach depended primarily on the tinnitus quality described by the patient. A throbbing, rushing, or humming sound suggested a vascular etiology. Thorough physical examinations were performed through otoscopy, auscultation of the ear canals, and a full head and neck examination. A tympanic mass could be visible on otoscopy. When the patient showed a normal eardrum with bruits on the auscultation around the head and neck area, the patient's pulse was checked if it was synchronous with the tinnitus sound. To discriminate the vascular structures of origin, the ipsilateral internal jugular vein (IJV) was gently compressed and any changes in tinnitus loudness were examined. Head turning test was also conducted to confirm the compression maneuver. In tinnitus of venous origin, light digital pressure over the ipsilateral IJV or head turning towards the tinnitus side allowed tinnitus to diminish or subside. When those maneuvers exerted no effect on tinnitus loudness, tinnitus of arterial origin was suspected.
All patients underwent pure tone audiometry, speech audiometry, and tinnitogram. Pure tone average (PTA) was determined at 0.5, 1, 2, and 3 kHz. We defined the hearing as low-frequency hearing loss when the low tone average at 125, 250, and 500 Hz was ≥20 dB higher than the high tone average at 1, 2, and 3 kHz. Blood pressure was measured to rule out hypertension, and blood tests were performed to exclude anemia and hyperthyroidism, which could increase cardiac output and cerebral blood flow.
In patients with a tympanic mass medial to the eardrum, temporal bone computed tomography (TBCT) and/or magnetic resonance imaging were obtained to demonstrate jugular bulb anomalies, glomus tumor, and the other tumorous lesions. In case of a glomus tumor, carotid angiography was also conducted to evaluate the cerebral collateral circulation as well as for embolization of the feeding artery before surgical removal. If the otoscopic finding was normal, and the venous or arterial origin could be differentiated by the physical maneuver, various imaging studies-TBCT, brain magnetic resonance angiography/venography (MRA/MRV), and transcranial Doppler sonography (TCD)-were performed subsequently to find the specific etiologies.
In patients with potential venous-origin vascular tinnitus, TBCT was the first choice to detect venous anomalies. Once jugular bulb anomaly was diagnosed, no further imaging study was not performed. Otherwise, MRV was additionally obtained to exclude the other vascular or intracranial pathology. In cases of normal imaging, we consulted a neurologist to exclude benign intracranial hypertension (BIH). When BIH was excluded by the neurologist, we finally diagnosed the tinnitus as venous hum.
In patients with potential arterial-origin vascular tinnitus, TCD was the first choice along with MRA or brain CT angiography. Atherosclerotic carotid artery disease (ACAD), dural arteriovenous fistula (AVF), and intracranial aneurysm could be found through these tests. In cases of normal imaging, we diagnosed the tinnitus as idiopathic. The flow chart is presented in Fig. 1. We provided the patients with appropriate treatment according to the specific etiology and tinnitus severity. The treatment options included surgical intervention, tinnitus retraining therapy (TRT), reassurance, and medications. The outcomes were assessed using patient's subjective reports at the follow-up interviews.
Of the total 57 patients (10 males and 47 females; age range, 18 to 85 years; mean age, 48.9 years) included, high jugular bulb was the most common cause (27 patients) of vascular tinnitus followed by venous hum (10 patients), dural AVF (5 patients), ACAD (4 patients), hypertension (4 patients), and intracranial aneurysm (3 patients) (Table 1). The mean duration was 25.9 months. Tinnitus was unilateral in 55 patients, and bilateral in two. The left ear was affected in 23 patients and the right in 32 patients. A female predominance was clearly observed in vascular tinnitus. Interestingly, there was no male patient who had venous hum or hypertension-related vascular tinnitus in our case series. High jugular bulb involved the right ear three times more frequently than the left.
The mean PTA of all patients was 18.8±12.2 dB (mean±standard deviation). In only one patient with high jugular bulb, air-bone gap of 30 dB was found in the affected ear. In tinnitogram, the mean tinnitus loudness was 31.0±19.7 dB (range, 6 to 90 dB); the mean pitch, 1,883±3,108 Hz (range, 125 to 8,000 Hz). Although the mean pitch was in the high frequency range, the low pitch was predominant except 1,000-3,000 Hz: 125, 250, 500, 4,000, 6,000, and 8,000 Hz was reported by 51.7%, 10.4%, 13.8%, 3.4%, 3.4%, and 17.2% of patients, respectively. Low-frequency hearing loss was shown in 38%/50%/60%/25%/75% in patients with high jugular bulb/venous hum/AVF/ACAD/hypertension, which may be related with the acoustic characteristics of vascular tinnitus. The mean tinnitus severity scores are as follows: AW, LD, AN, EOL, and THI was 60.6±30.5, 5.2±2.4, 5.6±2.5, 4.9±2.5, and 39.5±18.6, respectively. The subdivided data according to the main etiologies are exhibited in Table 2.
In patients with high jugular bulb, TRT was the first-line treatment after the control of newly developed hypertension if any. The components of TRT contained demonstration of the high jugular bulb on CT scan, directive counseling based on the Jastreboff neurophysiological model, and instructions to use enriched environmental sound or sound generators. The sound generators were required in only one patient who were bothered by severe tinnitus even with the environmental sound enrichment. This patient improved after instrumentation. The intractable tinnitus patients were treated with surgical ligation of the IJV showing favorable outcomes. All patients with venous hum were treated with TRT and medications, and most patients showed improvement. Dural AVF and intracranial aneurysms were detected in eight patients. Six of them were relieved of tinnitus completely after embolization, and in two patients, tinnitus was alleviated by TRT with medications during the observational period of the vascular lesion. Hypertension was diagnosed in four patients, who showed improvement after adequate blood pressure control. ACAD was observed in four patients; one of them was cured of tinnitus with angioplasty, and three showed improvement after TRT with medication. In one patient with glomus tympanicum, complete resolution was achieved by surgical removal. The patients who had rare causes of vascular tinnitus in our case series-a cavernous hemangioma located in an inoperable site within the brain, aberrant carotid artery, and BIH-underwent TRT with medications, and showed gradual improvement after the treatment. Long-term follow-up was not needed in most of the patient. The patients who were followed within 6 months were 77.2%. The treatment modalities and outcomes in all cases are summarized in Table 3.
In this study, we have summarized the data of our large case series of vascular tinnitus to provide the practitioners with some helpful information about the diagnosis and treatment of this challenging symptom in otology clinics. It is suggested that imaging studies are particularly important in the diagnostic process of vascular tinnitus. When venous origin was suspected, TBCT should be checked first to rule out the most common jugular bulb anomalies. If arterial origin was suspected, TCD along with MRA should be obtained. TCD was useful to evaluate the functional degree of intracranial vascular stenosis, especially ACAD. In addition, consultation with neurologists or neurosurgeons is frequently critical in vascular tinnitus. Because tinnitus patients who first visit otolaryngology clinics usually do not have identifiable neurologic signs and symptoms, high index of suspicion is needed. For example, before a neurologic consultation for BIH, other presenting symptoms such as headache, dizziness, and visual disturbances also require careful attention.
In our case series, high jugular bulb was the most common cause of vascular tinnitus, and the second, venous hum. Arterial causes were less common. Glomus tympanicum, intracranial cavernous hemangioma, aberrant carotid artery, and BIH were identified in only one case, each. Sismanis reported a 15-year study of 145 patients with vascular tinnitus [3]. In his study, BIH was the most common diagnosis (56 patients) followed by ACAD (24 patients). It has been reported that the incidence of BIH is increased in women who are 10% or more over ideal weight [4], and varies according to the prevalence of obesity in the respective region [5]. In our study, the incidence of BIH was very low; only one patient among 54 patents. These different incidences may be attributed to the different patient populations. Furthermore, the chief complaint of our patients is almost always tinnitus, not neurologic symptoms. If we collaborate with neurologists for the study, more intriguing data would be available on vascular tinnitus caused by intracranial vascular anomalies.
High jugular bulb has been defined as a jugular bulb extending above the inferior bony annulus [6]. The incidence of high jugular bulb has been reported from 3.5% to 22.6% [7]. High jugular bulb is usually asymptomatic, but when symptoms are present, tinnitus is known to be a common complaint [8]. The initial treatment method for high jugular bulb could be TRT, medication, and sound therapy [9]. In cases of the failure of initial treatment, surgical therapy can be considered. Surgical treatment options for high jugular bulb include jugular vein ligation, transcatheter endovascular coil embolization, transvenous stent-assisted coil embolization, surgical lowering through subfacial and infralabyrinthine approaches, and surgical covering and reinforcement using fascia, perichondrium, or autologous cartilage [10,11,12,13,14]. However, surgical outcomes of these methods were not sufficient to be considered as successful, and have not been evaluated properly. Moreover, potential complications of the surgery are intracranial hypertension, facial nerve injury, and conductive hearing loss. Thus, the surgery is not recommended as an initial therapy for tinnitus patients caused by high jugular bulb [9]. The authors initially provided our patients with TRT and medications: alprazolam (0.25 mg) and ginkgo biloba extract (80 mg) daily for 3 months. In only two cases among the 27 high jugular bulb patients, failure of the conservative treatment leaded to IJV ligation. One showed complete relief of tinnitus, and the other showed partial improvement.
Venous hum can be defined as an idiopathic vascular tinnitus of venous origin [15,16,17]. It is common in patients between 20 and 40 years with a marked female preponderance. A turbulent blood flow produced in the IJV is supposed to be the cause of venous hum [18]. Diagnosis of venous hum can only be made after the exclusion of the other disorders. In our clinic, all patients with this second most common cause of vascular tinnitus were treated with TRT and medication, because surgical treatment of venous hum has not been popular to date. The treatment responses were good in 80% of the patients, although no one showed complete cure. Dural AVF and aneurysm are relatively common intracranial vascular abnormalities. Tinnitus can be one of the most frequent symptoms in dural AVF. Cerebral venous thrombosis has been proposed to be the major pathogenic factor in the formation of dural AVF. As the thrombosed segment recanalizes, regeneration of dural arteries results in artery-to-sinus anastomosis. In a recent report, the overall mortality rate was 4.8% within the first 12 months [19]. An aneurysm is a focal dilatation of an arterial vessel caused by high blood pressure, shearing forces, turbulence, and morphological or biological characteristics within the vessel wall [20,21,22]. Overall prevalence was estimated to be 3.2% in a population with a mean age of 50 years [23]. Aneurysm of the internal carotid artery, particularly in the petrous portion, can manifest with pulsatile tinnitus alone [24]. Because the lesion is life-threatening when ruptured, interventions such as surgical clipping or endovascular coiling should be conducted if indicated. In our cases, all tinnitus patients with aneurysms were treated with embolization, and the pulsatile tinnitus was cured immediately after the treatment.
In conclusion, vascular tinnitus could be alleviated or cured in most of the patients after the individualized treatment according to the causes. Many patients with vascular tinnitus have treatable underlying etiologies. We suggest that establishing the correct diagnosis through a regular diagnostic protocol and early selected treatment will help patients to be relieved from their tinnitus effectively.
References
1. Stouffer JL, Tyler RS. Characterization of tinnitus by tinnitus patients. J Speech Hear Disord. 1990; 8. 55(3):439–453. PMID: 2381186.

2. Liyanage SH, Singh A, Savundra P, Kalan A. Pulsatile tinnitus. J Laryngol Otol. 2006; 2. 120(2):93–97. PMID: 16359136.

3. Sismanis A. Pulsatile tinnitus: A 15-year experience. Am J Otol. 1998; 7. 19:472–477. PMID: 9661757.
4. Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumour cerebri: Population studies in Iowa and Louisiana. Arch Neurol. 1988; 8. 45(8):875–877. PMID: 3395261.
5. Radhakrishnan K, Thacker AK, Bohlaga NH, Maloo JC, Gerryo SE. Epidemiology of idiopathic intracranial hypertension: a prospective and case-control study. J Neurol Sci. 1993; 5. 116(1):18–28. PMID: 8509801.

6. Overton SB, Ritter FN. A high placed jugular bulb in the middle ear: a clinical and temporal bone study. Laryngoscope. 1973; 12. 83(12):1986–1991. PMID: 4772103.

7. Subotic R. The high position of jugular bulb. Acta Otolaryngol. 1979; Mar-Apr. 87(3-4):340–344. PMID: 443015.
8. Weiss RL, Zahtz G, Goldofsky E, Parnes H, Shikowitz MJ. High jugular bulb and conductive hearing loss. Laryngoscope. 1997; 3. 107(3):321–327. PMID: 9121306.

9. Yoo HJ, Park SN, Kim DK, Park KH, Kim MJ, Kim JE. Incidence and clinical characteristics of patients with tinnitus according to diagnostic classification. Korean J Otorhinolaryngol-Head Neck Surg. 2011; 6. 54(6):392–398.

10. Huang BR, Wang CH, Young YH. Dehiscent high jugular bulb: a pitfall in middle ear surgery. Otol Neurotol. 2006; 10. 27(7):923–927. PMID: 16788425.
11. Buckwalter JA, Sasaki CT, Viraponse C. Pulsatile tinnitus arising from jugular megabulb deformity: a treatment rationale. Laryngoscope. 1983; 12. 93(12):1534–1539. PMID: 6645753.

12. Yoon BN, Lee TH, Kong SK. Management of high jugular bulb with tinnitus: transvenous stent-assisted coil embolization. Otolaryngol Head Neck Surg. 2008; 11. 139(5):740–741. PMID: 18984278.

13. Couloigner V, Grayeli AB, Bouccara D, Julien N, Sterkers O. Surgical treatment of the high jugular bulb in patients with Meniere's disease and pulsatile tinnitus. Eur Arch Otorhinolaryngol. 1999; 256(5):224–229. PMID: 10392295.
14. Kondoh K, Kitahara T, Mishiro Y, Okumura S, Kubo T. Management of hemorrhagic high jugular bulb with adhesive otitis media in an only hearing ear: transcatheter endovascular embolization using detachable coils. Ann Otol Rhinol Laryngol. 2004; 12. 113(12):975–979. PMID: 15633900.

15. Arenberg IK, McCreary HS. Objective tinnitus aurium and dural arteriovenous malformations of the posterior fossa. Ann Otol Rhinol Laryngol. 1971; 2. 80(1):111–120. PMID: 5100337.

16. Chandler JR. Diagnosis and cure of venous hum tinnitus. Laryngoscope. 1983; 7. 93(7):892–895. PMID: 6865626.

17. Engstrom H, Graf W. On objective tinnitus and its recording. Acta Otolaryngol Suppl. 1950; 95:127–137. PMID: 14884974.

18. Hentzer E. Objective tinnitus of vascular type: A follow-up study. Acta Otolaryngol. 1968; 10. 66(4):273–281. PMID: 5734496.
19. Piippo A, Laakso A, Seppa K, Rinne J, Jaaskelainen JE, Hernesniemi J, et al. Early and long-term excess mortality in 227 patients with intracranial dural arteriovenous fistulas. J Neurosurg. 2013; 7. 119(1):164–171. PMID: 23600937.

20. Hashimoto T, Meng H, Young WL. Intracranial aneurysms: Links among inflammation, hemodynamics and vascular remodeling. Neurol Res. 2006; 6. 28(4):372–380. PMID: 16759441.

21. Mizutani T, Kojima H, Asamoto S, Miki Y. Pathological mechanism and three-dimensional structure of cerebral dissecting aneurysms. J Neurosurg. 2001; 5. 94(5):712–717. PMID: 11354401.

22. Tulamo R, Frosen J, Hernesniemi J, Niemela M. Inflammatory changes in the aneurysm wall: a review. J Neurointerv Surg. 2010; 6. 2(2):120–130. PMID: 21990591.

23. Juvela S. Prevalence of risk factors for intracranial aneurysms. Lancet Neurol. 2011; 7. 10(7):595–597. PMID: 21641283.
24. Kim DK, Shin YS, Lee JH, Park SN. Pulsatile tinnitus as the sole manifestation of an internal carotid artery aneurysm successfully treated by coil embolization. Clin Exp Otorhinolaryngol. 2012; 9. 5(3):170–172. PMID: 22977715.

Fig. 1
Diagnostic algorithm for vascular tinnitus. TBCT, temporal bone computed tomography; TBMRI, temporal bone magnetic resonance imaging; HBP, hypertension; IJV, internal jugular vein; TN, tinnitus; MRA, magnetic resonance angiography; MRV, magnetic resonance venography; TCD, transcranial Doppler sonography; BIH, benign intracranial hypertension; ACAD, atherosclerotic carotid artery disease; AVF, arteriovenous fistula.
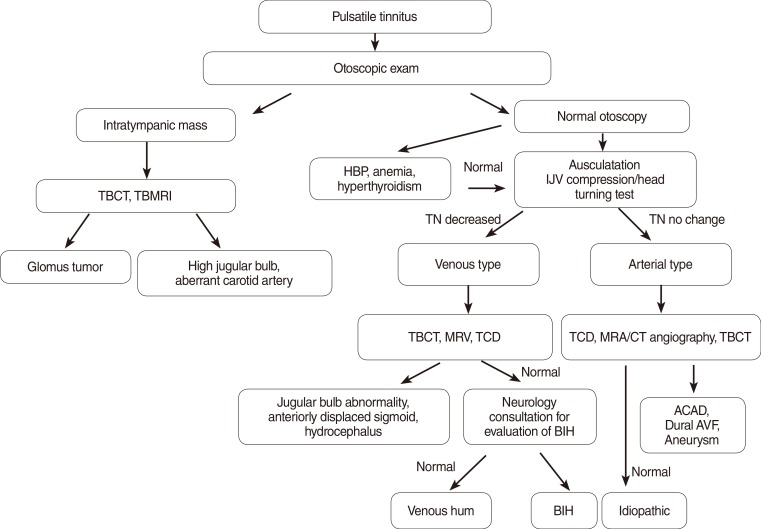
Table 1.
Relative frequency of the etiologies of vascular tinnitus
Table 2.
Demographic data and tinnitus severity scores in patients with 5 major etiologies of vascular tinnitus
Values are presented as mean±SD or number (%).
L, left; R, right; B, both; LFHL, low-frequency hearing loss; AW, awareness (percent of time aware of tinnitus during the waking hours); LD/AN/EOL, 10-point visual analogue scale for loudness/annoyance/effect on daily life; THI, tinnitus handicap inventory; DAVF, dural arteriovenous fistula; ACAD, atherosclerotic carotid artery disease.
Table 3.
Treatment options and outcomes for vascular tinnitus




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download