This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
Benzydamine is a nonsteroidal anti-inflammatory agents agent with anti-inflammatory and local anesthesia properties that is available in the entire world as an oral spray for oral mucositis patients who are suffering from radiation effects. The effect of benzydamine on oral mucositis in vivo is well known; however, the effect of the drug on tracheal smooth muscle has rarely been explored. During administration of the benzydamine for oral symptoms, it might affect the trachea via oral intake or inhalation.
Methods
We examined the effectiveness of benzydamine on isolated rat tracheal smooth muscle. The following assessments of benzydamine were performed: effect on tracheal smooth muscle resting tension; effect on contraction caused by 10-6M methacholine as a parasympathetic mimetic; and effect of the drug on electrically induced tracheal smooth muscle contractions.
Results
Addition of methacholine to the incubation medium caused the trachea to contract in a dose-dependent manner. Addition of benzydamine at doses of 10-5M or above elicited a significant relaxation response to 10-6M methacholine-induced contraction. Benzydamine could inhibit electrical field stimulation-induced spike contraction. It alone had a minimal effect on the basal tension of trachea as the concentration increased.
Conclusion
This study indicated that high concentrations of benzydamine might actually inhibit parasympathetic function of the trachea. Benzydamine might reduce asthma attacks in oral mucositis patients because it could inhibit parasympathetic function and reduce methacholine-induced contraction of tracheal smooth muscle.
Go to :

Keywords: Benzydamine, Anti-Inflammatory Agents, Non-Steroidal, Trachea, Smooth Muscle, In Vitro Study
INTRODUCTION
Benzydamine HCL (benzydamine) is an anti-inflammatory analgesic agent structurally unrelated to the steroid group. Benzydamine differs chemically from other nonsteroidal anti-inflammatory agents (NSAID) in that it is a base rather than an acid [
1,
2]. Animal models show that when administered systemically benzydamine is effective against pain and edema due to inflammatory conditions. It also inhibits granuloma formation [
1,
2]. At concentrations used for topical treatment, benzydamine possesses local anaesthetic action [
3,
4,
5]. During an asthmatic attack, the tracheal smooth muscle plays an important role in reducing pulmonary function as it becomes contracted. An asthma patient may also apply this drug for their mucositis. Hence, the effect of benzydamine oral spray on tracheal smooth muscle merits further exploration. The aim of this study was to determine the effects of benzydamine on isolated tracheal smooth muscle
in vitro.
Go to :

MATERIALS AND METHODS
Chemicals used were of the highest purity available. Commercial benzydamine oral spray (0.15%) was obtained through the courtesy of United Biomedical Co., Taiwan. All other chemical reagents were obtained from Sigma (St. Louis, MO, USA). We tested methacholine as a tracheal contraction drug. Eighteen rats were anesthetized by intraperitoneal administration of pentobarbital (45 mg/kg) and two pieces of trachea (~5 mm in length) were removed from each rat. This study was approved by an animal experiment review board (IACUC-07-133). The tracheal specimen was mounted using two steel plates and submersed in a 30-mL muscle bath at 37℃ as previously reported [
6,
7]. Briefly, the bath was filled with 30-mL Krebs solution consisting of (mmol/L): NaCl, 118; KCl, 4.7; CaCl
2, 2.5; MgSO
4·7H
2O, 1.2; KH
2PO
4, 1.2; NaHCO
3, 25.0; and glucose, 10.0. The upper side of the tracheal strip was attached to a Grass FT-03 force displacement transducer (AstroMed, West Warwick, RI, USA) by using a steel plate and a 3-0 silk ligature. The other side of the strip was fixed to a steel plate attached to the bath. A passive tension of 0.3 g was applied to the strips and subsequent changes in tension were recorded continuously using Chart V4.2 software (PowerLab, AD Instruments, Colorado Springs, CO, USA). Preliminary tests showed that the tracheal strip immersed in the bath solution used for subsequent experiments did not contract when basal tension was applied. Before drug assays were conducted, isolated tracheas were equilibrated in the bath solution for 15-30 minutes, during which they were continuously aerated with a mixture of 95% O
2 and 5% CO
2. Stepwise increases in the amount of drugs used were made to study contraction or relaxation responses of tracheal strips. All drugs were administered by adding a defined volume of stock solution to the tissue bath solution.
Electrical field stimulation (EFS) (5-Hz, 5-ms pulse duration, at 50 V, trains of stimulation for 5 seconds) was applied to the trachea strip with two wire electrodes placed parallel to the trachea strip and connected to a direct-current stimulator (Grass S44 Stimulator, Grass Medical Instruments, Quincy, MA, USA). An interval of 2 minutes was imposed between each stimulation period to allow recovery from the response. Stimulation was applied continuously to the trachea at 37℃.
The following assessments for benzydamine were performed: (1) effect on tracheal smooth muscle resting tension: this test was to examine the effect of the drug on the simulating condition of resting trachea condition; (2) effect on contraction caused by 10-6 M methacholine (a parasympathetic mimetic): this procedure was concerned with the examination of postsynaptic events such as muscle-receptor blockade, enhancement, and second messengers; and (3) effect of benzydamine on electrically induced contractions: electrical stimulation of this tissue causes parasympathetic nerve remnants in the trachea to release transmitter (acetylcholine). If there is interference with transmitter release, electrical stimulation does not cause contraction. Thus, presynaptic events were seen more easily with this procedure. The eighteen rats were equally divided into three groups. Two pieces of tracheal strip were removed from each rat. In the above assessments, twelve tracheal strips were used for each assessment. In each experiment, one untreated strip served as a control.
The concentrations of drugs were expressed as concentrations present in the 30-mL bath solution. Data were presented as mean values and standard deviations (SDs). Differences between mean values were compared using Student t-test. Differences were assumed to be significant at P<0.05.
Go to :

RESULTS
The degree of contraction or relaxation of tracheal strips was estimated from the tension applied to the transducer. Tracheal contraction induced by a small dose of methacholine was easily detected, and the tissue remained in a contracted state until the drug was rinsed from the tissue.
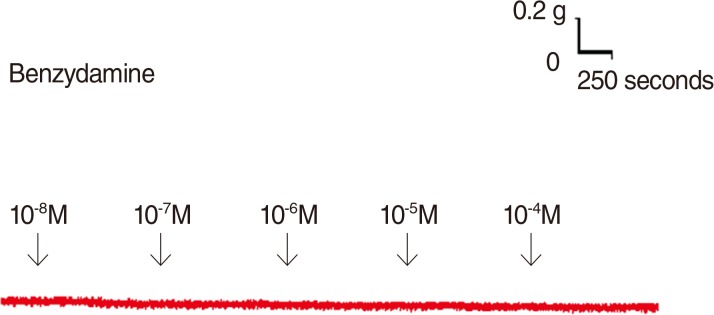
Addition of the benzydamine to the basal tension elicited a negligible effect (
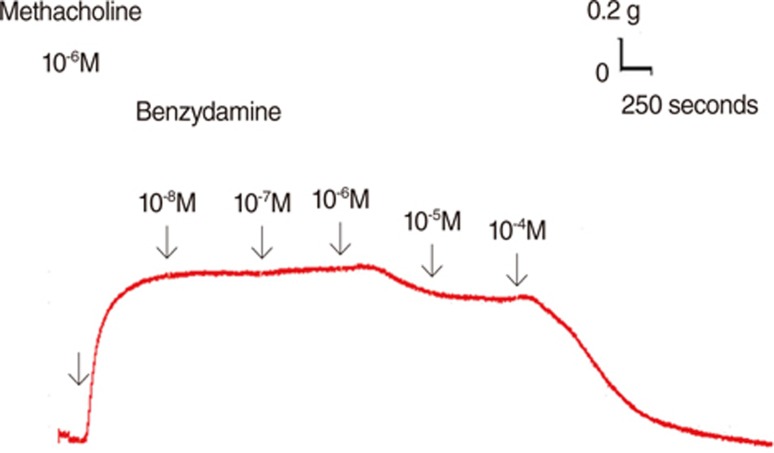
Fig. 1). It resulted in relaxation of the trachea when introduced after the addition of a constricting agent such as 10
-6M methacholine (
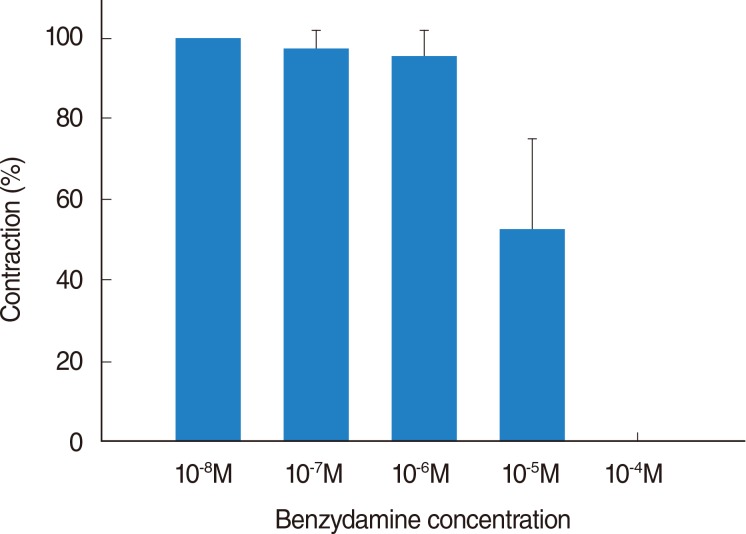
Fig. 2). Low doses of benzydamine resulted in a mild effect on contraction while higher doses relaxed significantly the trachea smooth muscle (
Figs. 2,
3). At 10
-8M benzydamine, the tension was 100% of the control values (
Fig. 3). At 10
-5M and 10
-4M benzydamine, the tensions were 52.9%±21.9% and 0, respectively (
Fig. 3). The difference in tension among the specimens treated with 10
-8M benzydamine and 10
-5M or 10
-4M benzydamine was statistically significant (
P<0.05).
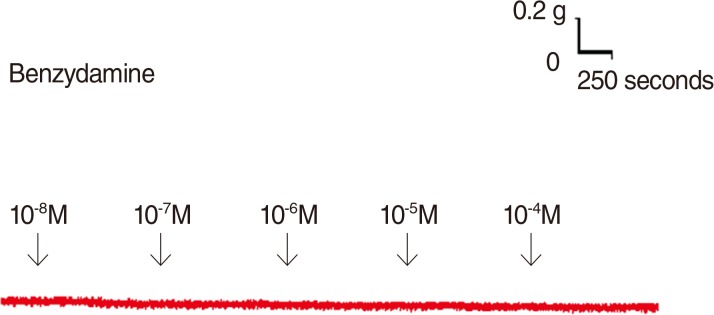 | Fig. 1Tension changes in rat trachea after application of various benzydamine concentrations. Benzydamine alone had a minimal effect on the basal tension of trachea as the concentration increased. Original basal tension was 0.3 g. 
|
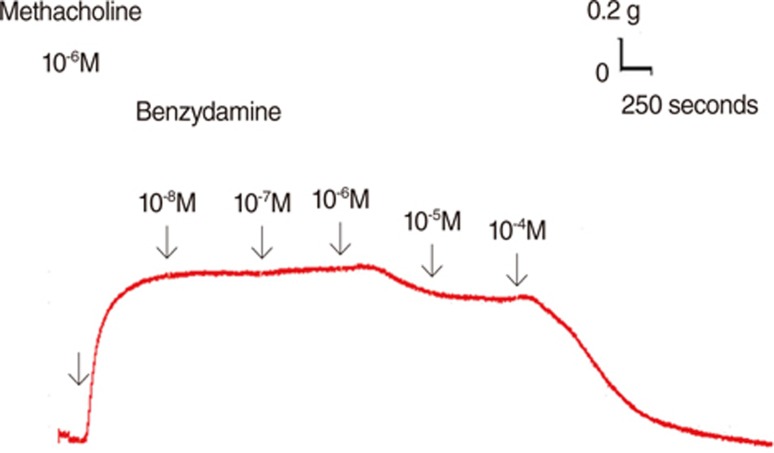 | Fig. 2Original recording of the effects of benzydamine on 10-6M methacholine-induced contraction of rat trachea. 
|
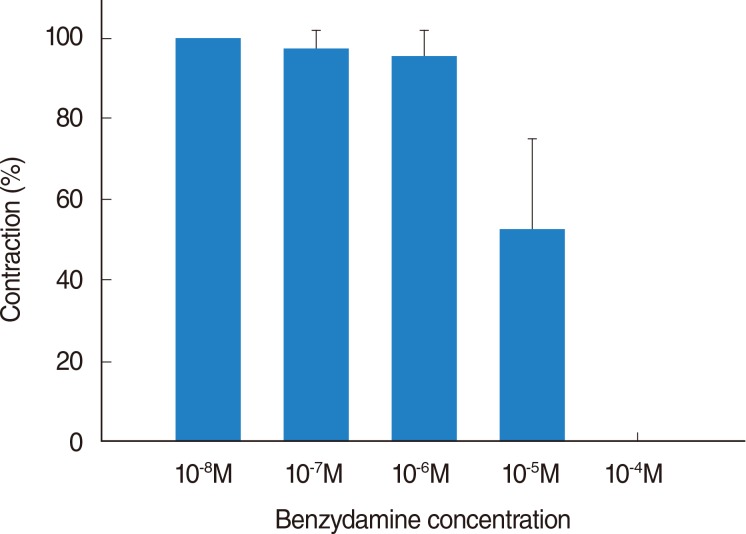 | Fig. 3Effects of benzydamine on 10-6M methacholine-induced contraction (contraction area calculated at 100% with no addition of benzydamine) of rat trachea. The difference in tension between 10-8M benzydamine and 10-5M benzydamine or 10-4M benzydamine was statistically significant (P<0.05). Results were mean±standard deviation (n=6). 
|
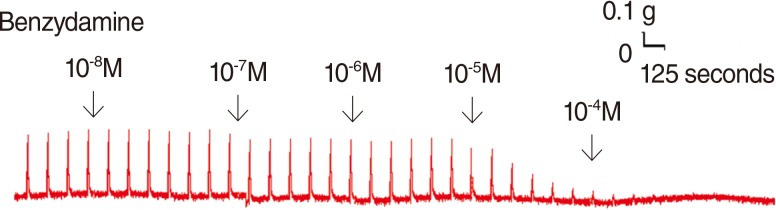
Benzydamine also inhibited the spike contraction induced by EFS (
Figs. 4,
5). The peak tension of the tracheal strip evoked by EFS upon the addition of 10
-8M benzydamine was 103.6%±3.2%, whereas at 10
-5M and 10
-4M benzydamine the peaks were 48.7%±19% and 8.9%±9.9%, respectively (
Fig. 5). The peak tension of the tracheal strip evoked by EFS at 10
-5M or 10
-4M benzydamine addition was significantly less than that at 10
-8M benzydamine (
P<0.05).
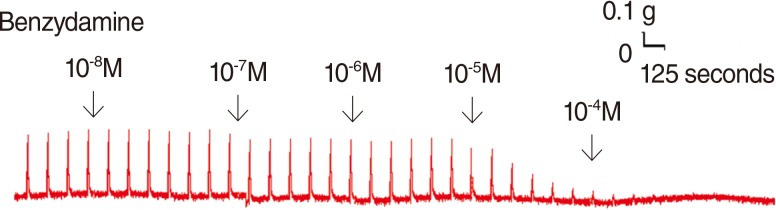 | Fig. 4Original recording of effects of benzydamine on electrically induced tracheal smooth muscle contractions was noted. Higher doses of benzydamine also decreased the spike contraction induced by electrical field stimulation. 
|
 | Fig. 5Effects of benzydamine on electrically induced tracheal smooth muscle contractions (contraction area calculated at 100% with no addition of benzydamine). The peak tension of the tracheal strip evoked by electrical field stimulation during the addition of 10-4M benzydamine was significantly less than that at the addition of 10-8M benzydamine (P<0.001). Results were mean±standard deviation (n=6). 
|
Go to :

DISCUSSION
This study was simple and effective. An intact tracheal ring was an important component of our technique [
8,
9]. An intact tracheal ring is much more representative of a physiological setting than smooth muscle strips. The results of our experiments should be interpreted within the context of the test materials used. Although it was difficult to determine which tissue component of the trachea was responsible for drug-induced contraction, the nature of specific tissues and their responses to specific drugs provided some indication. First, the tracheal strips used in our study were crude preparations that contained cartilage and tracheal smooth muscle. The smooth muscle of the trachea appeared to be the main tissue component responsible for contraction, as the other components (epithelium, glands, connective tissue, nerves, and cartilage) did not contract to a significant extent. Because this method involved cross contraction, changes in tension were caused by radial contraction of the tracheal ring. Although responses to drugs and electrical stimulation have been verified for similar preparations [
8,
9,
10], the contractile response observed in this study was probably an aggregate of the responses of various types of muscle tissue. Second, the isolated tracheal preparations used in our experiments were excised from rats without damaging the endothelium or smooth muscle. Therefore, it is reasonable to assume that tracheal responses to test agents in our study are comparable to those observed after application of a spray to the trachea during an asthmatic attack. It was not easy to obtain human tissue for similar studies. The effect of this drug on isolated human tracheal smooth muscle still needs further investigation. Because this was an
in vitro study, there were reservations as to its comparability with an
in vivo situation in humans. In the
in vivo situation, the response might be much more complicated than that in the
in vitro situation.
The cholinergic contracting agent tested in this preparation is commonly used for research purposes. It is noteworthy that benzydamine induced relaxation of tissue was dependent on prior partial contraction of smooth muscle after application of methacholine. Thus, it should be possible to assess the effects of common drugs and potential therapeutic agents supposedly responsible for relieving asthma attacks. Benzydamine, a NSAID agent, could reduce methacholine-induced contraction. Commercial oral spray contains 0.1% benzydamine, which is approximately 2×10-3M benzydamine. When applying a spray, one gets immediately dissolution of 1/10 resulting in a concentration of 2×10-4M benzydamine at the oral mucosal side. It remains to be shown-calculated/estimated that at the smooth muscles a concentration of 10-5M can be reached. Therefore, commercial benzydamine oral spray could decrease the contraction of tracheal smooth muscle during an asthmatic attack. The actual concentration of benzydamine in tracheal smooth muscle when used in spray requires further investigation. The mechanism by which this benzydamine affected the trachea smooth muscle is unknown and further studies are needed to elucidate the answer.
EFS is a common experimental tool; it activates the nerve terminals within the tissue to be tested and induces the release of endogenous neurotransmitters thereby triggering smooth muscle contraction. EFS-induced spike contraction of canine nasal mucosa, which is believed to result from the contraction of vascular smooth muscles, disappeared after ipsilateral cervical sympathetic ganglionectomy [
11]. Thus, EFS-induced spike contraction of isolated canine nasal mucosa has been proved to be mediated by sympathetic innervation [
11]. In this study, EFS-induced spike contraction of the tracheal smooth muscle was believed to be due to stimulation of parasympathetic innervation. Therefore, EFS-induced contraction of the trachea was decreased as the benzydamine concentration was increased. These findings suggested that benzydamine could antagonize the parasympathetic innervation responsible for trachea smooth muscle contraction. In addition, basal tension elicited a minimal effect at various concentrations of benzydamine. Oxymetazoline, a nasal spray used as a nasal decongestant, could reduce methacholine-induced contraction as well, but it also had minimal effect on basal tension too. It is known as a direct-acting α-adrenergic agonist [
12]. Clearly, what was observed in this study is very interesting, but further study is needed to clarify these phenomena.
The results of this study showed that high concentrations of benzydamine might actually inhibit parasympathetic function of the trachea. It could reduce methacholine-induced contraction as well. In addition to oral mucosal symptoms, benzydamine treats effectively an asthmatic attack. In the in vivo situation, the response might be much more complicated than that in the in vitro situation. Clinically, there were many oral mucositis patients who were suffering from radiation effects and had an asthma history. It is safe for them to use benzydamine oral spray.
In conclusion, this study indicated that high concentrations of benzydamine might actually inhibit parasympathetic function of the trachea. Benzydamine might reduce asthmatic attacks when administered to pharyngitis or oral mucositis patient because it could inhibit parasympathetic function and reduce methacholine-induced contraction of tracheal smooth muscle.
Go to :

ACKNOWLEDGMENTS
This work was supported in part by Taipei Medical University, Shuang-Ho Hospital (100MTU-SHH-05).
Go to :

Notes
Go to :

References
1. Turnbull RS. Benzydamine Hydrochloride (Tantum) in the management of oral inflammatory conditions. J Can Dent Assoc. 1995; 2. 61(2):127–134. PMID:
7600413.
2. Fanaki NH, el-Nakeeb MA. Antimicrobial activity of benzydamine, a non-steroid anti-inflammatory agent. J Chemother. 1992; 12. 4(6):347–352. PMID:
1287137.

3. Alterio D, Jereczek-Fossa BA, Fiore MR, Piperno G, Ansarin M, Orecchia R. Cancer treatment-induced oral mucositis. Anticancer Res. 2007; Mar-Apr. 27(2):1105–1125. PMID:
17465250.
4. Karavana SY, Guneri P, Ertan G. Benzydamine hydrochloride buccal bioadhesive gels designed for oral ulcers: preparation, rheological, textural, mucoadhesive and release properties. Pharm Dev Technol. 2009; 14(6):623–631. PMID:
19883251.
5. Kazemian A, Kamian S, Aghili M, Hashemi FA, Haddad P. Benzydamine for prophylaxis of radiation-induced oral mucositis in head and neck cancers: a double-blind placebo-controlled randomized clinical trial. Eur J Cancer Care (Engl). 2009; 3. 18(2):174–178. PMID:
19267733.

6. Wang HW, Wang YT, Wu CC. A modified in vitro method for studyingtracheal smooth muscle response to drugs. J Med Sci. 2007; 10. 27(5):203–206.
7. Kao CH, Chu YH, Wang HW. Effects of lidocaine on rat's isolated tracheal smooth muscle. Eur Arch Otorhinolaryngol. 2010; 5. 267(5):817–820. PMID:
19714348.

8. Bratton DL, Tanaka DT, Grunstein MM. Effects of temperature on cholinergic contractility of rabbit airway muscle. J Appl Physiol (1985). 1987; 11. 63(5):1933–1941. PMID:
3320012.

9. González O, Santacana GE. Effect of low temperature on tracheal smooth muscle contractile and relaxing responses evoked by electrical field stimulation. P R Health Sci J. 2001; 9. 20(3):237–244. PMID:
11776725.
10. Yau KI, Hwang TL. The nonadrenergic noncholinergic system can modulate the effect of prokinetic agents on contractile response of isolated guinea-pig trachea segments to electrical field stimulation. J Formos Med Assoc. 2002; 10. 101(10):695–699. PMID:
12517043.
11. Wang HW, Jackson RT. Do cholinergic neurons directly innervate nasal blood vessels? Rhinology. 1988; 6. 26(2):139–146. PMID:
3175457.
12. Wang HW, Wu CC. Effects of oxymetazoline on isolated rat's tracheal smooth muscle. Eur Arch Otorhinolaryngol. 2008; 6. 265(6):695–698. PMID:
17978828.

Go to :






 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download