Abstract
Objectives
Draf IIb approach provides wide, unilateral access to the frontal sinus. This approach can be extended without destruction of the contralateral frontal sinus drainage pathway, performed during Draf III (modified Lothrop) procedure. There is limited data in the literature regarding the use of modified Draf IIb procedures.
Methods
Patients treated with extended Draf IIb procedures in a single center were retrospectively assessed.
Results
Ten patients were identified, including 2 cases of osteoma, 1 inverted papilloma, 1 carcinoma, 5 mucoceles, and 1 chronic rhinosinusitis patient. Six patients had undergone prior surgery, including external procedures in 3 cases. Modifications of Draf IIb were classified as the following: removal of the anterosuperior nasal septum adjacent to the nasal beak, removal of the intersinus septum, and a combination of the above-mentioned methods (upper nasal septum and intersinus septum removal). There were 3 patients operated on with type 1 modification, one patient with type 2 modification, and 6 patients with type 3 modification. There were no perioperative complications.
Draf III procedure, also known as the modified endoscopic Lothrop procedure or median drainage, provides a wide transnasal approach to both frontal sinuses [1,2]. In the case of confined, predominantly unilateral lesions, distorted anatomy from previous procedures or trauma, less destructive, limited approaches, defined as modified or extended Draf IIb, can be applied. In these techniques, Draf IIb approach is extended without destruction of the contralateral frontal sinus drainage pathway. There is limited information on the use of modified Draf IIb procedures and their classification in literature.
Draf IIb can be extended by creating septectomy window to gain access to the laterally located supraorbital cell [3,4,5], or by removal of the anterosuperior nasal septum adjacent the frontal beak to gain better access to the anterior table. The advantage of septal perforation is possibility of bimanual dissection. Another modification of Draf IIb procedure, referred to as mini-Lothrop procedure is performed by removal of the intersinus septum [6,7]. The third possibility is a combination of both of the above-mentioned procedures: removal of the upper nasal septum and the intersinus septum. This modification provides the widest access to both frontal sinuses without destruction of the natural drainage pathway of the contralateral sinus. We present a series of 10 patients treated with these methods.
A retrospective analysis was done of extended Draf IIb procedures performed in a single center by the first author (TG) between 2010 and 2012. Data were collected on type of pathology, operative technique and postoperative course. The University Ethics Committee approved the study (approval number AKBE/15/13).
The procedures were performed under general anesthesia. If not performed during the previous procedures, the frontal recess was widened and the anterior-upper part of the middle turbinate was trimmed using standard functional endoscopic sinus surgery instruments and a 30° rigid scope. Draf IIb procedure was then performed with an irrigated curved burr (5.0 mm 15° burr, or 3.6 mm 70°, Unidrive motor system, Drill-Cut X handpiece, Karl Storz, Tuttlingen, Germany) and Kerrison punches. Further extension of the procedure depended on specific pathology and individual anatomic variations. The posterior wall of the frontal sinus was traced to avoid anterior cranial fossa penetration. Care was taken not to create excessive damage to the mucosa to prevent scarring of the ostium created.
Patients used saline nasal douches for 3 weeks postoperation, starting the day after surgery, and intranasal steroids starting 3 weeks after surgery. Follow-up was performed by nasal endoscopy.
Ten patients treated with extended Draf IIb procedures were identified (6 females and 4 males). Mucocele was the most common indication for surgery (5 cases) followed by osteoma (2 cases), inverted papilloma (1), carcinoma (1), and chronic rhinosinusitis (CRS) without polyps (1). One of the patients with frontal sinus osteoma had concurrent CRS with polyps. Three patients had undergone prior endoscopic surgery, and another 3 had undergone external approach procedures (all of them presented presented with mucocele or CRS).
The performed modifications of Draf IIb procedure were classified as Fig. 1: (1) Extended Draf IIb.1=Draf IIb+removal of the anterosuperior nasal septum adjacent to the frontal beak (Fig. 1B); (2) Extended Draf IIb.2, or mini-Lothrop=Draf IIb+removal of the lower intersinus septum (Fig. 1C); and (3) Extended Draf IIb.3=Draf IIb+removal of the upper nasal septum and the lower intersinus septum (Fig. 1D).
There were 3 patients operated on with type 1 modification, 1 patient with type 2 modification, and 6 patients with type 3 modification. There were no early complications, with the exception of eye-lid ecchymosis. The mean observation time was 14.7 months (range, 6 to 29 months). The ostium created was occluded in 2 patients operated on with extended Draf IIb.3. In the patient operated on due to type II osteoma (Chiu classification) and CRS with polyps, the ostium was completely occluded with the formation of a mucocele. The second patient had undergone 3 previous osteoplastic flap (OPF) procedures. After each of them, the frontal ostium became occluded. Both of these patients were reoperated on endoscopically and remain under close follow-up.
Advantages of extended Draf IIb.1 include the possibility of performing bimanual surgery and allowance of decent access to the anterior and lateral aspect of the frontal sinus due to removal of the anterosuperior part of the septum adjacent to the nasal beak. This approach in our study group was chosen for the patient with cancer due to the need for an appropriate margin of resection (Fig. 2), the patient with osteoma due to the possibility of bimanual dissection (Fig. 3A), and for the patient with a mucocele due to the need for maximum widening of the ostium. Indications for this approach did not include a lateral lesion location or supraorbital frontal cell. This approach should be distinguished from Hemi-Lothrop procedure described by Eloy et al. [3,4,5], in which nasal septectomy is created more inferiorly and posteriorly to gain access to laterally located supraorbital frontal cell from the contralateral nasal cavity.
In unilateral frontal sinus disease with intersinus septum deviation towards the lesion, ipsilateral extended Draf IIb procedure with removal of the intersinus septum (extended Draf IIb.2 or mini-Lothrop procedure [3,7]) can be a suitable treatment option, especially in cases with the presence of a mucocele (Fig. 3B). Similar procedure was described by Cho et al. [8], who used 'above and below' approach.
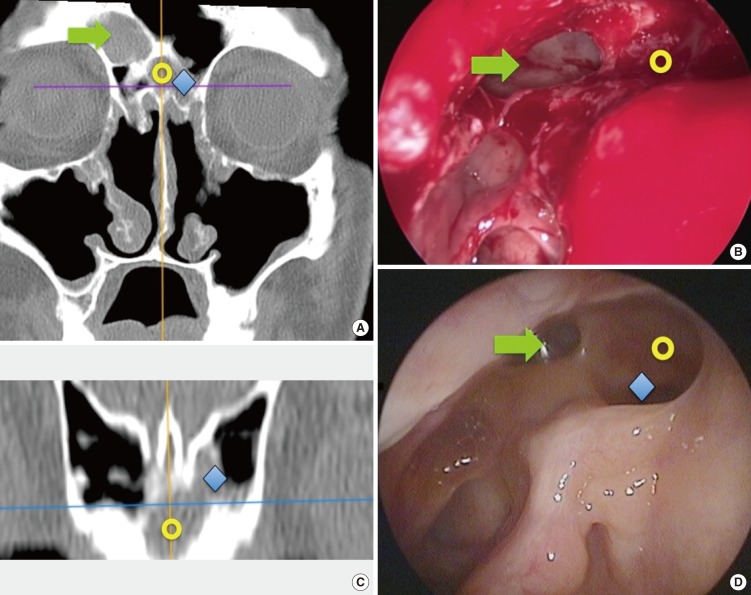
The extended Draf IIb.3, similar to extended Draf IIb.1, gives the possibility of bimanual dissection and enables appropriate visualization into the lateral aspect of the sinus. The ostium created is wider when compared to extended Draf IIb.1, and allows for inspection of major parts of the contralateral sinus and better maneuverability with surgical tools. There is potential for this procedure to be useful in the treatment of tumors of the frontal sinus. We used it for removal of inverted papilloma (Fig. 4), originating from the posterior table of the frontal sinus and crossing the midline (there was no sign of recurrence in 1 year of observation).
Removal of the intersinus septum, in our opinion, should not be treated as an unintended, harmful effect of surgery. There are reports on intersinus septectomy as a method of treatment of unilateral frontal sinus disease [8,9,10]. Intersinus septectomy is often performed during transseptal frontal sinusotomy [11], as an adjunct procedure during the Lynch procedure [12]. We tried to remove the lower intersinus septum from the anterior to the posterior table during the extended Draf IIb.2 and 3 procedures, however, in some cases, it was not possible due to distorted anatomy from previous procedures (Fig. 3A) or an irregular course of the septum. Assuming that intersinus septectomy does not disrupt mucociliary transport, it should have a beneficial effect in CRS patients by increasing aeration of the sinus, functioning in a similar fashion to a tympanostomy tube. There have been no symptoms related to mucus recirculation in patients from our group, and we did not observe it during endoscopic examination. However, data from a larger group of patients is needed to exclude such a possibility.
Removal of the intersinus septum during extended Draf IIb.2 and 3 procedures can be more complicated in the presence of a large frontal intersinus septal cell.
In radiological studies, a frontal intersinus septal cell, also known as a frontal wishbone, was found in 30% to 70% of patients [13,14,15]. Its anteroposterior dimensions were found to be larger in CRS patients with involvement of the frontal sinus [15]. This cell drains into one frontal sinus and, very rarely, to both of them. Among our patients that underwent extended Draf IIb.2 or 3 procedures, a frontal intersinus septal cell was found in 5 out of 7 patients. A large frontal intersinus septal cell restricting the drainage of the adjacent frontal sinus was present in 2 of them. In one of these patients with right-sided pathology, the intersinus cell had broad communication with the left frontal sinus. After right-sided extended Draf IIb.1, the wall of the intersinus cell was opened and the left frontal sinus was visualized through the intersinus cell. In the second patient, the anatomical situation was very similar, but the communication of the intersinus cell with the left frontal sinus was narrower (Fig. 5).
Both procedures were classified as extended Draf IIb.3, as the end result was the creation of communication between both frontal sinuses and perforation of upper nasal septum.
One of the patients from our group with ostium occlusion suffered from CRS with polyps and osteoma. Results of other studies seem to prove that the best surgical option for diffused polyposis is total sphenoethmoidectomy with wide medial antrostomy and median drainage (Draf III) [16]. Thus, in cases of recalcitrant CRS with polyps, we would advocate to perform nasalization and Draf III, rather than Draf IIb or extended Draf IIb procedure.
In conclusion, selected cases of isolated frontal sinus disease can be safely and effectively managed using tailored modifications of Draf IIb procedure. The decision of the type of extension of Draf IIb procedure to use depends on the anatomical variation of the frontal sinuses, especially the intersinus septum, previous procedures, and type of disease.
References
1. Draf W. Endonasal micro-endoscopic frontal sinus surgery: the Fulda concept. Oper Tech Otolaryngol Head Neck Surg. 1991; 12. 2(4):234–240.

2. Draf W, Minovi A. The frontal "T" in refinement of endonasal frontal sinus type III drainage. Oper Tech Otolaryngol Head Neck Surg. 2006; 6. 17(2):121–125.
3. Friedel ME, Li S, Langer PD, Liu JK, Eloy JA. Modified hemi-Lothrop procedure for supraorbital ethmoid lesion access. Laryngoscope. 2012; 2. 122(2):442–444. PMID: 22252573.

4. Eloy JA, Kuperan AB, Friedel ME, Choudhry OJ, Liu JK. Modified hemi-Lothrop procedure for supraorbital frontal sinus access: a case series. Otolaryngol Head Neck Surg. 2012; 7. 147(1):167–169. PMID: 22371340.
5. Eloy JA, Friedel ME, Murray KP, Liu JK. Modified hemi-Lothrop procedure for supraorbital frontal sinus access: a cadaveric feasibility study. Otolaryngol Head Neck Surg. 2011; 9. 145(3):489–493. PMID: 21515802.
6. Eloy JA, Friedel ME, Kuperan AB, Govindaraj S, Folbe AJ, Liu JK. Modified mini-Lothrop/extended Draf IIB procedure for contralateral frontal sinus disease: a case series. Int Forum Allergy Rhinol. 2012; Jul-Aug. 2(4):321–324. PMID: 22473904.

7. Friedel ME, Kuperan AB, Liu JK, Eloy JA. Modified Draf IIb with frontal intersinus septectomy for frontal sinus disease: a cadaveric study. Laryngoscope. 2011; 1. 121(Suppl 4):229.
8. Cho SH, Lee YS, Jeong JH, Kim KR. Endoscopic above and below approach with frontal septotomy in a patient with frontal mucocele: a contralateral bypass drainage procedure through the frontal septum. Am J Otolaryngol. 2010; Mar-Apr. 31(2):141–143. PMID: 20015729.

9. Reh DD, Melvin TA, Bolger WE, Lane AP. The frontal intersinus septum takedown procedure: revisiting a technique for surgically refractory unilateral frontal sinus disease. Laryngoscope. 2011; 8. 121(8):1805–1809. PMID: 21792973.
10. Goode RL, Strelzow V, Fee WE Jr. Frontal sinus septectomy for chronic unilateral sinusitis. Otolaryngol Head Neck Surg (1979). 1980; Jan-Feb. 88(1):18–21. PMID: 7393597.

11. Lanza DC, McLaughlin RB Jr, Hwang PH. The five year experience with endoscopic trans-septal frontal sinusotomy. Otolaryngol Clin North Am. 2001; 2. 34(1):139–152. PMID: 11344069.

12. Weissler MC. Open approaches. In : Kountakis S, Senior BA, Draf W, editors. The frontal sinus. Berlin: Springer-Verlag;2005. p. 275–280.
13. Merrit RM, Bent JP, Kuhn FA. The intersinus septal cell: anatomic, radiologic, and clinical correlation. Am J Rhinol. 1996; Sep-Oct. 10(5):299–302.
14. Som PM, Lawson W. The frontal intersinus septal air cell: a new hypothesis of its origin. AJNR Am J Neuroradiol. 2008; 6. 29(6):1215–1217. PMID: 18388213.

15. Goldsztein H, Pletcher SD, Reh DD, Metson R. The frontal wishbone: anatomic and clinical implications. Am J Rhinol. 2007; Nov-Dec. 21(6):725–728. PMID: 18201455.

16. Bassiouni A, Wormald PJ. Role of frontal sinus surgery in nasal polyp recurrence. Laryngoscope. 2013; 1. 123(1):36–41. PMID: 23070897.

Fig. 1
Schematic drawing of the resection area in the coronal plane. (A) Draf IIb, (B) extended Draf IIb.1, (C) extended Draf IIb.2 (mini-Lothrop), and (D) extended Draf IIb.3.
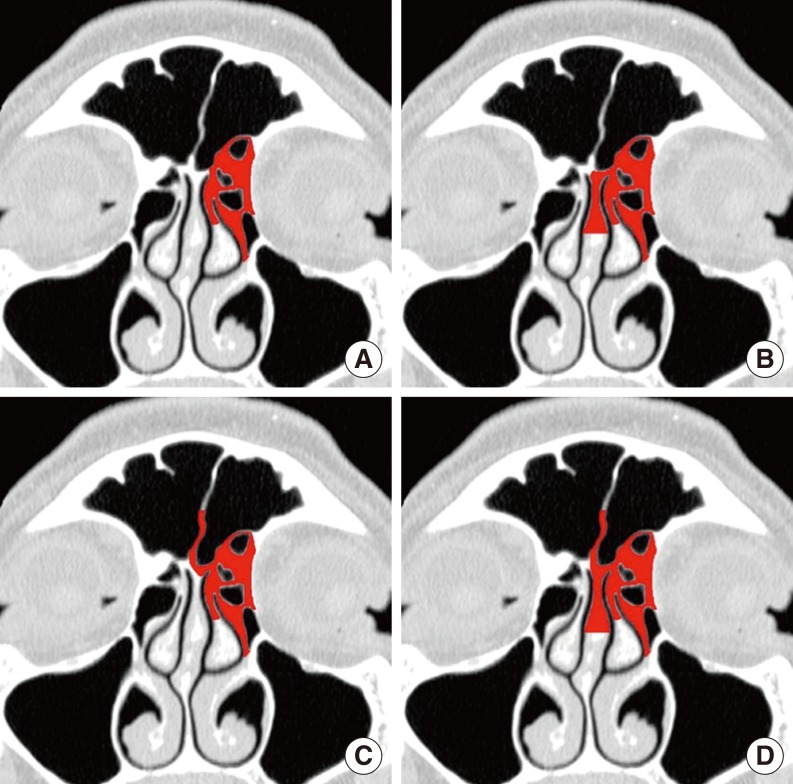
Fig. 2
Preoperative computed tomography (A) and magnetic resonance imaging (B) of the patient with sinonasal carcinoma treated with the extended Draf IIb.1.
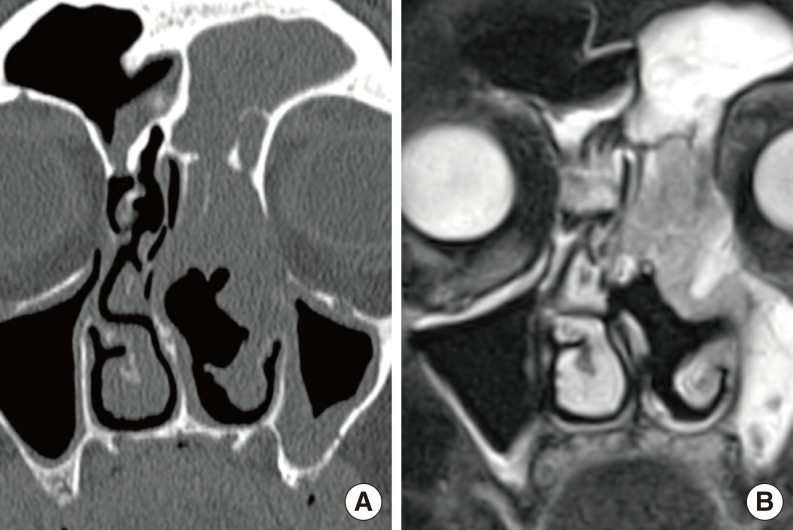
Fig. 3
Computed tomography before (A, C) and after the surgery (B, D). (A, B) Patient with osteoma treated with the extended Draf IIb.1. (C, D) Patient with mucocele as a consequence of osteoplastic flap procedure, treated with the extended Draf IIb.2 (mini-Lothrop) procedure.
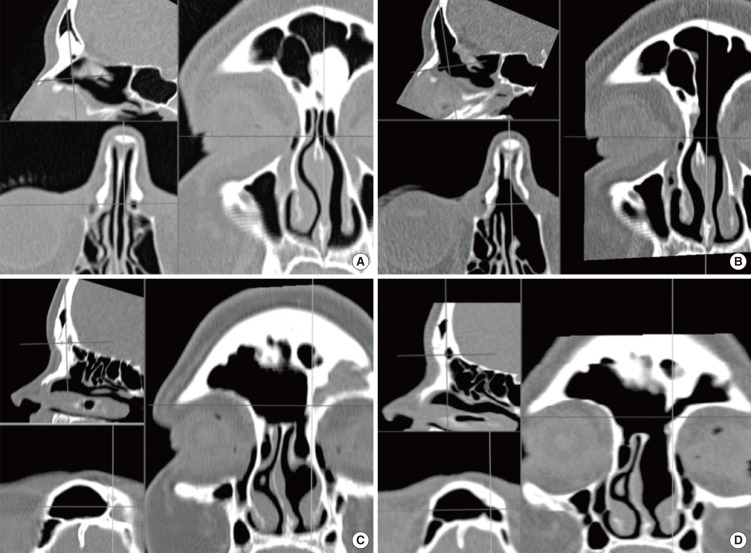
Fig. 4
Preoperative computed tomography (A) and magnetic resonance imaging (B) of the patient with inverted papilloma of the frontal sinus treated with the extended Draf IIb.3. Attachment of the tumor was found on the posterior table of the left frontal sinus. Small part of the tumor, which crossed the midline, was overhanging with no attachment on the right side.

Fig. 5
Patient with right-sided frontal sinus mucocele treated with the extended Draf IIb.3. Computed tomography before the procedure (A, C); endoscopic view through the right nasal passage after the Draf IIb.3 procedure (B, D), intraoperative view (B) and postoperative view (D). Arrows indicate the site of the mucocele; circles indicate the frontal intersinus septal cell; diamonds represent site of communication between frontal intersinus septal cell and left frontal sinus.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download