CASE REPORT
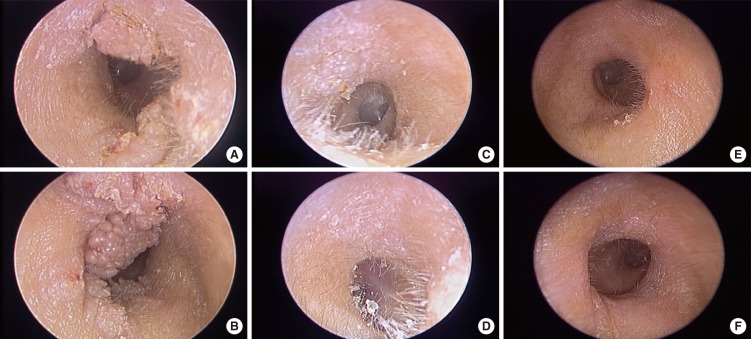
A 32-year-old male patient presented with ear fullness and palpable lumps in both EACs. The lumps were identified 18 months prior to the examination and the patient indicated that the lumps appeared to be getting larger. The patient had not undergone any specific treatment. Otoscopic examination revealed multiple pinkish, papillomatous masses that filled both of his EACs (
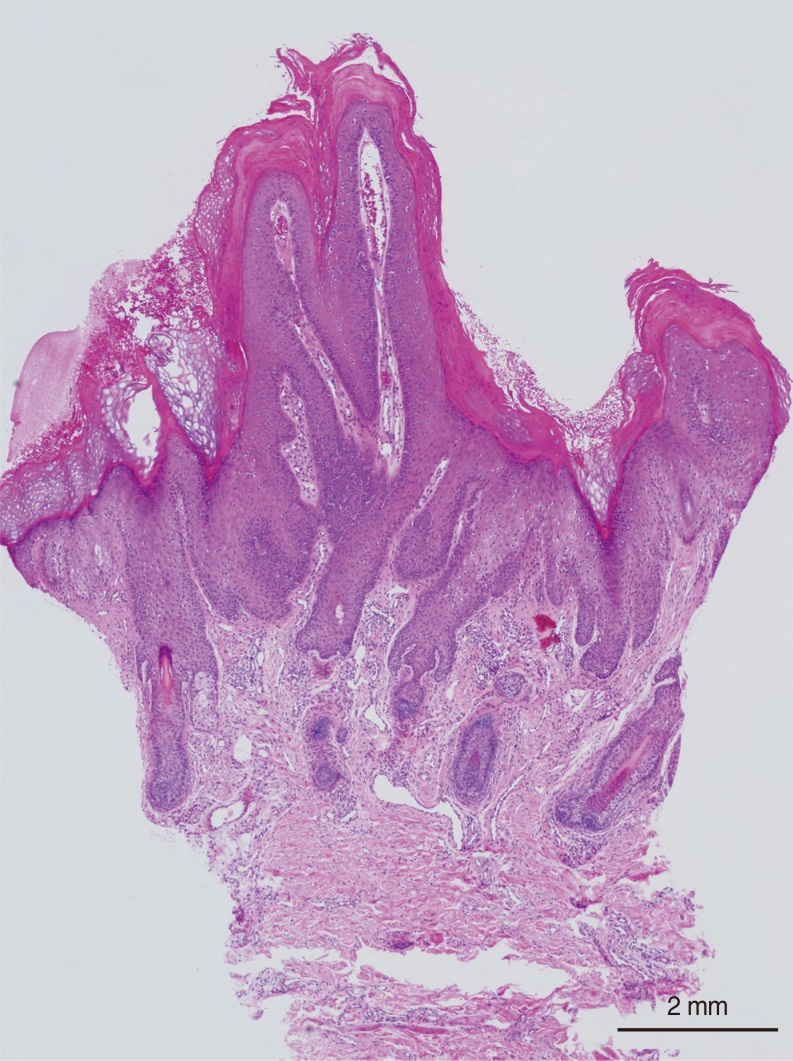
Fig. 1A, B). The tympanic membrane and the surrounding tissue were intact. Verruca was confirmed by punch biopsy (
Fig. 2). An otolaryngologist referred this patient and recommended surgical excision and skin grafting. However, we performed intralesional bleomycin injection, which is a simple and effective method for treatment of verruca vulgaris on the hands, feet or face.
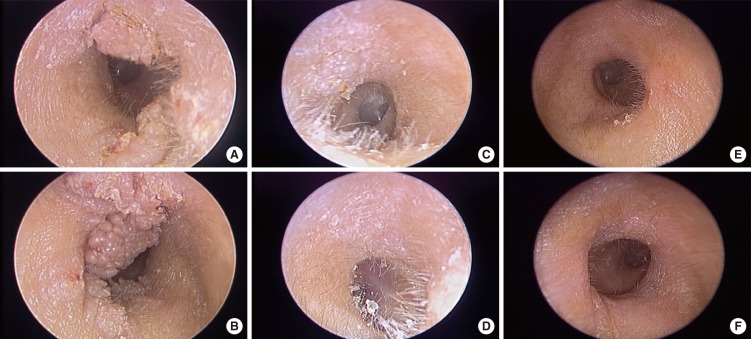 | Fig. 1Verruca vulgaris of both external auditory canals. (A, B) Multiple pinkish, papillomatous masses filled both external auditory canals. (C, D) One month after the first intralesional bleomycin injection. (E, F) Two months after the second intralesional bleomycin injection, all verrucae were completely disappeared without complication.
|
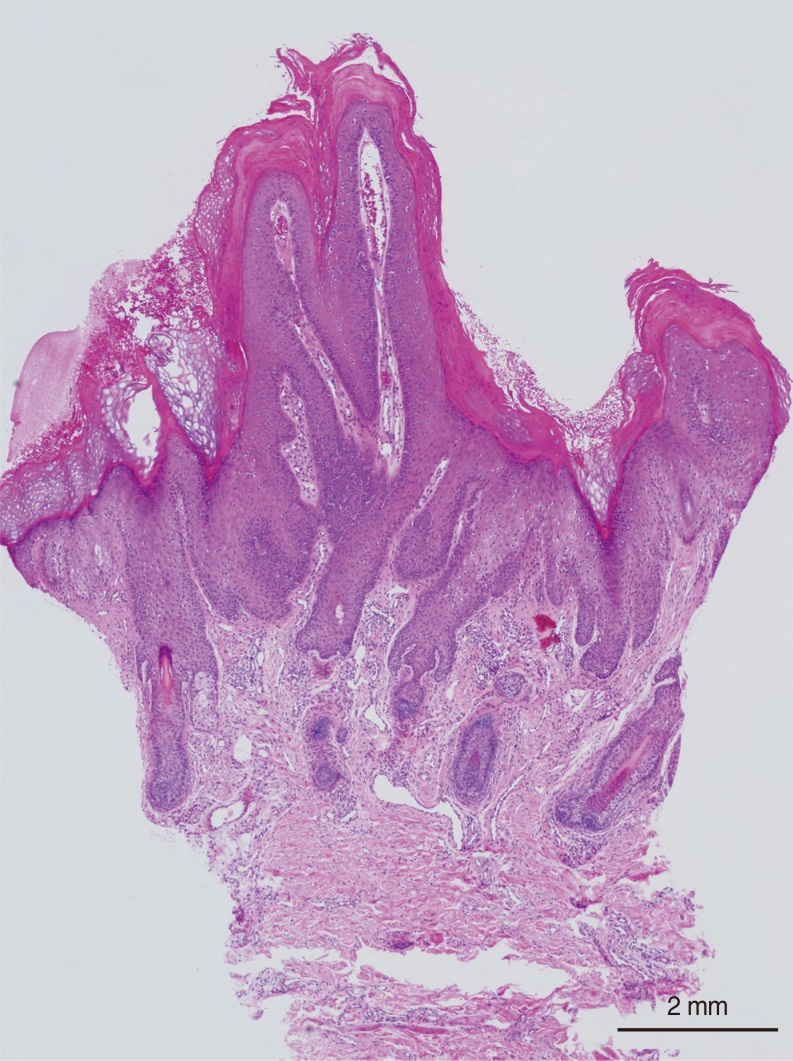 | Fig. 2Histopathological section of verruca in the external auditory canals. It indicates verruca vulgaris with a central fibrovascular core covered by keratinizing squamous epithelium (H&E, ×12.5).
|
Bleomycin was diluted with 1% lidocaine to make a 1-U/mL bleomycin solution. A 1-mL syringe with a 30-gauge needle was used to directly inject the bleomycin solution until the verruca was completely blanched. The bleomycin solution was injected twice; 0.5 mL at the first injection and 0.2 mL at the second injection one month later.
One month after first injection, the verruca decreased to approximately one-third of the initial size (
Fig. 1C, D). Two months after the second injections, the verruca was not observed and there was no scarring or necrosis (
Fig. 1E, F). Eight months after the second injection, the patient confirmed that there was no recurrence.
Go to :

DISCUSSION
Verruca vulgaris is caused by an HPV infection, and there are over 100 human papilloma DNA viruses that belong to the DNA papovaviridae family [
12345]. The most common sites of infection are the hands, feet and face [
1]. Histopathological examination is used for a definitive diagnosis, and revealed characteristic features of hyperkeratosis, papillomatosis, parakeratosis, acanthosis, and koilocytosis [
345].
Verruca in the EAC has rarely been reported. It is associated with low-risk HPV infections (types 6 and 11) that often result in a benign clinical course with no recurrence or malignant transformation [
345]. The mode of HPV transmission to EAC is currently not known. EAC infections are thought to be associated with a history of repeated manipulation using the finger tips or ear picking tools. In addition, it has been suggested that the hair follicles may serve as possible reservoirs [
2345]. EAC verruca causes mechanical obstruction which can lead to pressure necrosis of the adjacent bone or conductive hearing impairments, although tympanic membrane involvement is seldom reported [
24].
There are currently several methods to treat verruca, which include topical treatments, cryotherapy, immunotherapy, photodynamic therapy, laser therapy, curettage and cautery, radiation therapy, surgical excision and intralesional bleomycin injections [
12346]. A case report introduced surgical excision of verruca in the EAC as the preferred treatment because of difficulty to apply nonsurgical treatment such cryotherapy, photodynamic therapy or laser therapy [
2]. However, the most common complication associated with surgical excision is the possibility of scarring and subsequent EAC stenosis [
4].
Intralesional bleomycin injections have been used to treat verruca on the hands, forearm, feet and face [
1678910]. Bleomycin was originally isolated from the fungus,
Streptomyces verticillus, and is frequently used as an antitumor agent. Bleomycin blocks the cell cycle at G2, cleaves single-stranded and double-stranded DNA and degrades cellular RNAs; it also forms a complex with metal ions, which reduce oxygen to free radicals [
78]. These free radicals cause DNA breaks that ultimately lead to cell death. Other possible underlying mechanisms are endothelial damage, which induce tumor necrosis factor, hemorrhage of subepidermis and intraepidermis, and the appearance of apoptotic cells [
781011]. Bleomycin is hydrophilic and does not easily cross cell membranes [
7]. The cytotoxic effect and uptake of bleomycin is increased by mixing drug with local anesthetics because local anesthetics disrupt the cell membrane structure [
12].
After bleomycin intralesional injection, verruca on the hands and feet has exhibited hemorrhagic black eschars which suggest adequate bleomycin infiltration. Eschar formation is thought to be caused by absolutely decreased blood flow, necrosis, and subsequent detachment of the lesion [
7]. Eschar on the hands and feet typically separate after 2 to 3 weeks [
8].
However, verruca on the face indicated that the verruca gradually shrank after injection, and disappeared without eschar formation [
9]. We thought that the blood supply is decreased after injection but not completely interrupted because of rich and large dermal capillaries of the face. Incomplete blockage of blood flow may not cause hemorrhagic necrosis, eschar formation and consequential verruca detachment. Induction of endothelial and keratinocyte apoptosis by direct or indirect damage may be result in verruca shrinkage without necrosis or eschar. Verruca in the EAC disappeared without eschars after injections. Its clinical course was similar to one of verruca on the face.
In conclusion, we present a case of large and multiple verruca in both EACs that was successfully treated with twice intralesional bleomycin injections at one-month interval. There was no complication, such as ulceration, scar formation or recurrence. An intralesional bleomycin injection is simple, easy to apply without any difficulty and limitation, and had a high degree of patient satisfaction for treatment of verruca in the EAC. We propose that it may be an effective, first-line treatment of verruca in the EAC.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download