INTRODUCTION
A foreign body in the upper gastrointestinal tract occurs sporadically as food is ingested, and in many cases, it can cause irritation and pain. Most visits to medical institutions because of this problem are urgent; thus, it is very important to understand how to appropriately evaluate foreign bodies and provide treatment in an emergency medical situation [
1].
A foreign body in the upper gastrointestinal tract is an emergency that can occur frequently at any age. In 80%-90% of cases, the foreign body passes through the intestinal canal naturally, but in 10%-20% of cases, a noninvasive intervention is necessary; surgery is required in approximately 1% or less [
1234]. In some cases, various complications can occur, such as shutdown of the digestive tract, perforation, bleeding, ulcer, and peritonitis, and it can even lead to death [
5]. Approximately 1,500 people in the United States die annually due to foreign body ingestion [
6]. The most commonly ingested foreign body is a fish bone, and when it is in the oral cavity and laryngopharynx, it can easily be discovered. However, when it is in the esophagus, discovery and treatment are not easy and occasionally the foreign body is not found. Previous studies examined the usefulness of computed tomography (CT) in detecting esophageal foreign bodies and concluded that CT is the examination of choice for radiographic diagnosis and also for identifying soft tissue injury and inflammation [
78]. In addition, there have been recent reports of transnasal flexible esophagoscopy (TNE) being used to remove esophageal foreign bodies [
9].
Fish bone impaction in the upper gastrointestinal tract is a common reason for patients to seek emergent care, but the diagnosis and treatment of esophageal fish bone impaction was not yet fully proven. To address these problems, the current research aimed to find a clinical characteristics of patients with fish bone impaction in the upper gastrointestinal tract.
Go to :

MATERIALS AND METHODS
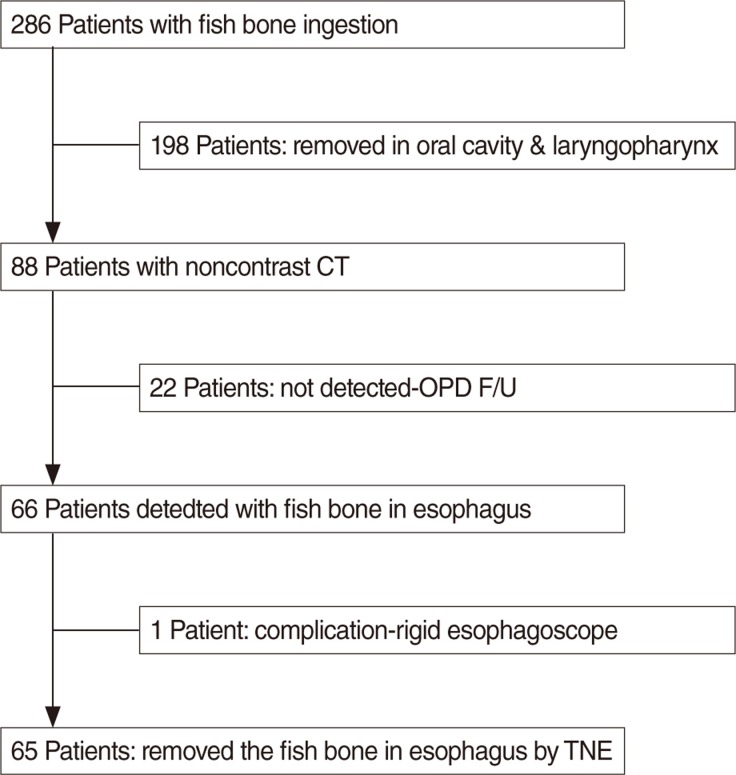
The study was conducted on fish bone ingestion patients who visited Gyeongsang National University Hospital complaining of dysphagia and irritation after eating fish from December 2010 to August 2012. The study selected 286 patients for whom fish bone foreign bodies in the upper gastrointestinal tract, including the oral cavity and laryngopharynx were suspected (
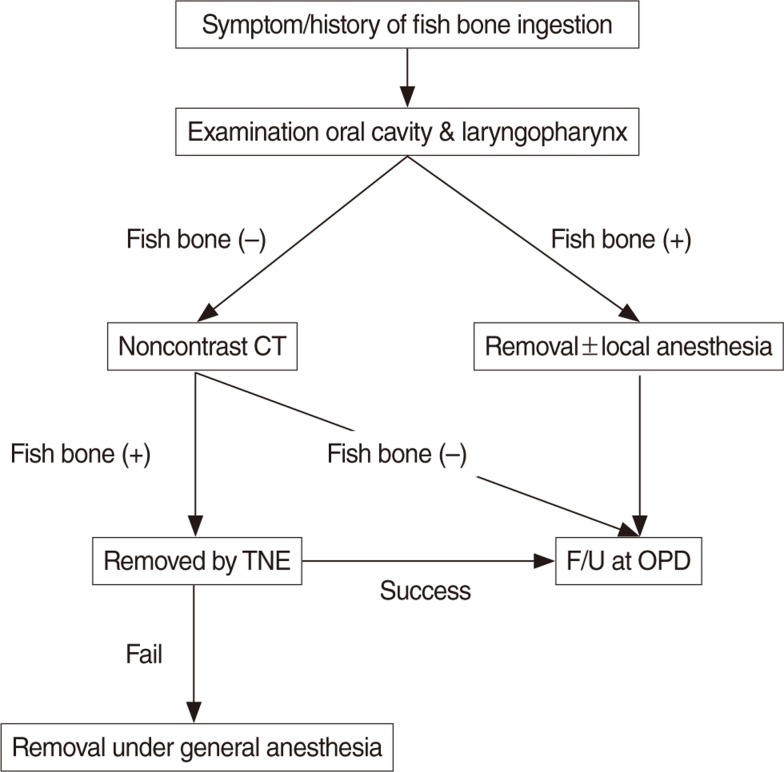
Fig. 1). Examination and treatment were performed according to the foreign body removal protocol (
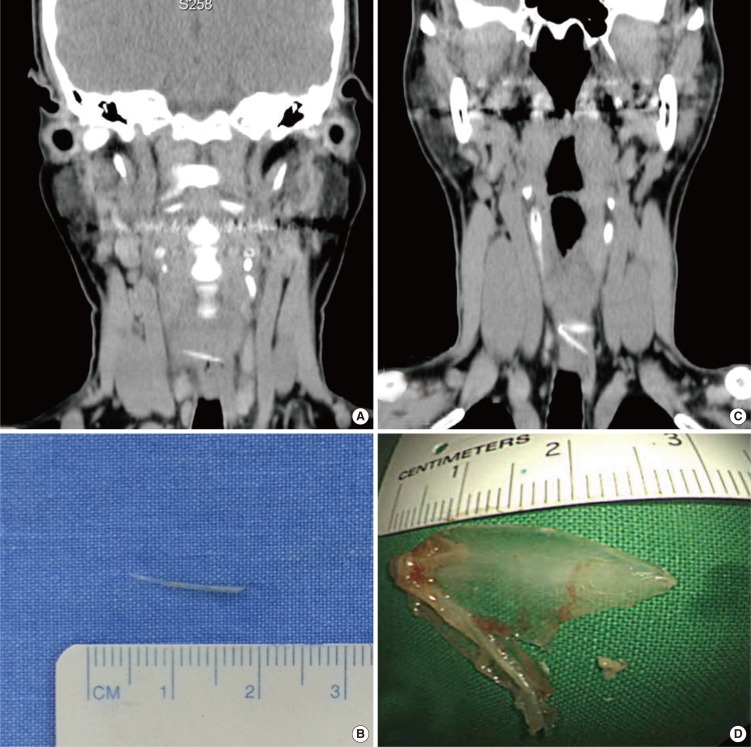
Fig. 2) developed by the hospital. After receiving the patient's consent, we investigated to analyze sex, age distribution, location and type of the fish bone foreign body, endoscopy observations, removal method of the foreign body, and complications after removal. When a fish bone was identified in the oral cavity or laryngopharynx, it was removed using forceps. However a foreign body was suspected in the esophagus, we used noncontrast CT. A radiologic evaluation including the following was performed: Helical CT scan, 3/3 mm slice thickness with images reconstructed at intervals of 1.5 mm, pitch 1.5, without oral or intravenous contrast material. Examination was limited to the upper gastrointestinal area (from the nasopharynx to the diaphragm limits). The CT studies were performed with a CT HiSpeed (GE Medical Systems, Milwaukee, WI, USA).The studies were interpreted as being pathological if a hyperdense body was detected in the esophageal lumen or within/next to the cervical esophageal walls. All these studies were performed and interpreted by a staff radiologist. If the fish bone was visible in noncontrast CT, it was removed using TNE. The EPM-3500 from PENTAX (Tokyo, Japan) was used as the TNE for endoscopic foreign body removal.
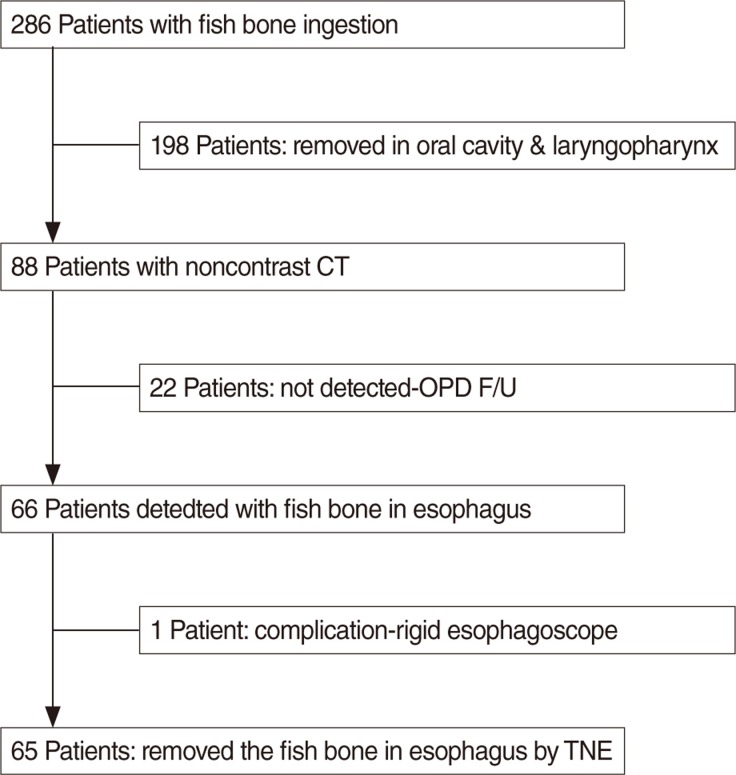 | Fig. 1The enrollment of patients. CT, computed tomography; OPD, out patient department; F/U, follow-up; TNE, transnasal esophagoscopy.
|
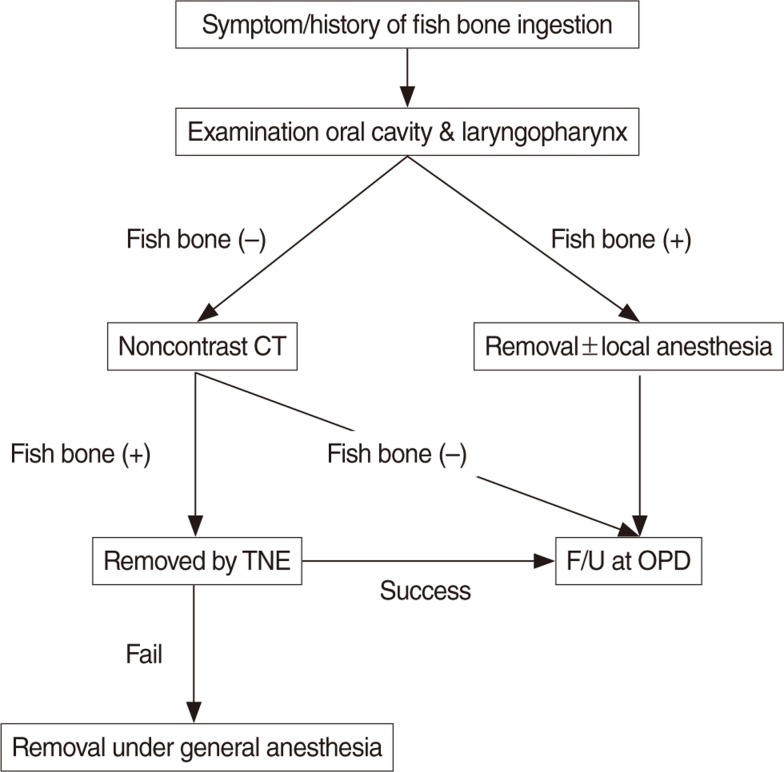 | Fig. 2The protocol of fish bone removal. CT, computed tomography; TNE, transnasal esophagoscopy; F/U, follow-up; OPD, out patient department.
|
Ethics
This study was performed after obtaining the approval from the Institutional Review Board at Gyeongsang National University Hospital (GNUH-2010-09-013-001) and registered at the Clinical Research Information Service (CRIS, KCT0000661).
Statistical analysis
We used the Mann-Whitney U-test for comparison of the age difference between two foreign body location groups, and we used Fisher exact test to compare types of food proportions between males and females. All statistical analysis was done using IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA), and the statistical significance threshold was set at <0.05 (2-sided test).
Go to :

DISCUSSION
In adults, a foreign body in the upper digestive tract usually occurs during daily meals. Especially in a region or country where people consume a large amount of fish, fish bone is a frequently discovered foreign body in the upper digestive tract [
8]. The locations for fish bones discovered in the upper digestive tract are known to occur mainly in the palatine tonsils, base of the tongue, valleculae, and the pyriform sinus [
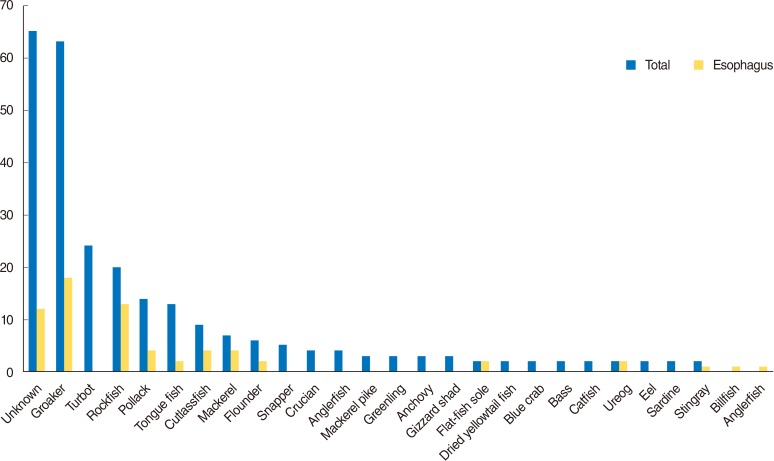
1011]. In this study, 198 cases out of 286 (69.23%) were discovered in the oral cavity and laryngopharynx. Thus, the results are in good agreement with existing results. In the esophagus, fish bone is most frequently discovered mainly in first narrow area among 3 narrow areas. Similar to existing reports, 65 cases of fish bones (98%) were discovered in the upper esophagus in this study. Also, we have analyzed about the type of fish and fish recipes. The type of fish that caused foreign body in the upper digestive tract was varied and there were no significant findings. However, a fish recipes (especially fish stew) was significant finding in esophageal foreign body impaction (
P<0.006).
Fish bones discovered in the oral cavity and laryngopharynx had a wide distribution for various age groups. However, fish bone impaction in the esophagus appeared to be more common in older patient in this study. According to Sheth and Diner [
10], dysphagia can occur as swallowing movement deteriorates with increasing age. In this respect, the reason for the rapid increase in fish bones in the esophagus in people older than their 40s is thought to be related to the physiological characteristics of the esophagus and the deterioration in swallowing movement that occurs with increasing age.
In diagnosis of patients with esophageal foreign bodies, the symptoms of the patient and the observations of the practitioner may not agree. Cervical plain film used to be included in the traditional management of impacted foreign body in esophagus. However, several studies [
7111213] have demonstrated poor sensitivity when the foreign body is fish, because they are rarely visible on radiographs. Otherwise, the CT was very high sensitivity and specificity. In a clinical study published in the digestive literature [
121415], the authors found noncontrast CT to be very effective in detecting esophageal bone impaction. In a unique clinical prospective study published in the otorhinolaryngology literature [
14], the authors found conventional CT to be very effective in detecting esophageal bone impaction, with a sensitivity of 100% and a specificity of 93.7%. They concluded that CT is a technique with no false-negatives and could thus prevent many unnecessary esophagoscopies. An additional retrospective study [
16] also reported that noncontrast CT may be a useful first-line radiological tool for the early diagnosis of esophageal foreign bodies. In this study, we also find that the noncontrast CT was a very useful tool for diagnosis of fish bone in esophagus.
In treating an esophageal foreign body, the treatment method differs according to the location of the foreign body, age and clinical state of the patient, and the size, shape and type of foreign body, and technical ability of the medical practitioner performing the endoscopy [
17]. In the past, esophageal foreign bodies were removed through surgery, but removal using an endoscope has been possible since the development of the rigid endoscope in the 1930s. After the flexible endoscope was developed, more effective removal of foreign bodies was possible. Treatment for esophageal foreign bodies can be performed using a rigid or flexible endoscope. Regarding rigid endoscopes, it is known that a variety of equipment is available and that the field of vision is good [
18], but it has the disadvantage that general anesthesia is required. However, with flexible endoscopes, an experienced practitioner can remove foreign bodies without general anesthesia. Recently, the use of TNE to remove esophageal foreign bodies has been reported [
9]. According to this report, TNE could be performed in an outpatient room under local anesthesia without sedation. In our study, all procedures were performed under local anesthesia without sedation and there were no complications associated with TNE. The TNE was well tolerated by all patients and was classified on average as "low-grade unpleasant". Because TNE can be performed without sedation or general anesthesia in nearly all patients, there are none of the risks associated with sedation agents or asphyxia by sedation. In addition, TNE does not require fasting, so it can be performed more quickly. Of course, large foreign bodies with sharp edges may be difficult to remove, and complications such as edema or bleeding in the mucous membrane can occur in the case of failure. Although the foreign bodies in this study were sharp pieces of fish bone, there were no difficulties in removing the fish bones through TNE; thus, the structure was clearly evaluated in the CT before the procedure. Hence, there were no occurrences of complications after treatment. Some case of fish bone was slipped to the stomach during the TNE procedure. It was TNE procedure stimulated the esophagus peristalsis or the air from the TNE push the fish bone to the stomach.
The TNE and noncontrast CT was useful tools for diagnosis and treatment of fish bone impaction in esophagus. However, it is thought that individualized diagnostic and therapeutic approach by clinical circumstances according to the size and species of fish bone and aspect of clinical symptom could facilitate the more reasonable and cost effective decision-making.
In conclusion, fish bone impaction in the esophagus appeared to be more common in older patients. Incorporating noncontrast CT and TNE can facilitate decision-making and adequate treatment for patients with fish bone impaction.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download