Abstract
Objectives
Speech intelligibility is severely affected in children with congenital profound hearing loss. Hypernasality is a problem commonly encountered in their speech. Auditory information received from cochlear implants is expected to be far superior to that from hearing aids. Our study aimed at comparing the percentages of nasality in the speech of the cochlear implantees with hearing aid users and also with children with normal hearing.
Methods
Three groups of subjects took part in the study. Groups I and II comprised 12 children each, in the age range of 4-10 years, with prelingual bilateral profound hearing loss, using multichannel cochlear implants and digital hearing aids respectively. Both groups had received at least one year of speech therapy intervention since cochlear implant surgery and hearing aid fitting respectively. The third group consisted of age-matched and sex-matched children with normal hearing. The subjects were asked to say a sentence which consisted of only oral sounds and no nasal sounds ("Buy baby a bib"). The nasalance score as a percentage was calculated.
Results
Statistical analysis revealed that the children using hearing aids showed a high percentage of nasalance in their speech. The cochlear implantees showed a lower percentage of nasalance compared to children using hearing aids, but did not match with their normal hearing peers.
Conclusion
The quality of speech of the cochlear implantees was superior to that of the hearing aid users, but did not match with the normal controls. The study suggests that acoustic variables still exist after cochlear implantation in children, with hearing impairments at deviant levels, which needs attention. Further research needs to be carried out to explore the effect of the age at implantation as a variable in reducing nasality in the speech and attaining normative values in cochlear implantees, and also between unilateral versus bilateral implantees.
The sense of hearing is essential for speech and language development in children. Congenital hearing loss can cause language delay as well as deviancies in their articulation and voice. A common problem in the speech of hearing-impaired children is hypernasality. They produce nonnasal phonemes as nasalized [1]. The increase in nasal resonance in these subjects has been attributed to the faulty placement of the tongue towards the back of the mouth, or to inefficient control of the velopharyngeal (VP) valve as a consequence of absent auditory feedback [2].
Hearing aids amplify sounds, whereas a cochlear implant instead sends sound signals directly to the auditory nerve. A cochlear implant is a prosthetic device which converts sound energy to electrical energy which stimulates the auditory nerve with coded electrical impulses [34]. Speech frequencies are better represented in cochlear implants and hence provide a more natural representation of speech sounds [5]. Although cochlear implants do not restore sound perception, the implant provides the user with auditory feedback in the domains of timing, intensity, and frequency of sound. Auditory information received and speech perception using cochlear implants are expected to be far superior to that offered by hearing aids.
Nasalance is an objective measure of the nasality of speech. It represents the ratio of nasal acoustic energy to total acoustic energy (i.e., both nasal and oral), and it is expressed as a percentage [6]. Not many studies have been done on the effect of cochlear implantation on hypernasality of speech, and the available studies are limited to adult implantees [78]. These studies revealed that a significant improvement in nasality was not observed following implantation in adults.
The aim of our study was to determine how superior is the speech of the cochlear implantees in terms of nasality compared to hearing aid users, and also to compare the nasality in the speech of cochlear implantees with children with normal hearing.
The approval of the Ethics Committee was obtained before initiating the study. Informed consent was obtained from the parents of all the participants in this study.
Subjects for the study consisted of three groups. Group I comprised 12 cochlear implantees using a multichannel cochlear implant, with prelingual bilateral profound hearing loss, and in the age range of 4-10 years. All of them were implanted only unilaterally after the age of three years, had used digital hearing aids prior to implantation, and had received at least one year of intervention post cochlear implant surgery. All these children were attending four hours of auditory verbal therapy per week from a qualified Speech Language Pathologist, and were attending a normal integrated preschool or school as well.
The second group consisted of 12 children with prelingual bilateral severe to profound hearing loss, in the age range of 4-10 years. All the children were binaurally fitted with digitally programmable hearing aids. No frequency modulation systems were used by any of the children. All these children were attending a minimum of four hours of speech language therapy per week from a qualified Speech Language Pathologist after hearing aid fitting, and had done so for at least one year. All the children were attending a normal integrated preschool or school as well.
The third group consisted of age-matched and sex-matched children with normal hearing. Exclusion criteria included the presence of (1) structural anomalies of the palate (e.g., cleft palate), (2) neuromuscular disorders, (3) cognitive delay, (4) common colds and nasal congestion.
Table 1 sets out the details regarding duration of hearing loss for both groups 1 and 2. The average aided response for the different frequencies by hearing aid users and cochlear implantees is given in Table 2.
The average scores obtained by hearing aid users and cochlear implantees in the picture test of speech perception in Malayalam [9] was 20% for the hearing aid users and 70% for the cochlear implantees. The picture test of speech perception in Malayalam is a standardized test for the age group of 3 to 6.5 years. It involves coloured pictures and a pointing task, and consists of a list of 50 phonetically balanced, bisyllabic, closed set words in Malayalam (a Dravidian language of south India). The test is administered in a audiometric double room setup. Stimulus was presented only through auditory modality and no visual cues were given.
The speech and language therapy sessions for the hearing aid users involved visual, tactile and proprioceptive feedback along with auditory modality, in order for them to learn the different articulatory positions and movement of articulators for production of sounds. The therapy sessions for the cochlear implantees were purely with auditory modality (auditory verbal therapy).
The benefit of using hearing aids was assessed using meaningful use of speech and auditory skills [10] (meaningful auditory integration scale), the Malayalam language test [11], and meaningful use of speech scale [12]. Table 3 shows the benefit of hearing aids, tested using meaningful use of speech scale, meaningful auditory integration scale, and the Malayalam language test.
The subjects were asked to say a sentence which consisted of oral sounds and no nasal sounds ("Buy baby a bib"). The speech stimuli were recorded from each participant individually in a sound treated room with an ambient noise below 40 dB, using a computer-based system of Nasal view developed by Tiger Electronics Inc. (Dr Speech; North Reading, MA, USA). The Nasal view is equipped with a sound plate that separates and measures sound energy emanating from the oral and nasal cavities. The instrument's software then calculates the nasalance score as a percentage. Before initiating data collection, the nasal view was calibrated in a sound treated booth, following the procedures outlined in the manual.
The statistical analysis was carried out using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). A one-way analysis of variance (ANOVA) and multiple comparisons using Bonferroni were performed to compare the three groups.
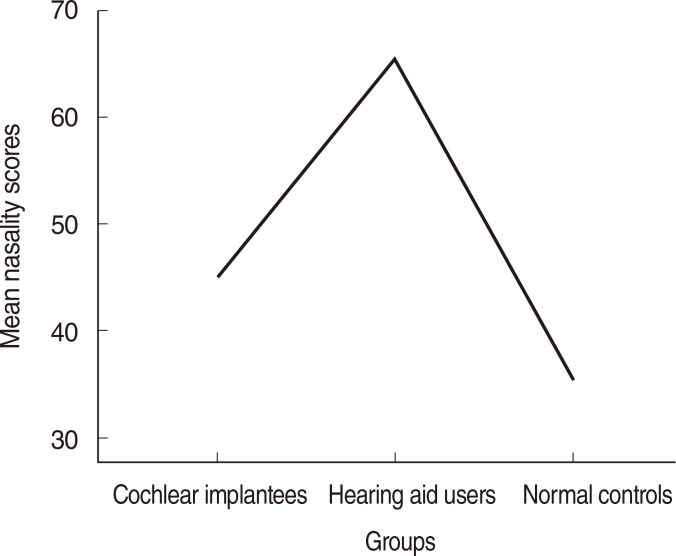
The mean nasalance score was 65.54% for the hearing aid users group, 45.0% for the cochlear implantees, and 35.37% for the normal control group (Fig. 1). One-way ANOVA revealed a statistically significant differences between all three groups (P<0.001) (Table 4). Each group was compared with the other two groups using the Bonferroni test (Table 5).
Even though there was a significant difference (P<0.001) between the normal controls and the hearing aid users as well as the cochlear implant users, the speech of the hearing aid users were far inferior to that of the cochlear implant users. The speech of the cochlear implantees was superior to that of hearing aid users but did not match with the normal controls.
Hearing-impaired children show hypernasality in their speech, which makes speech intelligibility poor [13]. Resonance disorder, especially hypernasality, is reported as a common problem in the speech of deaf adults and children [261415161718]. Research conducted into the characteristics of deaf speech of prelingual deaf individuals has revealed excessive nasality and/or resonance irregularities [1418]. Research has also shown that post lingual deaf adults, after prolonged hearing loss, can develop voice and speech abnormalities similar to prelingual deaf adults, including deviations in nasality [19].
The main purpose of the present study was to examine the effect of cochlear implantation on hypernasality of the speech of hearing-impaired children. Statistical analysis revealed that the nasalance scores were significantly higher in hearing-impaired children, compared to their peers with normal hearing.
LaPine et al. [20] studied the effect of hearing amplification on nasalance in children. They did not report any significant differences in nasalance scores between the aided and unaided conditions. Nasalance scores were found to be significantly higher in the hearing-impaired than in individuals with no hearing impairment, regardless of the degree of hearing loss, age, or the frequency of using hearing aids [2021].
The speech of the cochlear implantees was superior to that of the hearing aid users but did not match the normal controls. The nasalance scores of the cochlear implantees were significantly lower than those of the hearing aid users group, but were higher than those of the normal control group. This may be suggestive of the fact that increased nasality in the speech of children with congenital hearing loss is due to the inability of deaf speakers to monitor VP valving with auditory feedback.
There is a tendency in the present study towards improved nasalance scores after implantation, which highlights the role of auditory feedback in monitoring VP function. Auditory information contributes to the acquisition and maintenance of speech [22]. Children learn to relate their own auditory feedback to their articulatory gestures, and they learn how the consequences of their articulatory gestures compare to sounds that are produced by other talkers. Finally, children may learn to monitor their auditory feedback for the purpose of fine-tuning their continuing articulatory behavior, and for detecting speech sound errors [22].
The present study supports the earlier finding that acoustic variables still exist after cochlear implantation in children with hearing impairments at deviant levels [23], which needs to be addressed during speech therapy.
The scores are expected to be superior if the same study were to be conducted on children implanted at a younger age, before the critical period when the brain is still learning to interpret sound. Further research needs to be carried out to explore the effect of age at implantation as a variable in reducing nasality in speech and attaining normative values in cochlear implantees. Research also needs to be done comparing the nasality scores before and after cochlear implant surgery, and also between unilateral implantees and bilateral implantees.
In conclusion, the quality of speech of the cochlear implantees was superior to that of the hearing aid users, but did not match with the normal controls. Further research needs to be carried out to explore the effect of age at implantation as a variable in reducing nasality in speech and attaining normative values in cochlear implantees, and also between unilateral versus bilateral implantees.
ACKNOWLEDGMENTS
We are greatly indebted to Biostatistics Unit, Christian Medical College, for statistical analyses and interpretation of data.
References
1. Hudgins CV, Numbers FC. An investigation of the intelligibility of the speech of the deaf. Provincetown (MA): The Journal Press;1942.
2. Stevens KN, Nickerson RS, Boothroyd A, Rollins AM. Assessment of nasalization in the speech of deaf children. J Speech Hear Res. 1976; 6. 19(2):393–416. PMID: 790016.

3. House WF. Cochlear implants. Ann Otol Rhinol Laryngol. 1976; May-Jun. 85(Suppl 27):(3Pt2):1–93. PMID: 779582.

4. Staller SJ. Cochlear implant characteristics: a review of current technology. Semin Hear. 1985; 2. 6(1):23–32.

5. Hoth S. Indication for the need of flexible and frequency specific mapping functions in cochlear implant speech processors. Eur Arch Otorhinolaryngol. 2007; 2. 264(2):129–138. PMID: 17004087.

6. LaPine PR, Stewart MG, Tatchell J. Application of nasometry to speech samples of hearing-impaired children. Percept Mot Skills. 1991; 10. 73(2):467–475. PMID: 1766773.

7. Plant G, Oster AM. The effects of cochlear implantation on speech production: a case study. STL-QPSR. 1986; 27(1):65–86.
8. Langereis MC, Dejonckere PH, van Olphen AF, Smoorenburg GF. Effect of cochlear implantation on nasality in post-lingually deafened adults. Folia Phoniatr Logop. 1997; 49(6):308–314. PMID: 9415736.

9. Mathew P, Yathiraj A. A picture test of speech perception in Malayalam [master's thesis]. Mysuru: University of Mysore;1996.
10. Zimmerman-Phillips S, Osberger MJ, Robbins AM. Infant-toddler meaningful auditory integration scale. Sylmar (CA): Advanced Bionics Co.;2001.
11. RukminiA P. Malayalam language test [master's thesis]. Mysuru: University of Mysore;1994.
12. Robbins AM, Osberger MJ. Meaningful use of speech scale. Indianapolis: Indiana University School of Medicine Press;1991.
13. Evans MK, Deliyski DD. Acoustic voice analysis of prelingually deaf adults before and after cochlear implantation. J Voice. 2007; 11. 21(6):669–682. PMID: 16952440.

14. Colton RH, Cooker HS. Perceived nasality in the speech of the deaf. J Speech Hear Res. 1968; 9. 11(3):553–559. PMID: 5722479.

15. Fletcher SG, Higgins JM. Performance of children with severe to profound auditory impairment in instrumentally guided reduction of nasal resonance. J Speech Hear Disord. 1980; 5. 45(2):181–194. PMID: 7442151.

16. Lock RB, Seaver EJ 3rd. Nasality and velopharyngeal function in five hearing impaired adults. J Commun Disord. 1984; 2. 17(1):47–64. PMID: 6715568.

17. Ysunza A, Vazquez MC. Velopharyngeal sphincter physiology in deaf individuals. Cleft Palate Craniofac J. 1993; 3. 30(2):141–143. PMID: 8452833.

18. Fletcher SG, Mahfuzh F, Hendarmin H. Nasalance in the speech of children with normal hearing and children with hearing loss. Am J Speech Lang Pathol. 1999; 8. 8(3):241–248.

19. Leder SB, Spitzer JB. A perceptual evaluation of the speech of adventitiously deaf adult males. Ear Hear. 1990; 6. 11(3):169–175. PMID: 1967115.

20. LaPine PR, Stewart MG, Settle SV, Brandow M. Examining the effects of amplification on the nasalance ratios of hearing-impaired children. Folia Phoniatr (Basel). 1992; 44(5):185–193. PMID: 1490643.

21. Fletcher SG, Daly DA. Nasalance in utterances of hearing-impaired speakers. J Commun Disord. 1976; 3. 9(1):63–73. PMID: 965505.

22. Tye-Murray N. Articulatory organizational strategies and the roles of audition. Volta Rev. 1992; 7. 94(3):243–259.
23. Higgins MB, McCleary EA, Ide-Helvie DL, Carney AE. Speech and voice physiology of children who are hard of hearing. Ear Hear. 2005; 12. 26(6):546–558. PMID: 16377992.

Table 1.
Details regarding duration of hearing loss for both groups 1 and 2
Table 2.
The average aided response for the different frequencies by hearing aid users and cochlear implantees
|
Frequency (Hz) |
||||||
|---|---|---|---|---|---|---|
| 250 | 500 | 1,000 | 2,000 | 4,000 | 8,000 | |
| Hearing aid users | 35 | 35 | 40 | 40 | 40 | 45 |
| Cochlear implantees | 15 | 20 | 25 | 20 | 30 | 25 |
Table 3.
The benefit of hearing aid tested using meaningful use of speech scale, meaningful auditory integration scale and Malayalam language test
|
Average score |
|||
|---|---|---|---|
| Meaningful use of speech scale | Meaningful auditory integration scale | Malayalam language test | |
| Before intervention | 2 | 0 | 9 |
| After intervention | 16 | 12 | 82 |
Table 4.
The results of one-way analysis of variance
| Group | Nasality (%), mean±SD (range) | P-value |
|---|---|---|
| Cochlear implantees | 45.00±3.24 (40.00–50.00) | <0.001 |
| Hearing aid users | 65.54±2.66 (60.00–70.00) | |
| Normal peers | 35.37±0.88 (34.00–36.50) |




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download