1. Males AG, Gray RF. Mastoid misery: quantifying the distress in a radical cavity. Clin Otolaryngol Allied Sci. 1991; 2. 16(1):12–14. PMID:
2032350.

2. Whittemore KR Jr, Merchant SN, Rosowski JJ. Acoustic mechanisms: canal wall-up versus canal wall-down mastoidectomy. Otolaryngol Head Neck Surg. 1998; 6. 118(6):751–761. PMID:
9627232.
3. Shelton C, Sheehy JL. Tympanoplasty: review of 400 staged cases. Laryngoscope. 1990; 7. 100(7):679–681. PMID:
2362526.
4. Takahashi H, Iwanaga T, Kaieda S, Fukuda T, Kumagami H, Takasaki K, et al. Mastoid obliteration combined with soft-wall reconstruction of posterior ear canal. Eur Arch Otorhinolaryngol. 2007; 8. 264(8):867–871. PMID:
17340129.

5. Gantz BJ, Wilkinson EP, Hansen MR. Canal wall reconstruction tympanomastoidectomy with mastoid obliteration. Laryngoscope. 2005; 10. 115(10):1734–1740. PMID:
16222186.

6. Kim SH, Kang MK, Ahn JK, Han CS, Gu TW. Epitympanoplasty with mastoid obliteration technique in middle ear surgery:12-year result. J Int Adv Otol. 2009; 5(1):24–30.
7. Shea MC Jr, Gardner G Jr, Simpson ME. Mastoid obliteration using homogenous bone chips and autogenous bone paste. Trans Am Acad Ophthalmol Otolaryngol. 1972; Jan-Feb. 76(1):160–172. PMID:
4337026.
8. Grote JJ. Results of cavity reconstruction with hydroxyapatite implants after 15 years. Am J Otol. 1998; 9. 19(5):565–568. PMID:
9752961.
9. Lee HB, Lim HJ, Cho M, Yang SM, Park K, Park HY, et al. Clinical significance of β-tricalcium phosphate and polyphosphate for mastoid cavity obliteration during middle ear surgery: human and animal study. Clin Exp Otorhinolaryngol. 2013; 9. 6(3):127–134. PMID:
24069514.

10. Jang CH, Park H, Cho YB, Song CH. Mastoid obliteration using a hyaluronic acid gel to deliver a mesenchymal stem cells-loaded demineralized bone matrix: an experimental study. Int J Pediatr Otorhinolaryngol. 2008; 11. 72(11):1627–1632. PMID:
18786734.

11. Leatherman BD, Dornhoffer JL. The use of demineralized bone matrix for mastoid cavity obliteration. Otol Neurotol. 2004; 1. 25(1):22–25. PMID:
14724487.

12. Cho SW, Cho YB, Cho HH. Mastoid obliteration with silicone blocks after canal wall down mastoidectomy. Clin Exp Otorhinolaryngol. 2012; 3. 5(1):23–27. PMID:
22468198.

13. Black B. Mastoidectomy elimination. Laryngoscope. 1995; 12. 105(12 Pt 2 Suppl 76):1–30. PMID:
7500804.

14. Black B. Mastoidectomy elimination: obliterate, reconstruct, or ablate? Am J Otol. 1998; 9. 19(5):551–557. PMID:
9752959.
15. Leatherman BD, Dornhoffer JL, Fan CY, Mukunyadzi P. Demineralized bone matrix as an alternative for mastoid obliteration and posterior canal wall reconstruction: results in an animal model. Otol Neurotol. 2001; 11. 22(6):731–736. PMID:
11698788.

16. Moon BJ, Lee HJ, Jang YJ. Outcomes following rhinoplasty using autologous costal cartilage. Arch Facial Plast Surg. 2012; May-Jun. 14(3):175–180. PMID:
22801761.

17. Siegert R. Combined reconstruction of congenital auricular atresia and severe microtia. Laryngoscope. 2003; 11. 113(11):2021–2027. PMID:
14603067.

18. Cotton RT, Myer CM 3rd, O'Connor DM, Smith ME. Pediatric laryngotracheal reconstruction with cartilage grafts and endotracheal tube stenting: the single-stage approach. Laryngoscope. 1995; 8. 105(8 Pt 1):818–821. PMID:
7630293.

19. Uppal RS, Sabbagh W, Chana J, Gault DT. Donor-site morbidity after autologous costal cartilage harvest in ear reconstruction and approaches to reducing donor-site contour deformity. Plast Reconstr Surg. 2008; 6. 121(6):1949–1955. PMID:
18520880.

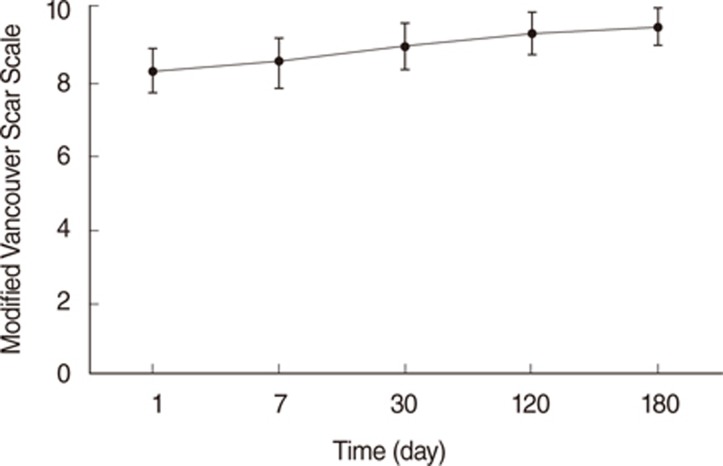
20. Baryza MJ, Baryza GA. The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil. 1995; Sep-Oct. 16(5):535–538. PMID:
8537427.

21. Draaijers LJ, Tempelman FR, Botman YA, Tuinebreijer WE, Middelkoop E, Kreis RW, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004; 6. 113(7):1960–1965. PMID:
15253184.

22. Rasp G, Staudenmaier R, Ledderose H, Kastenbauer E. Autologous rib cartilage harvesting: operative procedure and postoperative pain reduction. Laryngorhinootologie. 2000; 3. 79(3):155–159. PMID:
10763173.
23. Chepla KJ, Salgado CJ, Tang CJ, Mardini S, Evans KK. Late complications of chest wall reconstruction: management of painful sternal nonunion. Semin Plast Surg. 2011; 2. 25(1):98–106. PMID:
22294948.

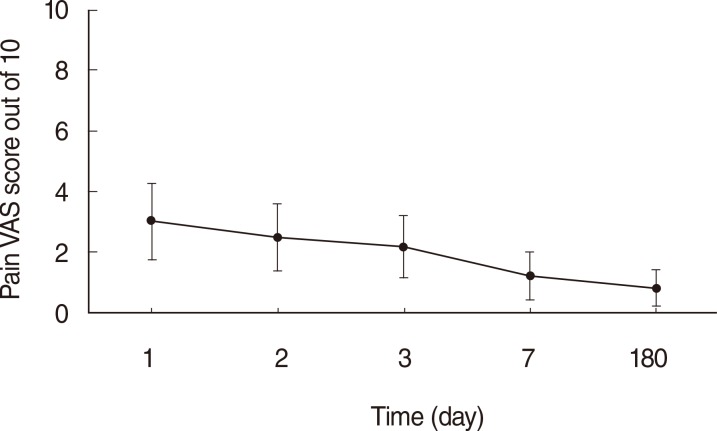
24. Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976; 6. 2(2):175–184. PMID:
1026900.

25. Joyce CR, Zutshi DW, Hrubes V, Mason RM. Comparison of fixed interval and visual analogue scales for rating chronic pain. Eur J Clin Pharmacol. 1975; 8. 8(6):415–420. PMID:
1233242.

26. Jensen MP, McFarland CA. Increasing the reliability and validity of pain intensity measurement in chronic pain patients. Pain. 1993; 11. 55(2):195–203. PMID:
8309709.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download