This article has been retracted. See "A Prospective Study of the Surgical Outcome of Simple Uvulopalatopharyngoplasty (UPPP), UPPP Combined With Genioglossus Advancement or Tongue Base Advancement for Obstructive Sleep Apnea Hypopnea Syndrome Patients With Multilevel Obstruction" in Volume 9 on page 387.
Abstract
Methods
All subjects underwent overnight polysomnography and were evaluated using the Epworth sleepiness scale (ESS), the Quebec sleep questionnaire and the snoring scale at the baseline and 3 and 12 months following operation. The primary endpoint was the overall effective rate representing the sum of the surgical success rate and effective rate.
Results
The overall effective rate at 12 months post surgery was 55.6% for simple UPPP, 95.8% for UPPP+GA, and 92.3% for UPPP+TBA. The surgical success rate at 3 and 12 months postoperation for UPPP+GA or UPPP+TBA was significantly higher than simple UPPP (P<0.05). Marked improvement was observed in all patients in the snoring scale score and the ESS score 3 and 12 months following surgery compared to the baseline (P<0.05 in all).
Obstructive sleep apnea hypopnea syndrome (OSAHS) is the most prevalent sleep disorder, affecting up to one quarter of the general population, depending on gender, age and definition of OSAHS [1]. It causes significant morbidity in the patients and also associated with excessive daytime sleepiness and impairs the quality of life. Airway obstruction is often present at multiple levels of the upper aiway in moderate and severe OSAHS patients. Continuous positive airway pressure (CPAP) is regarded as the gold standard for treating OSAHS with mandibular reposition appliance or surgery in reserve for CPAP failures. Simple uvulopalatopharyngoplasty (UPPP) remains the most common surgical procedure performed for OSAHS, but it only tackles obstruction at the soft palate while it does not address obstruction at the tongue base. The reported success rate of simple UPPP as a treatment of OSAHS also varies among surgeons, ranging from 16% to 83% [2,3,4]. As OSAHS patients often have obtruction at the multiple levels of the upper airway, simple UPPP is frequently inadequate [2]. Often, combination of UPPP with other nasopharyngeal or oropharyngeal procedures is required in order to achieve a satisfactory outcome. Riley et al. [5] were the first to carry out phase I multiple level surgery for OSAHS patients with obstruction at multiple levels by using genioglossus advancement (GA) combined with hyoid suspension for obstruciton at the soft palate.
Current surgical approaches for obstruction at the tongue base include radiofrequency tongue base ablation, partial glossectomy, GA, and hyoid suspension [6]. The Repose GA procedure has recently gained wider use because of its minimally invasive nature, but its long term effect and surgical indications remain controversial [7]. In the current single center parallel group study, we prospectively investigated the surgical outcomes of simple UPPP, UPPP combined with GA (UPPP+GA) and hyoid suspension or UPPP combined with tongue base advancement (TBA) using the Repose system (UPPP+TBA) for OSAHS patients with obstruction at multiple levels.
We prospectively studied OSAHS patients who received surgical treatment at our hospital between January 2009 and January 2011. OSAHS was diagnosed according to the 2009 Guidelines for OSAHS Diagnosis and Surgical Treatment in China [8]. A subject was excluded (1) if he or she had nasal stenosis, (2) if his or her body mass index (BMI)≥40 kg/m2, and (3) if he or she had hypothyroidism or acromegaly. All patients refused CPAP and requested surgery. The study protocol was approved by the local Institutional Review Board at the authors' affiliated institutions and patients or their legal surrogates provided informed consent to surgery and the study.
All subjects underwent overnight polysomnography (Embla S7000, Embla, Thornton, CO, USA) prior to surgery and at 3 and 12 months postoperation. Sleep stages were manually scored according to the 2007 American Academy of Sleep Medicine criteria [9]. Apnea was defined as a reduction of >90% in oronasal airflow lasting ≥10 seconds and hypopnea as a decrease of >30% in oronasal airflow lasting ≥10 seconds and associated with ≥4% desaturation from the pre-event baseline. The apnea hyponea index (AHI) was defined as the mean number of apneas and hypopneas per hour during sleep. OSAHS was defined when AHI was ≥5 events/hour. An AHI score of 5-14 was considered mild OSAHS, 15-29 was considered moderate OSAHS, and ≥30 was considered severe OSAHS [9]. The percentage of time spent at SaO2 below 90% (CT90) was calculated and LSO2 represented the lowest oxygen saturation.
Patients were evaluated using the Epworth sleepiness scale (ESS) [5], a questionnaire for assessing subjective daytime sleepiness, the Quebec sleep questionnaire (QSQ) [10] and the snoring scale at the baseline and 3 and 12 months following operation. The Chinese version ESS has been validated [11], with scores ranging from 0 to 24 with higher scores representing more severe daytime sleepiness. The Chinese version QSQ has been validated for use in Chinese patients [12] and includes 5 domains with scores ranging from 1 to 7 for each domain and the total QSQ score is an average of the 5 domain scores with higher scores representing better quality of life. The snoring scale assessed patients for loudness of snores and impact on others with scores ranging from 1 to 10 with 10 being the loudest. Snoring was recorded through a piezo snoring sensor.
The subjects were assigned to undergo simple UPPP, UPPP+GA, or UPPP+TBA. UPPP involved tonsillectomy, trimming and reorientation of the posterior and anterior tonsillar pillars and excision of the uvula and posterior palate and was performed as previously depicted [13]. GA and hyoid suspension [14] was undertaken as previously reported [15] and TBA with fixation was done using the Repose Tongue and Hyoid Suspension System (Influent Inc., San Francisco, CA, USA).
Cure was defined as AHI<5/hour, surgical success was defined as an AHI reduction of at least 50% and AHI reduction to below 20/hour, and effectiveness was defined as a ≥50% reduction in AHI but AHI was ≥20/hour. Ineffective was defined as a <50% reduction in AHI. Overall effective rate represented the sum of the surgical success rate and effective rate. In addition, surgical complications were recorded.
The SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Kolmogorov-Smirnov test was used for testing normal distribution of data. Normally distributed was expressed as X±SD or percentage, and Student t-test was used for comparing differences between groups, and variance analysis was used for comparison among three groups. Nonnormally distributed data were presented as median and interquartile range (IQR) and analyzed using the. Mann-Whitney rank test was used to compare differences between groups and Wilcoxon Signed rank test was used to compare ESS scores. The primary endpoint of this study was overall effective rate and the secondary endpoints were changes in ESS, QSQ, and snoring scale scores and changes in Changes in AHI, LSO2, and CT90. P<0.05 was considered statistically significant.
The study flowchart is shown in Fig. 1. One hundred twenty seven patients were screened for eligibility for the study and 89 patients met the inclusion criteria. Among them, 29 patients received simple UPPP, 30 patients underwent UPPP+GA, and 30 patients received UPPP+TBA using the Repose system. Twelve patients were excluded from analysis due to incomplete data. As a result, 77 were finally enrolled in this study including 27 receiving simple UPPP, 24 receiving UPPP+GA and 26 receiving UPPP+TBA. The demographic and baseline characteristics of the study participants are shown in Fig. 1. The patients receiving simple UPPP, UPPP+GA, and UPPP+TBA were comparable in demographic and baseline characteristics (Table 1). They had a mean age of 43 years and all of the patients were male (100%). Friedman staging identified 4 patients (5.2%) in stage I, 35 patients (45.5%) in stage II, and 39 patients (50.6%) in stage III. Their mean AHI was 46.23±15.58 (range, 21.85 to 66.62) events/hour; their SpO2 was 68.37±10.25 (range, 58.82 to 83.63); their mean CT90 was 25.24±5.83 (range, 18.45 to 33.25). Patients receiving simple UPPP, UPPP+GA, and UPPP+TBA had comparable AHI, SpO2, and CT90 (P>0.05). The median ESS score for the study subjects was 9.5 (IQR, 5 to 14); their median QSQ score was 3.8 (IQR, 2 to 6); their median snoring score was 8.0 (IQR, 3 to 13). Patients receiving simple UPPP, UPPP+GA, and UPPP+TBA were comparable in ESS, QSQ, and snoring scores (P>0.05).
No patients receiving any of the surgical treatments developed edema of the pharynx, breathing difficulties and pharynx incompetency postoperatively. The surgical outcomes are shown in Table 2. At 3 months, the surgical success rate for OSAHS patients undergoing simple UPPP was 14.8% (4/27), the effective rate was 70.4% (19/27), and the ineffective rate was 14.8% (4/27). The overall effective rate was 85.2%. At 12 months postsurgery, the surgical success rate was 7.4% (2/27), the effective rate was 48.1% (13/27), and the ineffective rate was 44.4% (12/27) with an overall effective rate of 55.6%. The surgical success rate at 3 months for OSAHS patients undergoing UPPP+GA was 20.8% (5/24), the effective rate was 75% (18/24), and the ineffective rate was 4.16% (1/24). The overall effective rate was 95.8%. At 12 months post surgery, the surgical success rate was 12.5% (3/24), the effective rate was 62.5% (15/24), and the ineffective rate 25% (6/24) with an overall effective rate of 75%. The surgical success rate at 3 months for OSAHS patients undergoing UPPP+TBA was 34.6% (9/26), the effectiveness rate was 65.4% (17/26), and the ineffective rate was 0%. The overall effective rate was 100%. At 12 months post surgery, the surgical success rate was 26.9% (7/26), the effective rate was 65.4% (17/26), and the ineffective rate was 7.7% (2/26) with an overall effective rate of 92.3%. The surgical success rate at 3 and 12 months post operation for OSAHS patients undergoing UPPP+GA or UPPP+ TBA was significantly higher than patients receiving simple UPPP (P<0.05). The overall effective rate at 12 months post surgery was the highest for patients undergoing UPPP+TBA, which was markedly higher than patients receiving either simple UPPP or UPPP+ GA (P<0.05).
Patients receiving simple UPPP, UPPP+GA, and UPPP+TBA all showed marked improvement in the snoring scale score and the ESS score 3 and 12 months following surgery compared to the baseline scores (P<0.05 in all). No statistically significant improvement in the QSQ scores was observed in patients receiving simple UPPP or UPPP+GA compared to the baseline scores (P>0.05 in both). By contrast, the median QSQ score of patients receiving UPPP+TBA improved from 4 (IQR, 2,6) at the baseline to 6.5 (IQR, 6,7) at 12 months post surgery (P<0.05). At 12 months following surgery, patients receiving simple UPPP, UPPP+GA, and UPPP+TBA had comparable ESS, QSQ, and snoring scores (P>0.05) (Table 3).
Patients receiving simple UPPP, UPPP+GA, and UPPP+TBA all showed marked improvement in the mean AHI, LSO2, and CT90 scores 3 and 12 months following surgery compared to the baseline scores (P<0.05 in all). Furthermore, patients receiving UPPP+GA and UPPP+TBA had statistically greater reduction in the AHI scores than patients receiving UPPP (P<0.05). No statistically significant difference was observed in the LSO2, and CT90 scores 3 and 12 months following surgery among patients receiving simple UPPP, UPPP+GA, and UPPP+TBA (P> 0.05) (Table 4).
No patients who received OSAHS developed edema of the pharynx, breathing difficulties and pharynx incompetency postoperatively. After UPPP, there may be haemorrhage, temporary velopharyngeal insufficiency and infection. Two patients (6%) who received UPPP+GA developed fracture of the mandible and one patient (3%) had fracture of the titanium miniplate (1 case, 3%). Four patients (13%) felt pressure on lower front teeth, especially during mastication and maximum opening, and two patients (6%) lost lower incisor tooth vitality. Atypical chronic facial pain in the inferior alveolar nerve area was present in one patient (3%). Furthermore, one patient suffered from a persistent fistula and aphonia 33 weeks after the operation. Apparent pain and dysarthria occurred in the immediate postoperative period in patients who underwent UPPP+TBA, which disappeared within 7 to 14 days. Of the 19 patients who underwent the procedure, complications developed in 5 (26.3%). Acute submandibular sialadenitis requiring antibiotic treatment developed in 2 patients (10.5%) both responded well to conservative treatment. Two patients (10.5%) developed hematoma in the mouth floor necessitating transoral drainage. One patient (5.3%) had extrusion of the suture 4 weeks postoperatively, and 1 patient (5.3%) had a persistent globus sensation in the tongue base necessitating suture removal 6 weeks postoperatively.
Mild OSAHS is predominantly manifested as palatal obstruction while obstruction at the tongue base is less commonly seen. On the other hand, severe OSAHS is characterized by multilevel obstruction with involvement of the tongue base in virtually all patients. Simple UPPP only tackles obstruction at the soft palate and does not address obstruction at the tongue base. Simple UPPP as a treatment of OSAHS has only achieved variable success is frequently inadequate for severe OSAHS. Our study compared the efficacy of simple UPPP, UPPP+GA, and UPPP+TBA for OSAHS patients with multilevel obstruction. The study population not only consists of isolated palate surgery patients but also included patients who concurrently underwent tongue base surgery. To our best knowledge, so far, there have been no previous prospective studies on the combination approach of OSAHS.
The 12-month success rates for our patients with moderate to severe OSA are 7.4% for UPPP, 12.5% for UPPP+GA, and 26.9% for UPPP+TBA, respectively, and the overall 12-month effective rates are 55.6% for UPPP, 75% for UPPP+GA, and 92.3% for UPPP+TBA, respectively. The surgical rate and the overall effective rate for UPPP are in the low range compared with the previously reported series [16,17,18,19,20,21]. It is a clinical reality in sleep surgery that remarkable differences in outcome can occur amongst patients with comparable preoperative AHI, BMI, and other clinicopathologic findings. The variable rates for OSAHS may also be attributed to differing definitions of surgical success. Kahn et al. [22] have defined surgical success or cure after UPPP as a 50% reduction in the AHI, whereas others combine this criterion with an absolute AHI of 20 or less as occurred in our current study.
Our findings further indicate that simple UPPP is less effective than either UPPP+GA or UPPP+TBA, suggesting that simple UPPP is inadequate as first-line therapy for moderate to severe OSAHS. The 12-month success rate for our patients with moderate to severe OSA treated with UPPP+GA or UPPP+TBA doubles that of patients treated with simple UPPP. Though 92.3% of our patients demonstrated an effective response to UPPP+TBA at 12-month postsurgery, the 12-month cure rate for these patients was 0%, as is the case with the other two surgical approaches. Increasing evidence shows that, when treating OSAHS, reducing the AHI to less than 5 is necessary to improve health care-related outcome measures, such as hypertension [23]. Therefore, surgical approaches are required that target surgical success for AHI outcomes of 5 or less or 10 or less. We further observed that the overall effective rate declined with longer follow-up for all the three surgical approaches, raising the question about the long term effectiveness of surgical treatment and also indicating for longer follow up of surgical patients.
OSAHS compromises the quality of life of patients. We were interested in whether the surgical treatments were translated into demonstrable benefits in the quality of life of the study subjects. We found no statistically significant improvement in the QSQ scores in patients receiving simple UPPP or UPPP+GA. By contrast, patients receiving UPPP+TBA had significantly improved QSQ scores over baseline, indicating that, compared to UPPP or UPPP+GA, UPPP+TBA is more effective in improving the patient quality of life. Furthermore, out study showed that all patients in this series exhibited statistically significant improvement in the mean AHI, LSO2, and CT90 scores. However, we observed a higher and significant complication rate after UPPP+ TBA compared to UPPP alone.
In conclusion, UPPP, UPPP+GA, and UPPP+TBA are all effective in improving the surgical outcome of OSAHS patients with multilevel obstruction. UPPP+TBA is the most effective in treating OSAHS patients. However, our findings need to be further confirmed by prospective studies of larger patient size.
References
1. Rangel AJ, Barros VD, Seraidarian PI. Snoring and obstructive sleep apnea syndrome: a reflection on the role of dentistry in the current scientific scenario. Dental Press J Orthod. 2012; May-Jun. 17(3):58–63.

2. Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996; 2. 19(2):156–177. PMID: 8855039.

3. Elshaug AG, Moss JR, Southcott AM, Hiller JE. Redefining success in airway surgery for obstructive sleep apnea: a meta analysis and synthesis of the evidence. Sleep. 2007; 4. 30(4):461–467. PMID: 17520790.

4. Carpenter JM, LaMear WR. Uvulopalatopharyngoplasty: results of a patient questionnaire. Ann Otol Rhinol Laryngol. 2008; 1. 117(1):24–26. PMID: 18254367.

5. Riley RW, Powell NB, Guilleminault C, Nino-Murcia G. Maxillary, mandibular, and hyoid advancement: an alternative to tracheostomy in obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 1986; 94(5):584–588. PMID: 3088520.

6. Handler E, Hamans E, Goldberg AN, Mickelson S. Tongue suspension: an evidence-based review and comparison to hypopharyngeal surgery for OSA. Laryngoscope. 2014; 1. 124(1):329–336. PMID: 23729234.
7. Terris DJ, Kunda LD, Gonella MC. Minimally invasive tongue base surgery for obstructive sleep apnoea. J Laryngol Otol. 2002; 9. 116(9):716–721. PMID: 12437808.

8. Chinese Medical Association of Otolaryngology Branch, Chinese Journal of Otorhinolaryngology Editorial Board. Guideline for diagnosis and surgical treatment of obstructive sleep apnea syndrome. Chin J Otorhinolaryngol Head Neck Surg. 2009; 44:295–296.
9. Iber C, Ancoli-Israel S, Chesson A, Quan S. for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester (IL): American Academy of Sleep Medicine;2007.
10. Lacasse Y, Bureau MP, Series F. A new standardised and self-administered quality of life questionnaire specific to obstructive sleep apnoea. Thorax. 2004; 6. 59(6):494–499. PMID: 15170032.

11. Peng LL, Li JR, Sun JJ, Li WY, Sun YM, Zhang R, et al. Reliability and validity of the simplified Chinese version of Epworth sleepiness scale. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2011; 1. 46(1):44–49. PMID: 21429336.
12. Huo H, Li WY, Liu JH, Tian X, Zhou EH, Chen WD, et al. A simplified Chinese version of the Quebec sleep questionnaire was evaluated for reliability and validity. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2011; 2. 46(2):101–107. PMID: 21426702.
13. Tucker Woodson B. Structural effectiveness of pharyngeal sleep apnea surgery. Sleep Med Rev. 2008; 12. 12(6):463–479. PMID: 19010290.

14. Neruntarat C. Genioglossus advancement and hyoid myotomy: short-term and long-term results. J Laryngol Otol. 2003; 6. 117(6):482–486. PMID: 12818058.

15. Sorrenti G, Piccin O, Latini G, Scaramuzzino G, Mondini S, Rinaldi Ceroni A. Tongue base suspension technique in obstructive sleep apnea: personal experience. Acta Otorhinolaryngol Ital. 2003; 8. 23(4):274–280. PMID: 15046416.
16. Kezirian EJ, Goldberg AN. Hypopharyngeal surgery in obstructive sleep apnea: an evidence-based medicine review. Arch Otolaryngol Head Neck Surg. 2006; 2. 132(2):206–213. PMID: 16490881.
17. Baisch A, Maurer JT, Hormann K. The effect of hyoid suspension in a multilevel surgery concept for obstructive sleep apnea. Otolaryngol Head Neck Surg. 2006; 5. 134(5):856–861. PMID: 16647548.

18. Richard W, Kox D, den Herder C, van Tinteren H, de Vries N. One stage multilevel surgery (uvulopalatopharyngoplasty, hyoid suspension, radiofrequent ablation of the tongue base with/without genioglossus advancement), in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2007; 4. 264(4):439–444. PMID: 17063353.

19. Benazzo M, Pagella F, Matti E, Zorzi S, Campanini A, Frassineti S, et al. Hyoidthyroidpexia as a treatment in multilevel surgery for obstructive sleep apnea. Acta Otolaryngol. 2008; 6. 128(6):680–684. PMID: 18568505.

20. van den Broek E, Richard W, van Tinteren H, de Vries N. UPPP combined with radiofrequency thermotherapy of the tongue base for the treatment of obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2008; 11. 265(11):1361–1365. PMID: 18347810.

21. Yi HL, Sun XQ, Chen B, Zhang YJ, Guan J, Wu HM, et al. Z-palatopharyngoplasty plus genioglossus advancement and hyoid suspension for obstructive sleep apnea hypopnea syndrome. Otolaryngol Head Neck Surg. 2011; 3. 144(3):469–473. PMID: 21493215.

22. Khan A, Ramar K, Maddirala S, Friedman O, Pallanch JF, Olson EJ. Uvulopalatopharyngoplasty in the management of obstructive sleep apnea: the mayo clinic experience. Mayo Clin Proc. 2009; 9. 84(9):795–800. PMID: 19720777.

23. Becker HF, Jerrentrup A, Ploch T, Grote L, Penzel T, Sullivan CE, et al. Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation. 2003; 1. 107(1):68–73. PMID: 12515745.

Fig. 1
The study flowchart. UPPP, uvulopalatopharyngoplasty; GA, genioglossus advancement with hyoid suspension; TBA, tongue base advancement with fixation.
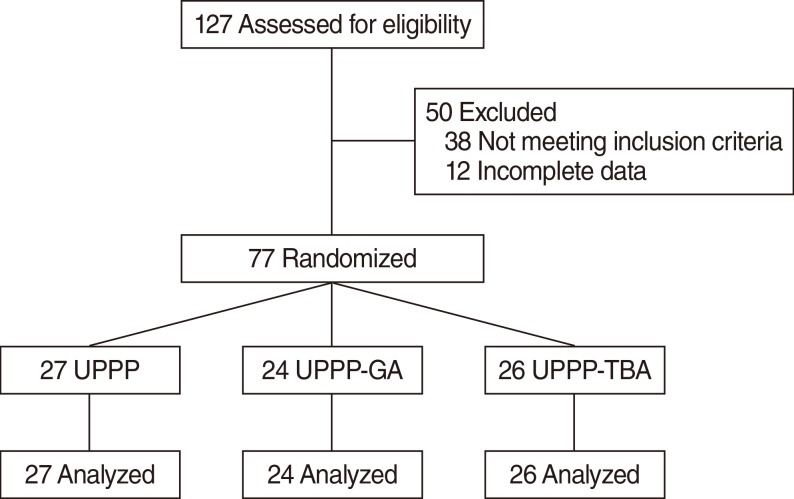
Table 1.
Demographic and baseline characteristics of the study participants
Table 2.
The surgical outcome of OSAHS patients in the study
| Surgical outcome | Simple UPPP (n=27) | UPPP+GA (n=24) | UPPP+TBA (n=26) |
|---|---|---|---|
| Cure rate | |||
| 3 Months postsurgery | 0 | 0 | 0 |
| 12 Months postsurgery | 0 | 0 | 0 |
| Surgical success rate | |||
| 3 Months postsurgery | 14.8 | 20.8 | 34.6 |
| 12 Months postsurgery | 7.4 | 12.5 | 26.9 |
| Effective rate | |||
| 3 Months postsurgery | 70.4 | 75.0 | 65.4 |
| 12 Months postsurgery | 48.1 | 62.5 | 65.4 |
| Overall effective rate | |||
| 3 Months postsurgery | 85.2 | 95.8 | 100 |
| 12 Months postsurgery | 55.6 | 75.0 | 92.3* |
| Ineffective rate | |||
| 3 Months postsurgery | 14.8 | 4.1 | 0 |
| 12 Months postsurgery | 44.4 | 25.0 | 7.7 |
Table 3.
Changes in the ESS, QSQ, and snoring scale scores of the study participants
| Variable | Simple UPPP (n=27) | UPPP+GA (n=24) | UPPP+TBA (n=26) |
|---|---|---|---|
| ESS | |||
| Baseline | 9.0 (5–13) | 10.0 (5–14) | 9.5 (6–14) |
| 3 Months postsurgery | 6.5 (2–12)* | 6.0 (2–10)* | 7.0 (3–11)* |
| 12 Months postsurgery | 6.5 (3–11)* | 5.0 (3–7)* | 6.5 (2–11)* |
| QSQ | |||
| Baseline | 3.5 (2–6) | 4.5 (2–7) | 4.0 (2–6) |
| 3 Months postsurgery | 6.5 (5–7) | 7.0 (5–9) | 6.0 (5–7)* |
| 12 Months postsurgery | 6.0 (5–7) | 6.5 (2–10) | 6.5 (6–7)* |
| Snoring scale | |||
| Baseline | 7.5 (3–11) | 8.0 (3–12) | 8.5 (3–13) |
| 3 Months postsurgery | 5.0 (1–9)* | 5.0 (2–9)* | 5.0 (2–9)* |
| 12 Months postsurgery | 4.5 (1–8)* | 4.0 (2–6)* | 4.5 (1–8)* |
Table 4.
Changes in the AHI, SpO2, and CT90 of the study participants
| Variable | Simple UPPP (n=27) | UPPP+GA (n=24) | UPPP+TBA (n=26) |
|---|---|---|---|
| AHI | |||
| Baseline | 41.00±18.14 | 46.10±13.26 | 51.78±14.65 |
| 3 Months postsurgery | 24.12±11.25* | 23.56±6.32* | 24.95±7.84* |
| 12 Months postsurgery | 30.53±10.05* | 26.17±18.85* | 25.21±7.85* |
| SpO2 | |||
| Baseline | 68.19±7.74 | 69.39±13.41 | 67.63±9.11 |
| 3 Months postsurgery | 79.31±6.3* | 81.20±4.92* | 80.20±5.52* |
| 12 Months postsurgery | 82.25±5.11* | 82.60±4.32* | 79.70±5.99* |
| CT90 | |||
| Baseline | 26.11±6.48 | 24.30±4.87 | 25.20±5.92 |
| 3 Months postsurgery | 12.75±6.78* | 12.23±2.78* | 13.17±3.56* |
| 12 Months postsurgery | 13.06±7.8* | 12.46±3.65* | 13.57±2.78* |



