Abstract
Objectives
The silk patch is a thin transparent patch that is produced from silk fibroin. In this study, we investigated the treatment effects of the silk patch in patients with traumatic tympanic membrane perforation (TTMP).
Methods
The closure rate, otorrhea rate, and closure time in all patients and the closure time in successful patients were compared between the paper patch and silk patch groups.
Results
Demographic data (gender, site, age, traumatic duration, preoperative air-bone gap, and perforation size and location) were not significantly different between the two groups. The closure rate and otorrhea rate were not significantly different between the two groups. However, the closure time was different between the two groups (closure time of all patients, P=0.031; closure time of successful patients, P=0.037).
Conclusion
The silk patch which has transparent, elastic, adhesive, and hyper-keratinizing properties results in a more efficient closure time than the paper patch in the treatment of TTMP patients. We therefore believe that the silk patch should be recommended for the treatment of acute tympanic membrane perforation.
Traumatic tympanic membrane (TM) perforation is frequently seen in otorhinolaryngologic clinics. Its causes are the variable including penetration injury by cotton bud, barotrauma, concussion, and head trauma. TM perforation causes many symptoms such as hearing difficulty, sudden pain, tinnitus, ear discomfort and bleeding. Treatment of TM perforation includes regular observation, hyaluronic acid application, epidermal growth factor, TM patch, fat tissue application, gelfoam application, myringoplasty and tympanoplasty with temporalis fascia. Though, high rates of spontaneous recovery following conservative management of traumatic TM perforation (TTMP) are reported in many studies [1,2,3]. Spontaneous healing could not handle immediately perforation-related problems, such as tinnitus and chance to middle ear infection. Also, if insufficient healing occurs, surgery such as myringoplasty incurs relatively high costs, patient discomfort during perioperative periods, and surgery related morbidities. In these reasons, TM patch is commonly used primary treatment option in traumatic perforations.
Recent advances in tissue engineering and biomaterial research have suggested alternative material for TM regeneration [4]. Silk, collagen, chitosan, and calcium alginate have been studied as TM patching materials and have shown favorable results in animal models and clinical studies [4,5,6]. Among them, silk patch is reported that it has high biocompatibility and has a role to heal the perforated TM in animal study [7,8]. Even at previous animal study revealed that the silk patch showed better results than paper patch in an aspect of faster TM recovery [6,7,8].
Silk patch (Tympasil, Daewoong-Bio, Seoul, Korea) is a thin transparent patch that is produced from silk fibroin (Fig. 1). According to our limited knowledge, there is no report that used silk patch in patients with TTMP. In this study, we investigate the treatment effects of silk patch in patient with TTMP.
From 2011 to 2013, all 52 consecutive patients who managed in the Department of Otorhinolaryngology-Head and Neck surgery, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon, Korea, with diagnosis of TTMP was included in this retrospective study. The 52 patients were received one of two grafting materials: paper or silk.
The patients were excluded if there was granulation tissue or persistent otorrhea in the ear, severe vertigo or profound hearing loss, facial palsy, temporal bone fracture, or ossicular disruption suspected by physical examination or imaging study. Also, the patients who visited the hospital over 1 month after trauma were excluded.
Pure tone audiograms were obtained using an audiometer in a quiet room at the initial and 3 months after patching procedure. 0.5, 1, 2, and 4 khz was obtained for the pure tone average [9]. All patients were examined with an otomicroscope, and the size and site of perforation were documented. Perforation size was subdivided into four groups upon their sizes: small perforation (<25% of total TM), medium perforation (25% to 50%), large perforation (50% to 75%), total perforation (>75%) [10]. Perforation portion was subdivided into three groups: anterior perforation (anterior portion to malleus handle), posterior portion (posterior portion to malleus handle), central perforation (summation of anterior and posterior portion).
In all cases, patients were fully informed about the procedure and gave their informed consent after a discussion of the alternatives that include observing spontaneous closure or performing a formal myringoplasty.
All patients were received their procedures in the operation room. The procedure was performed by one senior author. Under the operation microscope, the external auditory canal was injected with 2% lidocaine and 1:100,000 epinephrine at bony cartilaginous junction. Sterilized paper patch (cigarette paper) or silk patch was manipulated into proper size. After marginal trimming and eversion of inverted part of perforated TM, the paper patch or silk patch was laid over the perforation of the TM using microforceps and ear pick. But some of cases (trauma history of short time within 24 hours) received patch procedures without trimming and eversion.
Before the procedures, paper patch was applied by antibiotics ointment and silk patch was immersed in normal saline for 3-4 minutes. Wetted silk patch was gradually changed to a yielding temper, so manipulation of silk patch was easier than hard conditioned that (Fig. 2A). After this procedure, we did not apply otic antibacterial drops and external auditory canal packing. Patients were discharged from hospital with instruction to avoid getting water in the ear and to avoid nose blowing. Patients took 3 days oral antibiotics as a prophylactic treatment.
After the patching procedure, outpatient department visits were carried out once a week until the perforation was completely healed, or up to 12 weeks. Perforations not healed within that periods were considered treatment failure. Patients were educated to visit the clinic if there was otorrhea from the treated ear. In cases of infection of the middle ear, systemic antibiotics and otic solution were prescribed. If the patch severely detached from original site on TM at outpatient department visits, repatching was considered. All patched were removed at least 1 week after the operation when TM had appeared fully recovered. Treatment success was defined as an intact TM under microscopic examination until 3 months follow-up. After 3 months, patients with treatment failure were recommended formal myringoplasty.
For statistical analysis of the results of the two groups, independent t-test was performed for continuous data, and Pearson chi-square test was used for categorical data. We used Pearson chi-square test to analyse gender, site, perforation size, perforation portion, otorrhea, and success rate. We used the independent t-test for comparisons between the two groups regarding preoperative air-bone gap, age, trauma duration and healing time. A probability of P<0.05 was taken to indicate statistical significance.
Fifty-two patients were enrolled into the study. Twenty-six patients were received paper patch procedures, the other 26 patients were received silk patch. Demographic data of this study (gender, site, age, traumatic duration, preoperative air-bone gap, perforation size and portion) were shown on Table 1. There was no significance difference between two group, paper patch and silk patch.
Success rate was identified as complete healing percentage of TM at follow-up period. In paper patch group, 19 patients succeeded at one stage procedure. Three patients taken repatch procedure and their TMs were healed completely. Four patients of paper patch group were failed (closure rate of paper patch group was 84.6%). In silk patch group, 23 patients succeeded at one stage procedure (Figs. 2, 3). One patient taken repatch procedure and TM was healed completely. Two patient of silk patch group was failed (closure rate of paper patch group was 92.3%). Their closure rate were slightly different, but there closure rates were not statistically different (P=0.385). According to perforation size or portion, there were no significant different between two groups (Table 2).
Otorrhea was observed in 2 patients in the paper patch group (7.7%) and 1 patient in the silk group (3.8%). All 3 patients were treated with removing infected patch, oral and topical antibiotics. Among infected 3 patients, 1 patient of paper patching group was failed, remain 2 patients healed completely at follow-up period (Table 2).
Closure time of all patients of paper patch group was 16.7±4.1 days, and silk group was 13.7±4.7 days. There was significant different between two group (P=0.031). After removing failed patients for analysis, closure time of success patients between two groups was different significantly (P=0.037) (Table 2).
Silk is a natural polymer produced by Bombyxmori silk worms. The silk consists primarily of two proteins, sericin and fibroin. Fibroin, the main component of silk proteins, has been studied to be an optimal substrate for the proliferation and adhesion of various cells. Silk fibroin has been shown various characteristics, such as high tensile strength, controllable biodegradability, hemostatic properties, noncytotoxicity, low antigenicity, and noninflammatory characteristics [11,12,13,14]. Levin et al. [5] reported its possibility in myringoplasty. Our group previously investigated the effects of a thin silk patch, in comparison with the paper patch in rat with large TM perforation. In that study, the mean healing times were significantly shorter in silk patch group than paper patch group [8]. We also evaluated silk patch may lead to reduced scar formation and may induce thin natural TM with minimal disturbance of sound conduction [8].
In this human study, we investigated that silk patching resulted in a reduced healing time compared with paper patching group. Success rates of two groups were almost same, but healing time was different (closure time of all patients, P=0.031; closure time of success patients, P=0.037) (Table 2). The incidence of reperforation and otorrea was not significantly different among the two groups (P=0.385 and P=0.552, respectively). The spontaneous closing rate of TTMP was 79%, and otorrea rate was 5% [8]. Compared with natural healing course of TTMP, closure rate of patch procedures were minimally increased. So we focused more rapid healing. Silk patches may function to regulate the healing pattern of the fibrous layer by preventing dehydration of the perforation margins and may facilitate re-growth of epithelium without deformation of the TM contours [8], healing process of TM was depended to their attaching materials. Furthermore, transparent property of silk patch gave more advantage to decide removing time of patch. This advantage reduced unnecessary procedure of checking remained perforation. The transparent patch enables the doctors to observe the extent of the healing process. At the office after procedure, if insufficient healing was suspected, the doctor could be delayed the removal of the patch to next visit.
Paper patch has the advantages such as easily gettable properties and economical merits. In form of cigarette paper, or other forms of thin papers could be used in perforation of TM. It can be applied in office settings without complex ear canal packing or incision. However, paper patching also has considerable points. First, the paper is occasionally displaced after procedure. The external auditory canal could be easily penetrated by water in normal life. Also the TM is well known for its movement reactive with noise and middle ear pressure. The thin nature of the paper might act as a disadvantage for displacement of a patch. The property of silk fibroin has adhering to surrounding tissue and elasticity for procedure, silk patch adhered to TM firmly during healing period without detaching portion. Second, there is possibility that paper may cause delayed healing and inflammation response. Shen et al. [6] reported that evident paper fragments embedded in the fibrous layer of the TM in some of their experimental animals with accompanying inflammatory infiltration. Kim et al. [8] first reported that silk patches are noninfectious, excellent healing rate and biocompatibility at the comparative study of the silk patch and paper patch in animal perforation model. But in our study, there was no difference between two groups in infection rate.
Silk patch generally showed better mechanical properties than paper patch. Mechanical properties such as elasticity and strength are thought to be important for the TM graft [15]. The Shape of the TM is funnel shape. Flat paper patch shows unfavorable for large perforation because TM is funnel shape. Silk is easily manageable due to their elasticity, so large perforation patching without detached portion is more suitable at silk patch.
Silk fibroin could support adhesion, proliferation, and differentiation of cells in vitro, including human TM keratinocytes [5,16,17]. Also other study, reported that hearing and healing benefits of silk fibroin membranes using onlay myringoplasty in rats [18]. In our study, we checked that whitish hyper-keratinized portion was shown. This property of silk fibroin might be facilitated TM healing process.
In conclusion, silk patch with transparent, elastic, adhesive and hyperkeratinizing property is more efficient than paper patch for the treatment of TTMP patients in aspect of healing time. Specially, silk patch is more suitable on large perforation because silk patch is more elasticity and easily manipulated. And we think that silk patch is one of recommendable material at TM perforation treatment. Limitations of this study include the small number of patients in both groups. Large number of patients with prospective design of study would be needed.
ACKNOWLEDGMENTS
This study was supported by a grant of the Korean Health Technology R&D Project (HI13C2268), Ministry of Health & Welfare, Republic of Korea.
References
1. da Lilly-Tariah OB, Somefun AO. Traumatic perforation of the tympanic membrane in University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria. Niger Postgrad Med J. 2007; 6. 14(2):121–124. PMID: 17599109.
2. Orji FT, Agu CC. Determinants of spontaneous healing in traumatic perforations of the tympanic membrane. Clin Otolaryngol. 2008; 10. 33(5):420–426. PMID: 18983374.

3. Kristensen S. Spontaneous healing of traumatic tympanic membrane perforations in man: a century of experience. J Laryngol Otol. 1992; 12. 106(12):1037–1050. PMID: 1487657.

4. Teh BM, Marano RJ, Shen Y, Friedland PL, Dilley RJ, Atlas MD. Tissue engineering of the tympanic membrane. Tissue Eng Part B Rev. 2013; 4. 19(2):116–132. PMID: 23031158.

5. Levin B, Rajkhowa R, Redmond SL, Atlas MD. Grafts in myringoplasty: utilizing a silk fibroin scaffold as a novel device. Expert Rev Med Devices. 2009; 11. 6(6):653–664. PMID: 19911876.

6. Shen Y, Redmond SL, Teh BM, Yan S, Wang Y, Atlas MD, et al. Tympanic membrane repair using silk fibroin and acellular collagen scaffolds. Laryngoscope. 2013; 8. 123(8):1976–1982. PMID: 23536496.

7. Lee OJ, Lee JM, Kim JH, Kim J, Kweon H, Jo YY, et al. Biodegradation behavior of silk fibroin membranes in repairing tympanic membrane perforations. J Biomed Mater Res A. 2012; 8. 100(8):2018–2026. PMID: 22581612.

8. Kim J, Kim CH, Park CH, Seo JN, Kweon H, Kang SW, et al. Comparison of methods for the repair of acute tympanic membrane perforations: Silk patch vs. paper patch. Wound Repair Regen. 2010; Jan-Feb. 18(1):132–138. PMID: 20082686.

9. Park MK, Kim KH, Lee JD, Lee BD. Repair of large traumatic tympanic membrane perforation with a Steri-Strips patch. Otolaryngol Head Neck Surg. 2011; 10. 145(4):581–585. PMID: 21593464.

10. Saliba I. Hyaluronic acid fat graft myringoplasty: how we do it. Clin Otolaryngol. 2008; 12. 33(6):610–614. PMID: 19126140.

11. Mori H, Tsukada M. New silk protein: modification of silk protein by gene engineering for production of biomaterials. J Biotechnol. 2000; 8. 74(2):95–103. PMID: 11763506.

12. Horan RL, Antle K, Collette AL, Wang Y, Huang J, Moreau JE, et al. In vitro degradation of silk fibroin. Biomaterials. 2005; 6. 26(17):3385–3393. PMID: 15621227.

13. Meinel L, Hofmann S, Karageorgiou V, Kirker-Head C, McCool J, Gronowicz G, et al. The inflammatory responses to silk films in vitro and in vivo. Biomaterials. 2005; 1. 26(2):147–155. PMID: 15207461.

14. Mauney JR, Nguyen T, Gillen K, Kirker-Head C, Gimble JM, Kaplan DL. Engineering adipose-like tissue in vitro and in vivo utilizing human bone marrow and adipose-derived mesenchymal stem cells with silk fibroin 3D scaffolds. Biomaterials. 2007; 12. 28(35):5280–5290. PMID: 17765303.

15. Kim JH, Choi SJ, Park JS, Lim KT, Choung PH, Kim SW, et al. Tympanic membrane regeneration using a water-soluble chitosan patch. Tissue Eng Part A. 2010; 1. 16(1):225–232. PMID: 19691425.

16. Altman GH, Diaz F, Jakuba C, Calabro T, Horan RL, Chen J, et al. Silk-based biomaterials. Biomaterials. 2003; 2. 24(3):401–416. PMID: 12423595.

17. Levin B, Redmond SL, Rajkhowa R, Eikelboom RH, Marano RJ, Atlas MD. Preliminary results of the application of a silk fibroin scaffold to otology. Otolaryngol Head Neck Surg. 2010; 3. 142(3 Suppl 1):S33–S35. PMID: 20176279.

18. Shen Y, Redmond SL, Teh BM, Yan S, Wang Y, Zhou L, et al. Scaffolds for tympanic membrane regeneration in rats. Tissue Eng Part A. 2013; 3. 19(5-6):657–668. PMID: 23092139.

Fig. 1
(A) Scanning electron microscope image with nonporous structure. (B) Thin transparent silk patch.
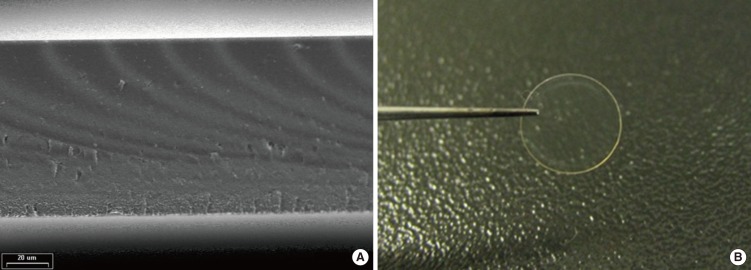
Fig. 2
Silk patch (black arrow) applied the group of small sized tympanic membrane (TM) perforation. (A) The pack of silk patch was opened and silk patch was immersed in normal saline for about 3 to 4 minutes to get the flexibility. (B) Right TM findings of silk patch applied 48 years old patient. He had the silk patch apply at 7 days after trauma. The complete perforation healing status of TM shows at postoperation 2 weeks. (C) Pure tone audiometry shows nonvisible air-bone gap at postoperation 2 weeks. Pre-Op, preoperation; Post-Op, postoperation.
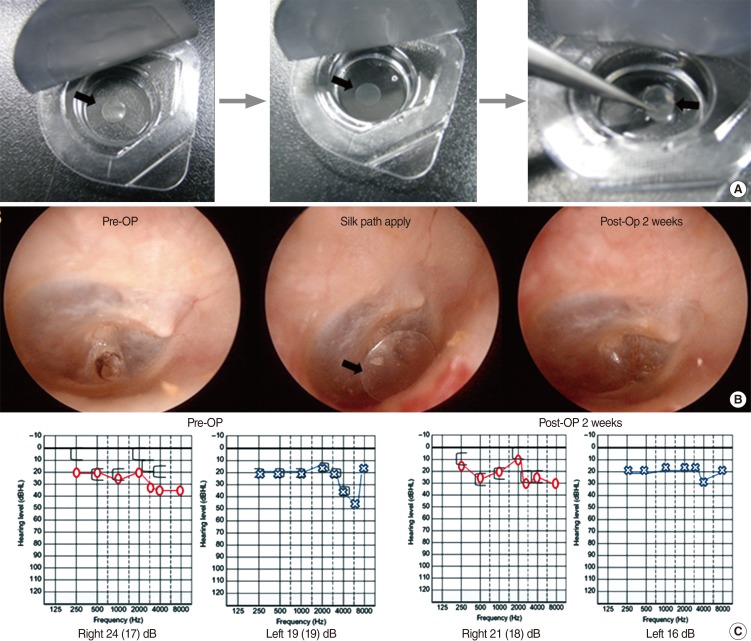
Fig. 3
Silk patch (black arrow) applied the group of medium sized tympanic membrane (TM) perforation. (A) Left TM findings of silk patch applied 62 years old patient. He had the silk patch apply at 2 weeks after trauma. TM findings show the complete perforation healing status of TM at postoperation 2 weeks. (B) Pure tone audiometry shows the improved air-bone gap at postoperation 1 month. Pre-Op, preoperation; Post-Op, postoperation.
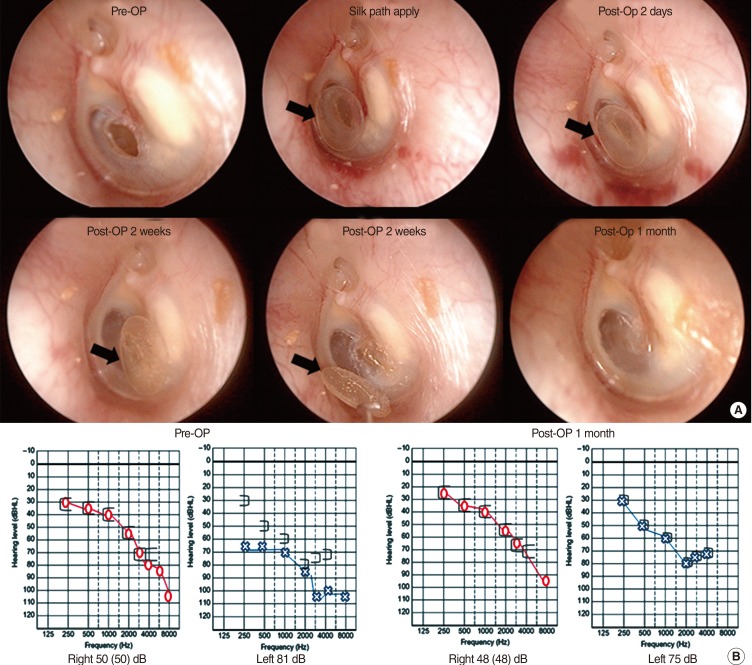
Table 1.
Demographic data of patients in the paper patch group and silk patch group
Table 2.
Outcomes of paper patch group and silk patch group
| Variable | Paper patch | Silk patch | P-value |
|---|---|---|---|
| Closure rate (%) | 84.6 | 92.3 | 0.385 |
| Failed patients as perforation size (small:medium:large:total) | 1:1:0:2 | 0:1:1:0 | 0.290 |
| Failed patients as perforation portion (anterior:posterior:central) | 0:2:2 | 1:0:1 | 0.223 |
| Otorrhea (%) | 7.7 | 3.8 | 0.552 |
| Closure time of all patients (day), mean±SD | 16.7±4.1 | 13.7±4.7 | 0.031* |
| Closure time of success patients (day), mean±SD | 16.9±4.2 | 14.0±4.6 | 0.037* |




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download