Abstract
Relapsing polychondritis (RP) is an uncommon systemic disease that is characterized by episodic and progressive inflammation of the cartilaginous structures, which can be very debilitating and in some instances life-threatening. The pathogenic pathways of RP are largely unknown. However, several hypothesis have been suggested. We had an interesting case of aggravation of RP due to the infection. Graft cartilage on the nasal tip was affected by RP also. This case can give a clue of revealing the pathogenesis of RP. We introduce a case with a review of the literature.
Relapsing polychondritis (RP) is an uncommon systemic disease that is characterized by episodic and progressive inflammation of the cartilaginous structures, including the elastic cartilage of the ear and nose, the hyaline cartilage of the peripheral joints, the fibrocartilage at axial sites and the cartilage of the tracheobronchial tree, which can be very debilitating and in some instances life-threatening [1]. The pathogenesis of RP is still unclear, but it is believed to involve an immunologic mechanism as evidenced by the presence of auto-antibodies against native collagens (II, IX, and XI), a cell mediated immune response toward cartilage components and collagen II immunization induced chondritis and arthritis in animal models [2]. The purpose of this article is to describe a case of aggravation of RP due to an infection and inflammation and to provide a review of the literature. We also speculate about the pathognomic factors and pathogenesis of RP.
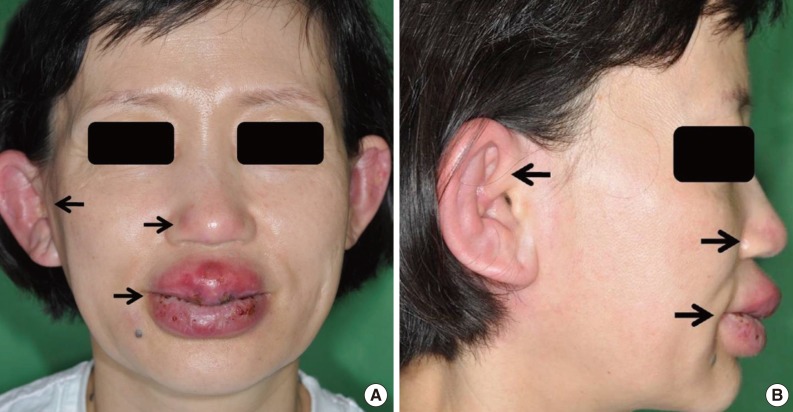
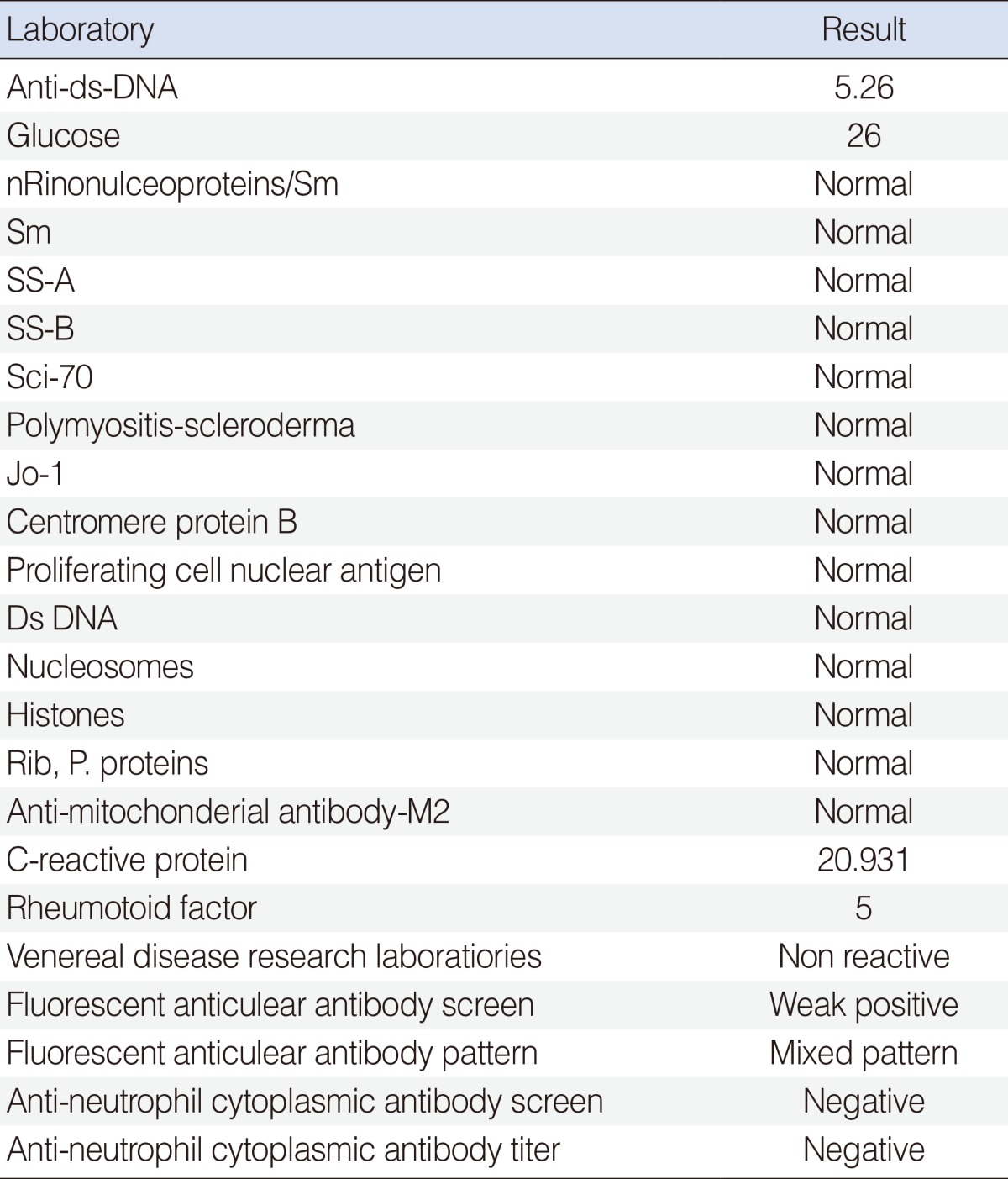
A 48-year-old woman initially presented in September 2009 with complaints of painful swelling and erythematous changes in the upper and lower lips, both ear auricles and the nasal tip for the previous three days (Fig. 1). She had undergone a filler injection procedure for cosmetic reasons on the both lips at an illegal cosmetic hair shop (not by a medical doctor) seven days previously. The cause of lip infection may be the filler materials which may be not sterilized and not qualified on Korea Food and Drug Administration. There were no other symptoms like fever, chills, arthralgias, dyspnea or voice changes and no specific lab findings (Table 1). She had a medical history of relapsing polychondritis and a surgical history of undergoing a surgical operation that was performed by a plastic surgeon for the tip of her nose. The nose-tip surgery had been done by using the right conchal cartilage for augmentation. After she underwent the operation, the nasal tip turned red whenever polychondritis symptoms-color changes of both ear auricles and arthralgia-developed. This case shows that grafted cartilage can also be affected like other cartilages. The symptoms improved a few days after she received methotraxate (2.5 mg, twice a day) and methylpredisolone (8 mg, twice a day) (Fig. 2). We used the medication for seven days. Four weeks after discharge, the swelling and erythematous changes of the nasal tip and the other cartilage resolved.
The pathogenic pathways of RP are largely unknown. However, an immunologic role has been suggested. The presence of auto-antibodies against native collagens and the response to steroid and immunosuppressant drugs like methotrexate are evidence of the immunologic characteristic of RP. Patient with RP have demonstrated both autoantibodies and cellular immune reactions to type II collagen [3]. Alexandros A. Drosos et al. reported that the titers against native type II collagen were substantially higher than the titers against the constituent alpha-1 (II) chains [4]. This observation suggests that the antibodies were not formed after destruction of cartilage and denaturation of collagen. Therefore, the formation of antibodies to type II collagen may be a primary event in the pathogenesis of RP and not a consequence of inflammation. However, Stabler et al. [5] studied the serum cytokine profiles in RP. In that study, the levels of proinflammatory chemokine like monocyte chemoattractant protein 1, macrophage inflammatory protein 1b, and interleukin-8 were elevated in RP. This data suggests a major role for a cell-mediated immune response in the pathophysiology of RP. In our case, the basis of relationship between RP and filler injection is the RP symptoms onset time. After she underwent filler procedure, inflammation on her lips occurred and immediately after her RP symptoms occurred too. We think inflammation on lips is the trigger factor of RP. Finally, as lips inflammation was improved, RP symptoms were improved too. Another factors (another infection, inflammation, and immune factor) which can give rise to RP symptoms were not found at that time. Judging by our case, an inflammation resulting from infection can be one of the factors to trigger the immune cascade in RP. Therefore, we can support that a cell-mediated immune response can play a major role in RP. Although there are many hypotheses about the pathogenesis of RP, further study about the beginning, perpetuation and activation of the immune system is needed.
With regard to the pathogenesis, in our case, it is interesting that the grafted auricular cartilage also may have been affected by autoantibodies [6]. This may be the first case of grafted cartilage being affected by RP. Antibodies to type II collagen as well as to type IX and XI collagen are found in the sera of patients with RP. Therefore, autoantibodies in the sera of RP patients can affect grafted cartilage, wherever the location of the cartilage is. However, in this case, we can also speculate about some part of the pathogenesis. If the grafted cartilage is not the patient's, then what could have happened? There were still autoantibodies in the patient's sera and homologous grafted cartilage also have type II collagen as well as type IX and XI. We think that that the grafted homologous cartilage, and not autologous cartilage, may have also been affected by autoantibodies because these antibodies targeted against the native or denatured type II collagen and proteoglycans, which are quite common in cartilage and denatured structures. This case could be helpful to speculate the pathogenesis of RP.
In conclusions, relapsing polychondritis is rare disease and its pathogenesis is not clear. However, inflammation due to the infection can trigger the cascade of RP, and it can provide some evidence to reveal the secret.
References
1. Yamaoka K, Saito K, Hanami K, Nakayamada S, Nawata M, Iwata S, et al. A case of life-threatening refractory polychondritis successfully treated with combined intensive immunosuppressive therapy with methotrexate. Mod Rheumatol. 2007; 17(2):144–147. PMID: 17437170.

2. McAdam LP, O'Hanlan MA, Bluestone R, Pearson CM. Relapsing polychondritis: prospective study of 23 patients and a review of the literature. Medicine (Baltimore). 1976; 5. 55(3):193–215. PMID: 775252.
3. Dolan DL, Lemmon GB Jr, Teitelbaum SL. Relapsing polychondritis: analytical literature review and studies on pathogenesis. Am J Med. 1966; 8. 41(2):285–299. PMID: 4223687.
4. Sokka T, Toloza S, Cutolo M, Kautiainen H, Makinen H, Gogus F, et al. Women, men, and rheumatoid arthritis: analyses of disease activity, disease characteristics, and treatments in the QUEST-RA study. Arthritis Res Ther. 2009; 11(1):R7. PMID: 19144159.
5. Stabler T, Piette JC, Chevalier X, Marini-Portugal A, Kraus VB. Serum cytokine profiles in relapsing polychondritis suggest monocyte/macrophage activation. Arthritis Rheum. 2004; 11. 50(11):3663–3667. PMID: 15529362.

6. Foidart JM, Abe S, Martin GR, Zizic TM, Barnett EV, Lawley TJ, et al. Antibodies to type II collagen in relapsing polychondritis. N Engl J Med. 1978; 11. 299(22):1203–1207. PMID: 714080.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download