Abstract
Petrous apicitis is a rare but fatal complication of otitis media. An infection within the middle ear can extend within the temporal bone into the air cells of the petrous apex. With only the thin dura mater separating the trigeminal ganglion and the 6th cranial nerve from the bony petrous apex, they are vulnerable to inflammatory processes, resulting in deep facial pain, lateral rectus muscle paralysis, and diplopia. In 1904, Gradenigo described a triad of symptoms related to petrous apicitis, including acute suppurative otitis media, deep facial pain resulting from trigeminal involvement, and abducens nerve palsy. It has traditionally been treated with surgery, but recent advances in imaging, with improved antibiotic treatment, allow conservative management. In this case report, we describe a clinical and neuroradiological evolution of a child with a petrous apicitis after acute otitis media, which was managed medically with a positive outcome.
Petrous apicitis is an extension of infection from the mastoid air cell tract into a pneumatized anterior or posterior petrous apex. The petrous apex may be pneumatic, marrow filled, or sclerotic, and it has been estimated that 30% of posterior petrous apices are pneumatized [1,2]. Prior to the introduction of widely available antibiotics, apical petrositis was a frequently fatal complication of otitis media. Unrecognized and under-treated petrositis can lead to clinically important complications including meningitis, extradural and intracranial abscesses, cranial nerve palsies, venous sinus thrombosis, subdural empyema, labyrinthitis and death [3]. With only the thin dura mater separating the trigeminal ganglion and the sixth cranial nerve from the bony petrous apex, they are vulnerable to inflammatory processes in that region, resulting in deep facial pain, lateral rectus paralysis, and diplopia [4].
In 1904, Gradenigo described the triad of retroorbital pain, the sixth cranial nerve paralysis, and otorrhea, since known as Gradenigo syndrome. Only a few patients with petrous apicitis exhibited the full triad these days [1,2]. A short review of English literature showed only 13 cases of complete Gradenigo syndrome in children during otitis media since 1980 [5]. In Korea, only 4 cases of petrositis with abducens nerve palsy were reported. Three cases were successfully treated surgically, an 8-year-old boy with both petrous apicitis and ipsilateral abducens nerve palsy [6], 29-year-old male with petrositis and the abducens palsy [7], and a patient with full triad of symptoms of Gradenigo syndrome [8]. One case showed improvement without surgery, an 8-year-old female with cavernous sinus thrombophlebitis and abducence nerve palsy secondary to petrositis, who had complete resolution of her symptoms after antibiotics, steroids and ventilation tube insertion [9]. We presented a case of petrositis after acute otitis media (AOM) with both abducence nerve palsies, which was managed medically without any steroid or surgical intervention.
A 8-year-old girl was admitted to our pediatric department with a 3-week history of headache and diplopia. She had visited a local clinic due to otorrhea of left side and taken medication under the diagnosis of left AOM. After a few days, otorrhea disappeared but headache and diplopia were worsened. Her past medical history was significant only for left convergent strabismus. At admission, physical examination showed restricted lateral gaze of both eyeballs and diplopia at central gaze, secondary to clearly apparent both abducens nerve palsies (Fig. 1A). Facial motor examination was normal. The left tympanic membrane was amber and right tympanic membrane was intact. There was no fever, although she claimed that she had high fever up to 38.9℃ before she took medication at the local clinic. Her headache was located at left temporal area at the initial stage but migrated to frontal and then to whole head. The ophthalmologic examination showed bilateral optic disc swelling (Fig. 2A). Laboratory tests showed a white blood cell count of 6, 290 mm3 with 67% neutrophils, and the C-reactive protein was 0.3 mg/L, and erythrocyte sedimentation rate (ESR) 6 mm/hour. Under the impression of meningitis at the pediatric department she took brain magnetic resonance imaging (MRI), spinal tapping, temporal bone computed tomography (CT), and bone scan. Her brain MRI showed a diffuse inflammatory process in the left mastoid air cells with invasion of the left petrous bone (Fig. 3). Temporal bone CT showed soft tissue densities at left mastoid, middle ear, and well-developed petrous apex cells (Fig. 4A). The cerebrospinal fluid examination was normal, and bone scan showed increased uptake of the left mastoid and petrous bones. Diagnosis of left petrositis and bilateral abducens nerve palsies was made, and intravenous antibiotic treatment with ceftriaxone (1 g/day), clindamycin (300 mg/day) was initiated. After 9 days of intravenous antibiotics, consultation and transfer to otolaryngology department was done due to continuous headache and diplopia. Pure tone audiometry was done and showed air-bone gap of 10 dB on left ear. On physical examination, restricted lateral gaze on both sides due to abducens nerve palsies of both side was noted. Left tympanic membrane was amber and ventillation tube insertion was performed and serous profuse discharge in the middle ear was sent for culture. No bacteria was identified. Intravenous antibiotics (ceftriaxone, clindamycin) were continuously administered and topical ear drops were applied. On the 16th hospital day, diplopia was improved and the field of diplopic vision was shortened from 10 cm to 2 cm length (Fig. 1B), but intermittent spiking fever up to 38.3℃ occurred, and intravenous amikacin was added. On the 19th hospital day, the fever continued and follow-up temporal bone CT with contrast enhance, H1N1 PCR for H1N1 flu which was common at the time, general laboratory studies and pediatric consultation was done. On temporal bone CT with contrast enhancement, remaining soft tissue densities at mastoid and petrous area with improving petrositis was noted (Fig. 4B). And with negative H1N1 PCR and high AST/ALT of 617/365 IU/L, under the diagnosis of drug fever, she was transfered to the pediatric department, on the 21th hospital day when diplopia disappeared. Antibiotic was changed to intravenous vancomycin, and fever subsided with AST/ALT of 40/78 IU/L on the 30th hospital day. The strabismus returned to preadmission state, and the patient was finally discharged (Fig. 1C). After two weeks at the out-patient department, follow-up temporal bone CT was taken and disappearance of opacification and improved aeration at left petrous apex area were noted (Fig. 4C). There was also improvement of bilateral papilledema six weeks later of admission (Fig. 2B).
Petrositis is a rare complication of otitis media. In Minottis's research of 100 children admitted to Children's Hospital of Pittsburgh between 1980 and 1995 with an intratemporal complication of AOM, four patients presented with acute petrositis [10]. Patients exhibiting the full triad of Gradenigo syndrome, retroorbital pain, the sixth cranial nerve paralysis, and otorrhea, are very rare. A review of the English literature for Gradenigo syndrome or petrous apicitis revealed only 48 publications concerning this entity, most in the otolaryngology literature [4]. In Korea, only 4 case reports of petrositis with abducens nerve palsy have been found on recent reviews of the Korean-language literatures.
Most cases of petrous apicitis are considered to occur in patients with well-developed air cell systems extending into the petrous apex [1,2]. The time interval between the onset of the otitis and the manifestation of cranial nerve dysfunction varies between one week and two to three months. This is not surprising, since the petrous apex is the summit of the pyramid-shaped os petrosum, of which the middle ear and the mastoid form the base. The inflammatory process spreads from the base to the top of the pyramid, extending along the strings of pneumatized cells from the mastoid towards the petrous apex [11]. In addition to the triad symptoms of Gradenigo syndrome, petrous apicitis may have variable presentations. Other symptoms include ipsilateral facial paralysis due to involvement of the 7th cranial nerve, deficits of cranial nerves VIII, IX, and X, vertigo, and sensorineural hearing loss as a result of labyrinthine involvement of the inner ear [4].
Unilateral sixth nerve palsy does not always reveal a Gradenigo syndrome. A patient, who had three recurrent episodes of unilateral sixth nerve palsy that occurred after a viral upper respiratory tract infection, has been described [12]. Each time, the patient was managed conservatively and had complete return of the sixth cranial nerve function within two weeks [12].
No reported case of bilateral abducens nerve palsies after AOM has been found, but bilateral abducens nerve palsies occurring after meningitis, sphenositis, etc. were not unfrequent [13,14]. In our case, radiologic test revealed no abnormality in contralateral petrous apex. But the fact that the cavernous sinus also encases contralateral abducens nerve, optic nerve etc., microscopic spread of infection can be considered resulting in contralateral abducens nerve palsy.
Most authors advocate for surgery, due to the possibility of fatal complications. Chole and Donald [15], stated that aggressive surgical drainage is indicated when the diagnosis of petrous apicitis is made, and Watkyn-Thomas [16] reported that petrositis is curable by adequate mastoid operation. Hendershot et al. [17] presented middle fossa approach for the the treatment of petrous apicitis. But recent reports advocate conservative therapy with high-dose broad-spectrum antibiotics and less aggressive surgical procedures [4], and actually five cases among 48 reviewed English literatures were treated without surgery. Marianowski et al. [5] insisted on the possibility of a conservative management of Gradenigo syndrome in children, when diagnosis is performed before intracranial complications, and reported a case of a 6-year-old boy with Gradenigo syndrome managed medically with a positive outcome. The patient had been treated at first by oral antibiotics (amoxicillin at a dose of 50 mg/kg per day) for a right otitis media, but right diplopia occurred and intravenous antibiotics were started. He received ceftriaxone (50 mg/kg per day), metronidazole (40 mg/kg per day) for 33 days and amikacin (5 mg/kg per day) for 3 days, plus acetyl salycilic acid and an intravenous corticotherapy (methylprednisolone). Discharge medication was oral amoxicillin (100 mg/kg per day) and clavulanate, and complete recovery of the abducens palsy was noted [5]. Minotti and Kountakis [18] reported a case of petrositis with abducens nerve palsy managed successfully without surgical intervention, a 47-year-old woman successfully treated with intravenous antibiotics and tympanostomy tube placement. And Finkelstein et al. [19] also reported a 12-year-old boy with Gradenigo syndrome successfully treated with intravenous antibiotics and tube placement. The patient was given intravenous ceftriaxone (2 g/day) and vancomycin (600 mg/3 per day) for 3 weeks, metronidazole (400 mg/3 per day) for 1 week, and intravenous dexamethasone (10 mg/day) for 2 days, and 2 weeks of oral amoxicillin (40 mg/kg per day) and clavulanic acid (10 mg/kg per day) for discharge medication. Burston et al. [3] reported 2 cases of Gradenigo syndrome successfully treated with conservative treatment. One case was treated with 4 weeks of intravenous metronidazole, 6 weeks of intravenous ceftriaxone, and oral ciprofloxacin, followed by 6 weeks of ciprofloxacin and clindamycin. The other case used intravenous ceftriaxone, amoxicillin-clavulanic acid and metronidazole for 6 weeks, and oral amoxicillin-clavulanic acid and metronidazole for further 6 weeks [3]. In 4 reported cases of Korean-language literature, 3 cases were treated surgically, and only one case was cured with conservative treatment. A 8-year-old girl with abducens nerve palsy secondary to petrositis recoverd completetly with ventilation tube insertion, intravenous cefotaxime, ampicillin and oral steoid (prednisolone, 1 mg/kg/day) [9].
We would like to insist on the possibility of a conservative management of petrositis. Our case showed a good example of conservative treatment; adequate diagnosis by using imaging studies, and close observation with antibiotics and drainage through ventilation tube, before occurrence of intracranial complications. Especially in children with pneumatized petrous bones, prompt treatment of otitis media would be helpful before occurrence of these complications. However, when the conservative therapy fails or chronic ear disease is present, surgical intervention is indicated to ensure adequate drainage of the mastoid and petrous bone.
References
1. Chole RA, Sudhoff HH. Chronic otitis media, mastoiditis, and petrositis. In : Flint PW, Haughey BH, Lund VJ, Niparko JK, Richardson MA, Robbins KT, editors. Cummings otolaryngology head and neck surgery. 5th ed. Philadelphia, PA: Mosby;c2010. p. 1963–1978.
2. El-Kashlan HK, Harker LA, Shelton C, Aygun N, Niparko JK. Complications of temporal bone infections. In : Flint PW, Haughey BH, Lund VJ, Niparko JK, Richardson MA, Robbins KT, editors. Cummings otolaryngology head and neck surgery. 5th ed. Philadelphia, PA: Mosby;c2010. p. 1979–1998.
3. Burston BJ, Pretorius PM, Ramsden JD. Gradenigo's syndrome: successful conservative treatment in adult and paediatric patients. J Laryngol Otol. 2005; 4. 119(4):325–329. PMID: 15949093.

4. Lutter SA, Kerschner JE, Chusid MJ. Gradenigo syndrome: a rare but serious complication of otitis media. Pediatr Emerg Care. 2005; 6. 21(6):384–386. PMID: 15942518.
5. Marianowski R, Rocton S, Ait-Amer JL, Morisseau-Durand MP, Manach Y. Conservative management of Gradenigo syndrome in a child. Int J Pediatr Otorhinolaryngol. 2001; 1. 57(1):79–83. PMID: 11165646.

6. Lee NH, Ban JH, Park CY, Kim CC. A case of petrositis with abducens palsy. Korean J Otolaryngol-Head Neck Surg. 2006; 8. 49(8):869–872.
7. Shin HS, Yoo HK, Suh YR. A case of unusual petrositis. Korean J Otolaryngol-Head Neck Surg. 1964; 6. 7(2):59–62.
8. Lee KC, Chio C, Park KY, Park MS. A case of Gradenigo's syndrome combining epidural abscess and Bezold's abscess. Korean J Otolaryngol-Head Neck Surg. 1989; 6. 32(3):567–571.
9. Park SN, Yeo SW, Rhyoo JY, Lee HY. A case of cavernous sinus thrombophlebitis and abducence nerve palsy secondary to petrositis. Korean J Otolaryngol-Head Neck Surg. 2002; 1. 45(1):82–85.
10. Goldstein NA, Casselbrant ML, Bluestone CD, Kurs-Lasky M. Intratemporal complications of acute otitis media in infants and children. Otolaryngol Head Neck Surg. 1998; 11. 119(5):444–454. PMID: 9807067.

11. Gillanders DA. Gradenigo's syndrome revisited. J Otolaryngol. 1983; 6. 12(3):169–174. PMID: 6876244.
12. Sternberg I, Ronen S, Arnon N. Recurrent, isolated, post-febrile abducens nerve palsy. J Pediatr Ophthalmol Strabismus. 1980; Sep-Oct. 17(5):323–324. PMID: 7441445.

13. Laurens MB, Becker RM, Johnson JK, Wolf JS, Kotloff KL. MRSA with progression from otitis media and sphenoid sinusitis to clival osteomyelitis, pachymeningitis and abducens nerve palsy in an immunocompetent 10-year-old patient. Int J Pediatr Otorhinolaryngol. 2008; 7. 72(7):945–951. PMID: 18472169.

14. Peters GB 3rd, Bakri SJ, Krohel GB. Cause and prognosis of nontraumatic sixth nerve palsies in young adults. Ophthalmology. 2002; 10. 109(10):1925–1928. PMID: 12359616.

15. Chole RA, Donald PJ. Petrous apicitis: clinical considerations. Ann Otol Rhinol Laryngol. 1983; Nov-Dec. 92(6 Pt 1):544–551. PMID: 6660745.
16. Watkyn-Thomas FW. The treatment of petrositis: (section of otology). Proc R Soc Med. 1936; 1. 29(3):267–274. PMID: 19990585.
17. Hendershot EL, Wood JW, Bennhoff D. The middle cranial fossa approach to the petrous apex. Laryngoscope. 1976; 5. 86(5):658–663. PMID: 933655.

18. Minotti AM, Kountakis SE. Management of abducens palsy in patients with petrositis. Ann Otol Rhinol Laryngol. 1999; 9. 108(9):897–902. PMID: 10527283.

19. Finkelstein Y, Marcus N, Mosseri R, Bar-Sever Z, Garty BZ. Streptococcus acidominimus infection in a child causing Gradenigo syndrome. Int J Pediatr Otorhinolaryngol. 2003; 7. 67(7):815–817. PMID: 12791460.

Fig. 1
Photography of the eyes at initial (A), the 16th hospital day (B), and the 30th hospital day (C). The patient had left strabismus at central gaze, and inability of full lateral gaze of both eyes suggesting both abducens nerve palsy at initial (A). Improvement of left strabismus at central gaze accompanying central diplopia and much improvement of lateral gaze of both eyes were shown at the16th hospital day (B). Improvement of left strabismus at central gaze without central diplopia, and further improvement of lateral gaze of both eyes were shown at the 30th hospital day (day of discharge).
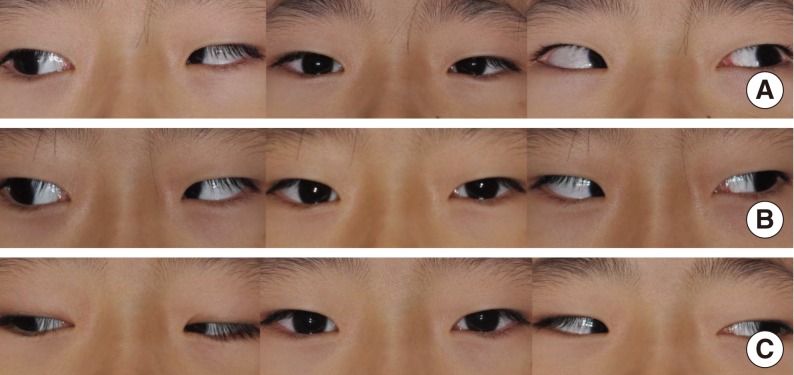
Fig. 2
Fundoscopic examinations at admission (A), and at six weeks after admission (B). There was severe swelling of bilateral optic discs at admission day (A), and much improvement of blurring of the optic disc margins after six weeks (B).
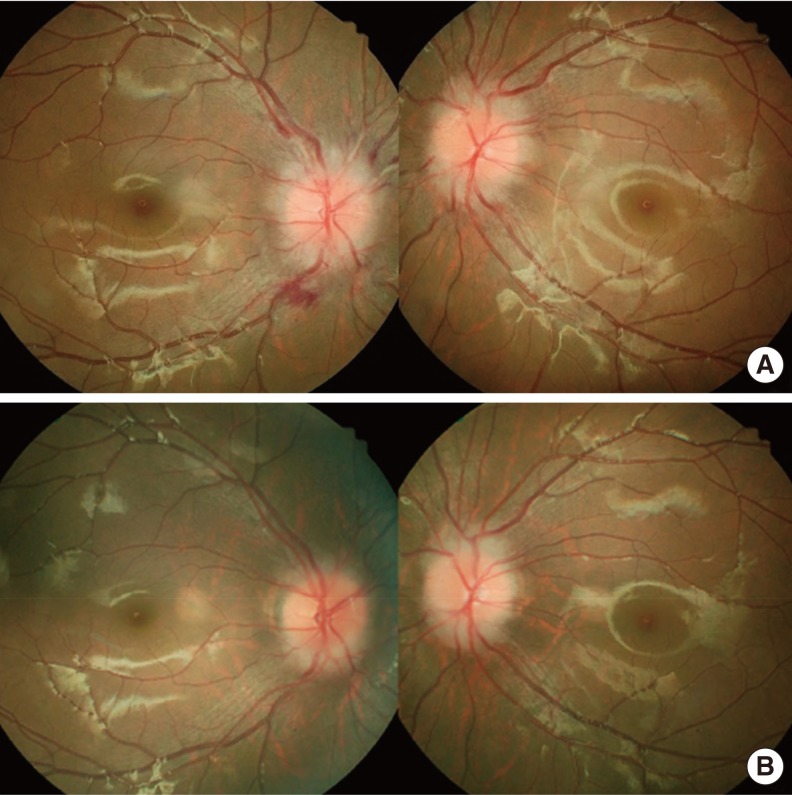
Fig. 3
Brain magnetic resonance imaging (MRI) findings at admission: T2 weighted MRI finding (A) and T1 weighted enhanced MRI finding (B). These showed high signal intensities involving left mastoid and petrous apex (arrows).
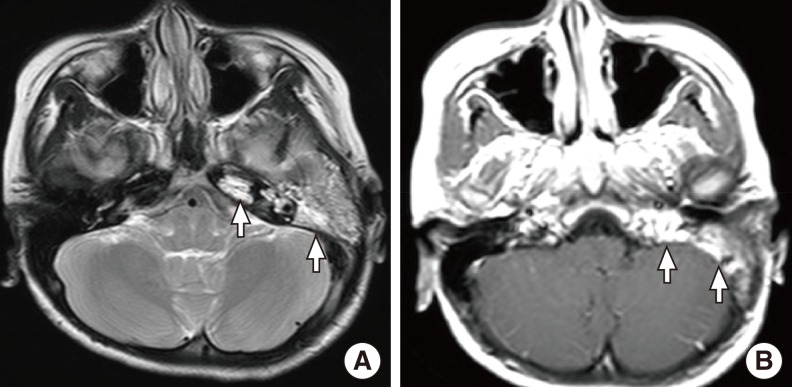
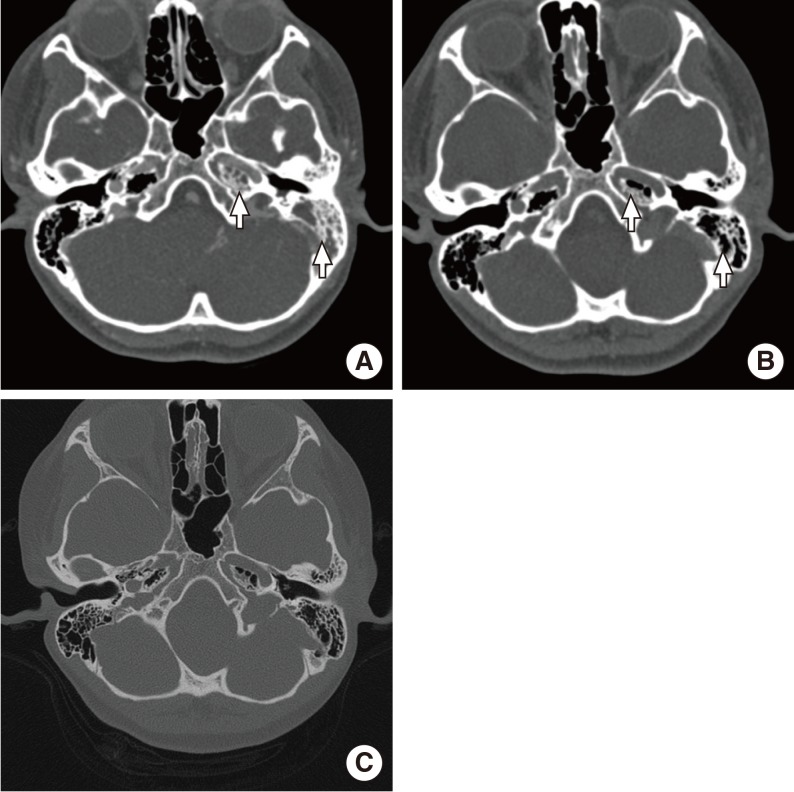
Fig. 4
Temporal bone computed tomography (CT) with contrast enhancement at the 9th hospital day, showing extended pneumatization of left temporal bone to petrous apex and soft tissue densities at left mastoid and petrous apex (A). At the 21th hospital day, improved aeration of left petrous apex and mastoid with some residual soft tissue densities are shown (B). Temporal bone CT at two weeks after discharge date, showing further improvement of aeration of left petrous apex and mastoid with ventilation tube in situ (C).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download