1. Mognetti B, Di Carlo F, Berta GN. Animal models in oral cancer research. Oral Oncol. 2006; 5. 42(5):448–460. PMID:
16266822.

2. Salley JJ. Experimental carcinogenesis in the cheek pouch of the Syrian hamster. J Dent Res. 1954; 4. 33(2):253–262. PMID:
13152263.

3. Chen YK, Lin LM. DMBA-induced hamster buccal pouch carcinoma and VX2-induced rabbit cancer as a model for human oral carcinogenesis. Expert Rev Anticancer Ther. 2010; 9. 10(9):1485–1496. PMID:
20836683.

4. Kim S. Animal models of cancer in the head and neck region. Clin Exp Otorhinolaryngol. 2009; 6. 2(2):55–60. PMID:
19565028.

5. Morris AL. Factors influencing experimental carcinogensis in the hamster cheek pouch. J Dent Res. 1961; Jan-Feb. 40(1):3–15. PMID:
13772812.
6. Heber EM, Monti Hughes A, Pozzi EC, Itoiz ME, Aromando RF, Molinari AJ, et al. Development of a model of tissue with potentially malignant disorders (PMD) in the hamster cheek pouch to explore the long-term potential therapeutic and/or toxic effects of different therapeutic modalities. Arch Oral Biol. 2010; 1. 55(1):46–51. PMID:
19945092.

7. Odukoya O, Shklar G. Initiation and promotion in experimental oral carcinogenesis. Oral Surg Oral Med Oral Pathol. 1984; 9. 58(3):315–320. PMID:
6435048.

8. Odukoya O, Shklar G. Two-phase carcinogenesis in hamster buccal pouch. Oral Surg Oral Med Oral Pathol. 1982; 11. 54(5):547–552. PMID:
6817251.

9. Fasanaro TS. Bleaching teeth: history, chemicals, and methods used for common tooth discolorations. J Esthet Dent. 1992; May-Jun. 4(3):71–78. PMID:
1389350.

10. Pohanish RP, Sittig M. Sittig's handbook of toxic and hazardous chemicals and carcinogens. 6th ed. Amsterdam: Elsevier;2012.
11. Naik S, Tredwin CJ, Scully C. Hydrogen peroxide tooth-whitening (bleaching): review of safety in relation to possible carcinogenesis. Oral Oncol. 2006; 8. 42(7):668–674. PMID:
16488181.

12. Hirota N, Yokoyama T. Enhancing effect of hydrogen peroxide upon duodenal and upper jejunal carcinogenesis in rats. Gann. 1981; 10. 72(5):811–812. PMID:
7327382.
13. Ito A, Watanabe H, Naito M, Naito Y. Induction of duodenal tumors in mice by oral administration of hydrogen peroxide. Gann. 1981; 2. 72(1):174–175. PMID:
7274643.
14. Weitzman SA, Weitberg AB, Stossel TP, Schwartz J, Shklar G. Effects of hydrogen peroxide on oral carcinogenesis in hamsters. J Periodontol. 1986; 11. 57(11):685–688. PMID:
3104570.

15. Institute of Laboratory Animal Resources (US), Committee on Care and Use of Laboratory Animals. Guide for the care and use of laboratory animals. Bethesda, MD: US Department of Health and Human Services, Public Health Service;1996.
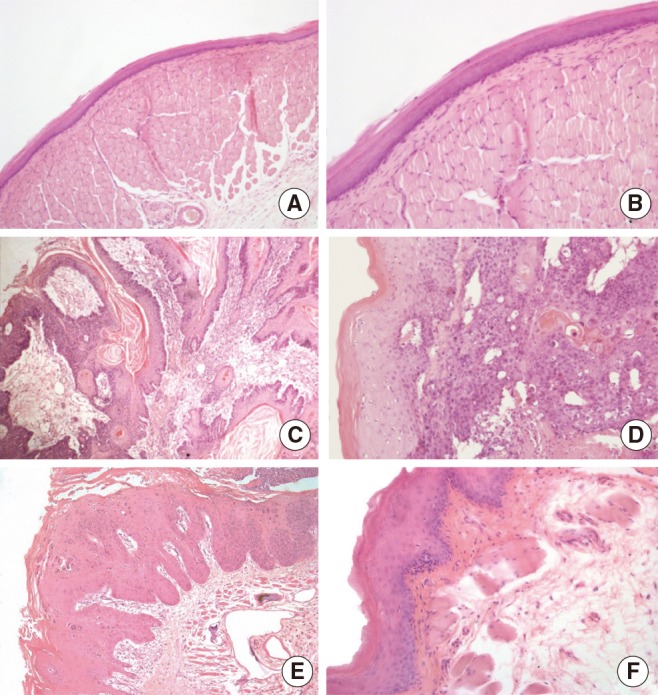
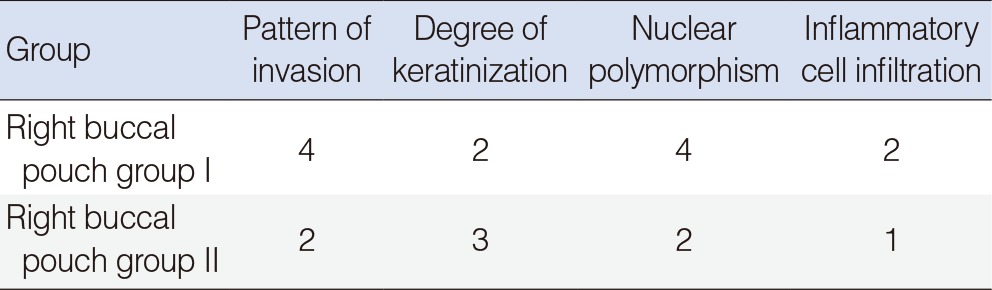
16. Bryne M. Is the invasive front of an oral carcinoma the most important area for prognostication? Oral Dis. 1998; 6. 4(2):70–77. PMID:
9680893.

17. Anneroth G, Batsakis JG, Luna M. Malignancy grading of squamous cell carcinoma in the floor of the mouth related to clinical evaluation. Scand J Dent Res. 1986; 8. 94(4):347–356. PMID:
3462898.

18. Lametschwandtner A, Lametschwandtner U, Weiger T. Scanning electron microscopy of vascular corrosion casts--technique and applications: updated review. Scanning Microsc. 1990; 12. 4(4):889–940. PMID:
2094009.
19. Konerding MA. Scanning electron microscopy of corrosion casting in medicine. Scanning Microsc. 1991; 9. 5(3):851–865. PMID:
1725561.
20. Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009; Apr-May. 45(4-5):309–316. PMID:
18804401.

21. Ow TJ, Myers JN. Current management of advanced resectable oral cavity squamous cell carcinoma. Clin Exp Otorhinolaryngol. 2011; 3. 4(1):1–10. PMID:
21461056.

22. Vairaktaris E, Spyridonidou S, Papakosta V, Vylliotis A, Lazaris A, Perrea D, et al. The hamster model of sequential oral oncogenesis. Oral Oncol. 2008; 4. 44(4):315–324. PMID:
18061531.

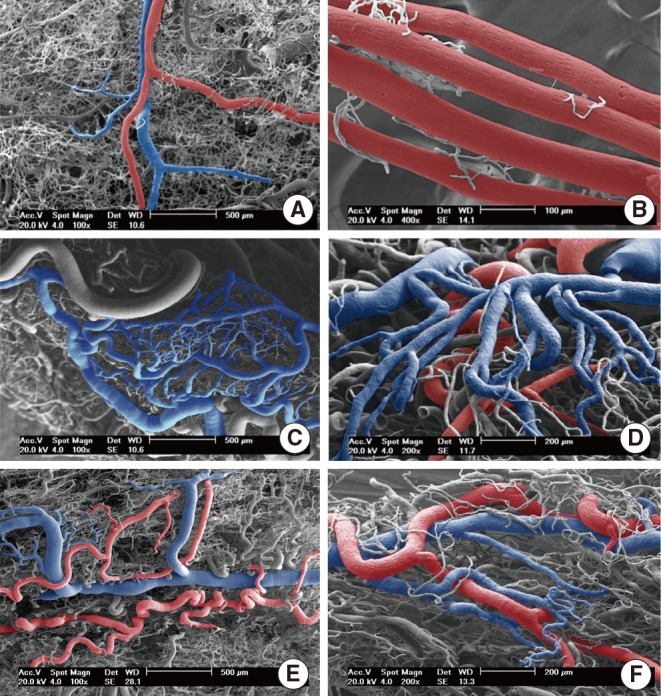
23. Sullivan SM, Pittman RN. Hamster retractor muscle: a new preparation for intravital microscopy. Microvasc Res. 1982; 5. 23(3):329–335. PMID:
7099023.

24. Molinari AJ, Aromando RF, Itoiz ME, Garabalino MA, Monti Hughes A, Heber EM, et al. Blood vessel normalization in the hamster oral cancer model for experimental cancer therapy studies. Anticancer Res. 2012; 7. 32(7):2703–2709. PMID:
22753729.
25. Collet AM, Palmieri M, Molinari B, Schwint AE, Itoiz ME. Experimental study to test the potential tumor promotion effect of a tooth bleaching agent. Acta Odontol Latinoam. 2001; 14(1-2):30–34. PMID:
15208934.
26. Lin LM, Chen YK, Lai DL, Huang YL. Minimal arecaidine concentrations showing a promotion effect during DMBA-induced hamster cheek pouch carcinogenesis. J Oral Pathol Med. 1996; 2. 25(2):65–68. PMID:
8667258.

27. Wani MK, Yarber RH, Ahmed A, Hengesteg A, Robbins KT. Cancer induction in the DMBA hamster cheek pouch: a modified technique using a promoter. Laryngoscope. 2001; 2. 111(2):204–206. PMID:
11210861.

28. Silvan S, Manoharan S. Apigenin prevents deregulation in the expression pattern of cell-proliferative, apoptotic, inflammatory and angiogenic markers during 7,12-dimethylbenz[a]anthracene-induced hamster buccal pouch carcinogenesis. Arch Oral Biol. 2013; 1. 58(1):94–101. PMID:
22776109.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download