Abstract
Objectives
Facial nerve schwannomas may be misdiagnosed as vestibular schwannomas (VSs) if the tumor is confined to the internal auditory canal (IAC) without involvement the geniculated ganglion or labyrinthine segment of facial nerve. Because facial nerve schwannomas may be misdiagnosed as VSs, we investigated the differences between the two.
Methods
The study included 187 patients with a preoperative diagnosis of VS. Of these, six were diagnosed with facial nerve schwannomas during surgery. We reviewed the preoperative evaluations and surgical findings of facial nerve schwannomas mimicking VSs.
Results
No useful preoperative predictors are available for facial nerve schwannomas mimicking VSs. Facial nerve schwannomas are usually confined to the IAC. After opening the dura of the IAC, a facial nerve schwannoma can be diagnosed after identifying a normal-appearing nerve located lateral to the tumor. When this was the case, we performed facial nerve preservation surgery or decompression.
Facial nerve schwannomas are typically multi-segmental and most often involve the geniculate or tympanic segment [1,2]. However, facial nerve schwannomas involving the internal auditory canal (IAC) or cerebellopontine angle (CPA) without extension to the labyrinthine segment or beyond have been reported [3,4].
It is important to identify a facial nerve schwannoma with preserved facial nerve function because surgical removal of the tumor can lead to facial nerve injury and permanent facial palsy. However, no useful preoperative evaluation tools are available for determining the nerve origin of a schwannoma when the tumor is confined to the IAC or CPA [5,6]. Therefore, we investigated the differences between facial nerve and vestibular schwannomas (VSs).
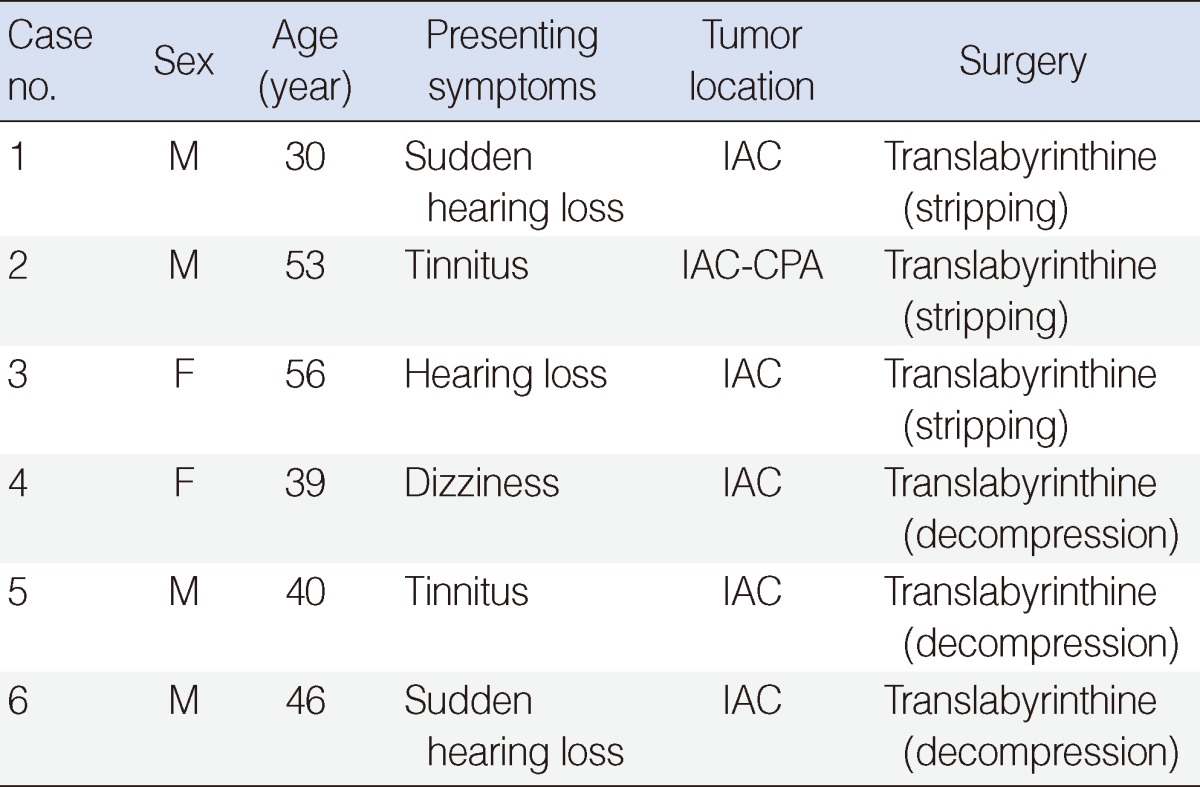
We retrospectively reviewed the charts of 187 patients who were preoperatively diagnosed with VS at Soonchunhyang University Hospital and Severance Hospital between January 2000 and December 2011. We excluded cases with preoperative facial palsy. Of the 187 patients, six were diagnosed with facial nerve schwannoma during surgery. We called this 'facial nerve schwannoma mimicking vestibular schwannoma' (FNSMVS). We reviewed the preoperative and surgical findings of FNSMVS.
All six patients with FNSMVS had cochleovestibuar symptoms without facial palsy (Table 1). There was no involvement of geniculate ganglion or labyrinthine segment of facial nerve in all cases. Three patients presented with hearing loss on the lesion side; of these, two presented with sudden hearing loss. Of the remaining three patients, two complained of tinnitus and one case presented with dizziness. Five cases of FNSMVS were confined to the IAC and one was a small tumor. There was no specific finding to find the nerve of origin of the tumor in magnetic resonance imaging (MRI). We performed facial nerve preservation stripping surgery or decompression after making the correct diagnosis.
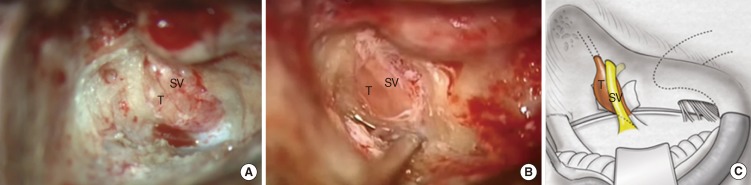
For a VS, the tumor mass can only be seen after the dura of the IAC is opened using a translabyrinthine approach (Fig. 1). The facial nerve is identified in the fundus area proximal to the tumor. For a FNSMVS, a normal-appearing nerve lateral to the tumor mass can be seen after opening the IAC (Fig. 2). The normal-appearing nerve runs from fundus to porus laterally. By continuing to drill along the tumor at the fundus, we can confirm the origin of the tumor. The tumor is connected with labyrinthine segment of facial nerve. The normal-appearing nerve starting at the fundus is the superior vestibular nerve.
With the increasingly widespread use of MRI, retrocochlear tumor lesions are being detected more frequently. Schwannomas of IAC or CPA arise mainly from the vestibular nerve, while the facial nerve is rarely involved. Several studies have reported facial nerve schwannomas that were initially diagnosed as VS [3,4,6]. However, no useful tools are available for the preoperative determination of the nerve origin of a schwannoma, when the tumor is confined to the IAC or CPA. As in our study population, most facial nerve schwannomas in the IAC or CPA are diagnosed during surgery.
A facial nerve schwannoma in the IAC and CPA usually manifests as perceptive hearing impairment and tinnitus because the tumor compresses the cochlear nerve [7,8]. Sherman et al. [9] reported that a facial nerve schwannoma limited to the CPA/IAC presents with a higher rate of hearing loss and a much lower rate of facial palsy. In our study population, most patients had cochlear symptoms without facial palsy.
Large CPA tumors with preoperative facial palsy are likely to be considered facial nerve schwannoma. Although approximately 30% of facial nerve schwannomas present with no facial palsy, large facial nerve schwannomas extending to the posterior cranial fossa quite often present with facial palsy [10]. None of our patients had a large tumor and it is likely that large facial nerve schwannomas usually present with facial palsy.
Although there were attempts to identify a small lesion arising eccentrically from the anterior superior location of the facial nerve in either the CPA or IAC using sagittal oblique reconstructions of the three-dimensional MRI, the distinction between VS and FNS of the CPA or IAC alone cannot be made reliably on imaging so far [2]. We also could not differentiate the FNSMVS on MRI findings in our cases.
When a facial nerve schwannoma is identified unexpectedly during surgery for a presumed VS, the surgeon is faced with a dilemma regarding how to proceed. The patient may not have been informed of, or given appropriate consent for, issues associated with tumor removal. A biopsy is generally contraindicated unless malignancy is suspected [11]. There have been several reports of tumor excision in which the nerve is left intact and functioning [12,13]. In some cases without facial dysfunction, we were able to dissect the tumor from the facial nerve because the neural compression was minimal. Angeli and Brackmann [14] reported that wide decompression is an alternative to surgical removal in cases of unsuspected facial neuromas in patients with normal facial nerve function. In other cases, we chose to use decompression because the exposed tumor could not be dissected from the facial nerve.
Although preoperative differentiation between FNSMVS and VS is impossible, early detection during surgery is very important to avoid inadvertent damage. The surgeon can also establish a treatment plan for an unexpected facial nerve schwannoma during surgery. When the anatomic relationship of the vestibular nerves to the facial nerve is considered, the facial nerve is typically deflected medially by the tumor. Therefore, the facial nerve is identified as both proximal and distal to the tumor, for smaller tumors. When a normal-appearing nerve appears lateral to the tumor, one might question the diagnosis of FNSMVS. The tumor diagnosis can be confirmed by dissecting the facial nerve both proximal and distal to the tumor.
FNSMVS can be differentiated from VS by identifying specific surgical findings after opening the dura of the IAC. Surgeons should familiarize themselves with these surgical finding and suspect FNSMVS when they encounter one during surgery. It is also desirable to inform the patient about the possibility of a facial nerve schwannoma when diagnosing a VS.
ACKNOWLEDGMENTS
The authors wish to thank Dong-Soo Jang for the medical illustration. This study was supported by the Soonchunhyang University Research Fund.
References
1. Lipkin AF, Coker NJ, Jenkins HA, Alford BR. Intracranial and intratemporal facial neuroma. Otolaryngol Head Neck Surg. 1987; 1. 96(1):71–79. PMID: 3118299.

2. Thompson AL, Aviv RI, Chen JM, Nedzelski JM, Yuen HW, Fox AJ, et al. Magnetic resonance imaging of facial nerve schwannoma. Laryngoscope. 2009; 12. 119(12):2428–2436. PMID: 19780031.

3. King TT, Morrison AW. Primary facial nerve tumors within the skull. J Neurosurg. 1990; 1. 72(1):1–8. PMID: 2294168.

5. Park HY, Kim SH, Son EJ, Lee HK, Lee WS. Intracanalicular facial nerve schwannoma. Otol Neurotol. 2007; 4. 28(3):376–380. PMID: 17414044.

6. Kania RE, Herman P, Tran Ba. Vestibular-like facial nerve schwannoma. Auris Nasus Larynx. 2004; 9. 31(3):212–219. PMID: 15364354.

7. McMenomey SO, Glasscock ME 3rd, Minor LB, Jackson CG, Strasnick B. Facial nerve neuromas presenting as acoustic tumors. Am J Otol. 1994; 5. 15(3):307–312. PMID: 8579133.
8. O'Donoghue GM, Brackmann DE, House JW, Jackler RK. Neuromas of the facial nerve. Am J Otol. 1989; 1. 10(1):49–54. PMID: 2719087.
9. Sherman JD, Dagnew E, Pensak ML, van Loveren HR, Tew JM Jr. Facial nerve neuromas: report of 10 cases and review of the literature. Neurosurgery. 2002; 3. 50(3):450–456. PMID: 11841711.

10. Kubota Y, Kawamata T, Kubo O, Kasuya H, Muragaki Y, Hori T. Large facial nerve schwannomas without facial palsy: case reports and review of the literature. Neurosurg Rev. 2005; 7. 28(3):234–238. PMID: 15754210.

11. McMonagle B, Al-Sanosi A, Croxson G, Fagan P. Facial schwannoma: results of a large case series and review. J Laryngol Otol. 2008; 11. 122(11):1139–1150. PMID: 18177538.

12. Nadeau DP, Sataloff RT. Fascicle preservation surgery for facial nerve neuromas involving the posterior cranial fossa. Otol Neurotol. 2003; 3. 24(2):317–325. PMID: 12621351.

13. Lee JD, Kim SH, Song MH, Lee HK, Lee WS. Management of facial nerve schwannoma in patients with favorable facial function. Laryngoscope. 2007; 6. 117(6):1063–1068. PMID: 17464236.

14. Angeli SI, Brackmann DE. Is surgical excision of facial nerve schwannomas always indicated? Otolaryngol Head Neck Surg. 1997; 12. 117(6):S144–S147. PMID: 9419130.

Fig. 1
Surgical finding of vestibular schwannoma (VS). (A) The VS is seen only as a tumor mass after opening the dura of the internal auditory canal (IAC). (B) Schematic drawing of a VS after opening the dura of the IAC. T, tumor; FN, facial nerve.
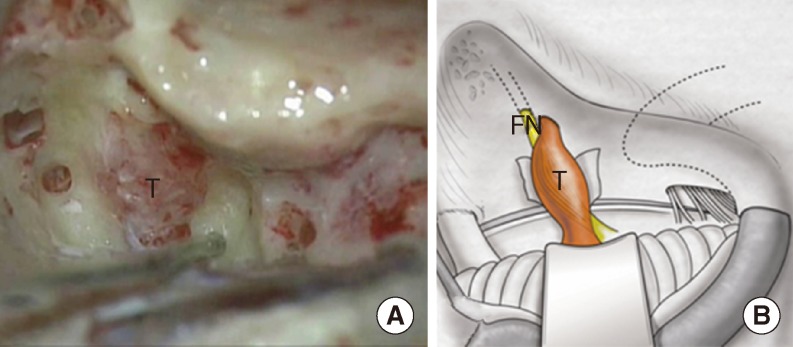
Fig. 2
Surgical finding of facial nerve schwannoma mimicking a vestibular schwannoma (VS). (A, B) Facial nerve schwannoma has a normal-appearing nerve lateral to the tumor mass in each case. (C) Schematic drawing of a facial nerve schwannoma mimicking a VS after opening the dura of the internal auditory canal. T, tumor; SV, superior vestibular nerve.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download