This article has been
cited by other articles in ScienceCentral.
Abstract
The authors report a 64-year-old man who developed persistent direction fixed nystagmus after a canalith repositioning maneuver for horizontal canal benign paroxysmal positional vertigo (HC-BPPV). The patient was initially diagnosed with right HC-BPPV given that the Dix-Hallpike test showed geotropic horizontal nystagmus that was more pronounced on the right side, although the roll test did not show any positional nystagmus. The patient was treated with a canalith repositioning maneuver (Lempert maneuver). The next day, the patient experienced a different character of dizziness, and left-beating spontaneous nystagmus regardless of head position was observed. After a forced prolonged left decubitus and frequent head shaking, his symptoms and nystagmus resolved. This condition, referred to as canalith jam, can be a complication after the repositioning maneuver in patients with BPPV. Atypical positional tests suggest that abnormal canal anatomy could be the underlying cause of canalith jam.
Go to :

Keywords: Canalith jam, Benign paroxysmal positional vertigo, Repositioning maneuver
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is one of the most common disorders that cause dizziness. BPPV is characterized by brief recurrent episodes of vertigo triggered by changes in head position. The duration, frequency, and symptom intensity of BPPV vary depending on the involved canals and the location of otolithic debris [
1].
It has been proposed that the pathogenesis of BPPV is related to free-floating particulate matter in the endolymph of the semicircular canals [
2]. Three types of BPPV variants were described-canalolithiasis, cupulolithiasis, and canalith jam.
Canalith jam refers to a condition caused by a blockage of free-floating particles within a canal, which blocks the flow of endolymph or the movement of a cupula [
3]. Canalith jam is caused by plugging of the horizontal canal's narrow point, which either occurs during a canalith repositioning maneuver or develops spontaneously and can cause persistent nystagmus regardless of head position [
4].
We report a patient who presented with BPPV of the right horizontal semicircular canal and subsequently developed persistent left-beating horizontal nystagmus unaffected by head position following a canalith repositioning maneuver, probably due to jamming of the horizontal canal.
Go to :

CASE REPORT
A 64-year-old man presented with recurrent attacks of vertigo, one of which was provoked by head movement one day prior to presentation. The patient had a history of left vestibular neuritis 2 years prior. A caloric test was performed at that time, and the results showed a 64% left vestibular function deficit. There were no abnormal findings on the brain magnetic resonance imaging (MRI).
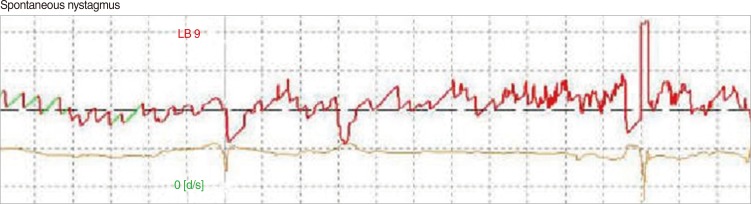
A caloric test was performed on the current presentation, and the results showed a 53% left vestibular function deficit. A physical examination was also performed, and spontaneous nystagmus was not observed with the patient in the sitting position. A Dix-Hallpike test revealed bilateral geotropic horizontal nystagmus, in which the nystagmus was direction-changing nystagmus depending on the head position and was more pronounced on the right. Subjective dizziness was also more severe on the right. However, a head roll test did not induce any nystagmus on either side (
Fig. 1). A diagnosis of right horizontal canal BPPV (HC-BPPV) was made, and the patient was treated with the Lempert maneuver.
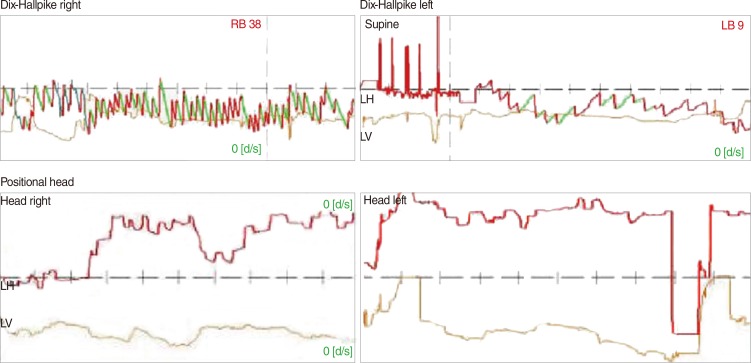 | Fig. 1Result of Dix-Hallpike test performed on initial visit. It showed bilateral horizontal geotropic nystagmus on the Dix-Hallpike test. The Dix-Hallpike test provoked horizontal nystagmus that was more pronounced on the right (38 deg/second) than on the left (9 deg/second). However, in positional roll test, there was no nystagmus recorded. RB, right beating; LB, left beating; LH, left horizontal; LV, left vertical. 
|
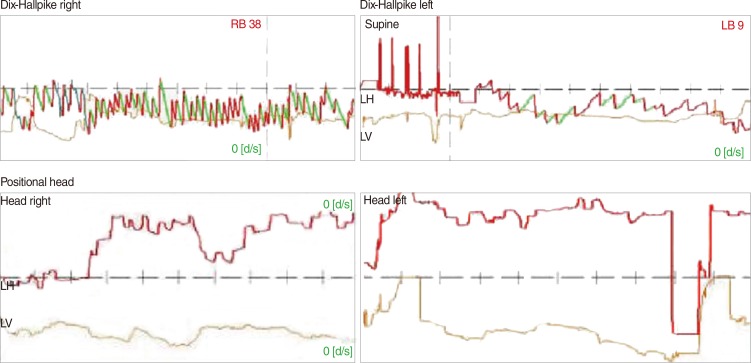
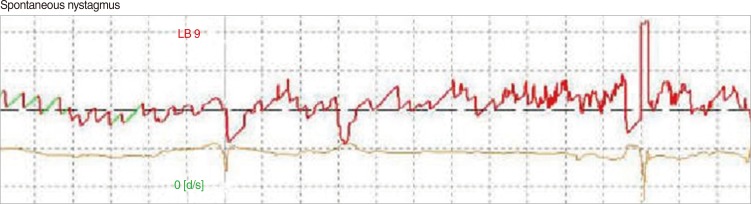
The next day, the patient still complained of dizziness, but the character of the dizziness was different. On video nystagmography, left-beating horizontal spontaneous nystagmus was observed with the patient in the sitting position (
Fig. 2). The Dix-Hallpike test and the head roll test showed persistent left-beating nystagmus in either side (
Fig. 3). Based on these findings, we diagnosed a canalith jam in the right horizontal semicircular canal that developed after the canalith repositioning maneuver in the setting of HC-BPPV. We instructed the patient to perform frequent head shaking and had him maintain a left decubitus position. After one day, the nystagmus was not observed on portable video nystagmography in any position and subjective dizziness was completely disappeared.
 | Fig. 2Spontaneous nystagmus recorded on the day after the repositioning maneuver. It showed left-beating spontaneous nystagmus (9 deg/second). LB, left beating. 
|
 | Fig. 3Result of the Dix-Hallpike and positional test the day after the repositioning maneuver. It shows left-beating nystagmus independent of head position during the Dix-Hallpike test and positional test. The velocity of the nystagmus was greater after the Dix-Hallpike test than after the positional test. LB, left beating; LH, left horizontal; LV, left vertical; RH, right horizontal; RV, right vertical. 
|
Go to :

DISCUSSION
In this case report, the patient was initially diagnosed with right HC-BPPV because of direction-changing geotropic horizontal nystagmus based on the positioning test. However, the day after a canalith repositioning maneuver, the patient developed persistent vertigo with spontaneous horizontal nystagmus to the left regardless of head position. This direction-fixed persistent nystagmus resolved after treatment with head shaking and a prolonged left decubitus position. We consider this case of canalith jam a rare complication after a canalith repositioning maneuver.
Canalith jam was first described by Epley [
3]; in this condition, freely moving otoconial particles block the endolymphatic flow. This results in negative pressure between the cupula and the jamming point and transiently reduces the vestibuloocular reflex. This causes persistent direction-fixed nystagmus towards the opposite side.
The cause of canalith jam is not yet clear. Theoretically, there are two possibilities: innate semicircular canal stenosis and/or a plug caused by otoconial debris. Accordingly, the innate stenosis of the canal could induce an otoconial debris jam in the narrow portion, although a giant otoconial plug could occur in a normal canal. Horii et al. [
5] recently suggested that patients with intractable BPPV had more abnormal appearing canals compared with normal controls based on 3-dimensional reconstruction of inner ear MR images.
There are few case reports on canalith jams. von Brevern et al. [
6] described continuous vertigo with spontaneous nystagmus following a canalith repositioning maneuver for HC-BPPV. Our case is very similar. However, in our case, the results of the provoking maneuver in HC-BPPV is quite different from cases of typical HC-BPPV. The patient did not show any nystagmus on a head roll test or any spontaneous nystagmus in the sitting position. Geotropic horizontal nystagmus was not induced by the head roll test but was induced by the Dix-Hallpike test.
Generally, the Dix-Hallpike test is not more sensitive than the head roll test in patients with horizontal canalolithiasis. However, in the current case, the Dix-Hallpike test was more sensitive than the head roll test in diagnosing HC-BPPV. White et al. [
7] revealed that the Dix-Hallpike test provides stimulation of the lateral semicircular canal when changing from a sitting position to a supine position. Any tests that induce stimulation of the horizontal semicircular canal can lead to direction-changing horizontal nystagmus. In this case, free floating particles were lodged in the shorter canal rather than in the normal semicircular canal due to a portion of the canal being stenotic. For this reason, the Dix-Hallpike test when performed with a faster head motion induced more apparent nystagmus than the head roll test. Thus, the horizontal nystagmus without a torsional portion induced bilaterally by the Dix-Hallpike test should be considered canalolithiasis of the horizontal semicircular canal.
Treatment of the otoconial debris jam involves procedures designed to dislodge the particles back in the direction from which the debris originated. This can be accomplished using gravity and with vibration applied to the mastoid. Simultaneously, a forced prolonged position in which patients feel more comfortable can improve the symptoms. In the current case, the patient was treated successfully with frequent head shaking and forced prolonged left decubitus. The day after the treatment, spontaneous nystagmus completely resolved based on video nystagmography.
In conclusion, canalith jam is a possible complication following the canalith repositioning maneuver. Geotropic horizontal nystagmus changed into direction-fixed spontaneous nystagmus after the canalith repositioning maneuver. In addition, in this patient, geotropic horizontal nystagmus was induced by the Dix-Hallpike maneuver rather than the head roll test. This means that the geometric structure of the horizontal canal might be abnormal in this patient.
Go to :






 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download