Abstract
Objectives
The purpose of study was to report the current role of transnasal esophagoscopy (TNE) in Korea.
Methods
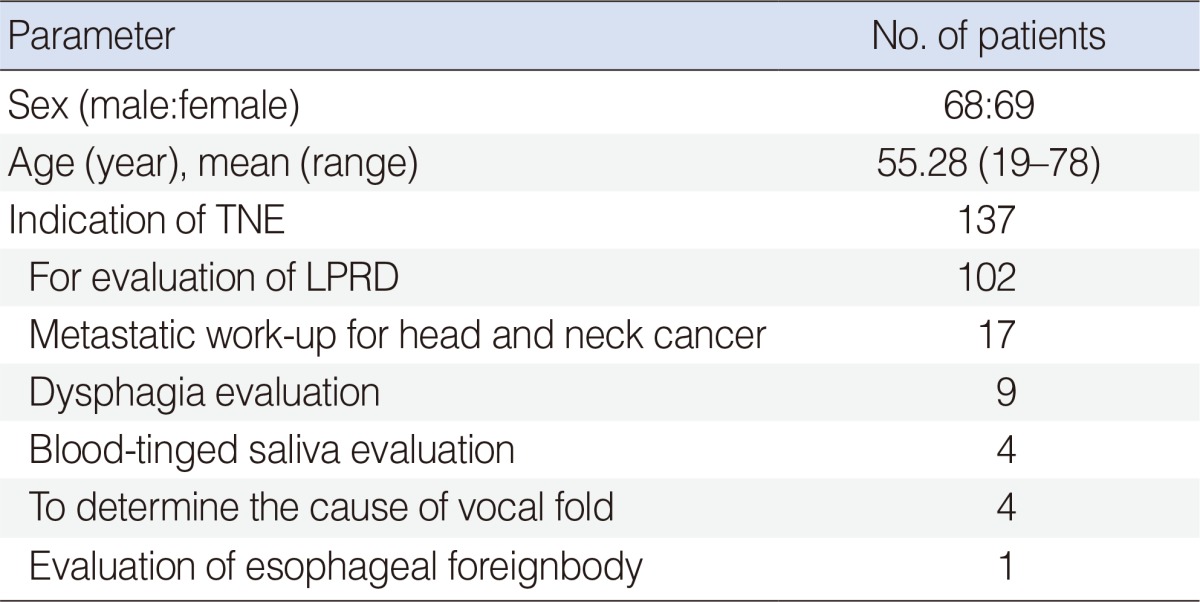
One hundred thirty-seven patients who underwent TNE at Soonchunhyang University Bucheon Hospital (n=69) and Korea University Anam Hospital (n=68) from July 2007 to February 2009 were prospectively analyzed. Laryngopharyngeal reflux disease (LPRD) patients without any response to proton-pump inhibitor (n=102), and patients with complaints that require esophagoscopy as part of their evaluation (n=35) were included in this study; investigation of metachronous lesions or routine follow-up screening of head and neck cancer patients, n=17; dysphagia, n=9; blood tinged saliva, n=4; to determine the cause of vocal fold paralysis as screening tool, n=4; suspicious esophageal foreign body, n=1.
Results
Fifty-three patients (38.7%) had positive findings on TNE. Positive finding ratio was highest in group of dysphagia (7 among 9 patients, 78%). Forty-two patients (41.1%) were found to have pathology (esophagitis, n=41; esophageal diverticulum, n=1) during the screening examination for LPRD. There were no significant complications in any of the patients.
Go to : 
A substantial percentage of patients present to the laryngologist with complaints that require esophagoscopy as part of their evaluation. Until recently, to evaluate esophagus below the level of the pyriform sinus, gastroenterologist become involved so that the patient could undergo flexible esophagoscopy performed with the use of intravenous sedation. However, head and neck surgeon is familiar with transnasal fiberscopic laryngoscope and anatomy of the esophagus. Also, the small caliber flexible endoscopes with excellent image quality now allow unsedated, transnasal esophagoscopy (TNE) in the office setting. This offers the patient the advantage of a complete upper aerodigestive tract evaluation in a short period of time, with immediate review of the results. The purpose of study was to report the current role of TNE in Korea.
Go to : 
One-hundred thirty seven patients who underwent TNE at Soonchunhyang University Bucheon Hospital (n=69) and Korea University Anam Hospital (n=68) from July 2007 to Feb 2009 were prospectively analyzed in this study. The study group was composed of 68 men and 69 women (mean age, 55.28 years; range 19 to 78 years). Laryngopharyngeal reflux disease (LPRD) patients without any response to proton-pump inhibitor (PPI) (n=102), and patients with complaints that require esophagoscopy as part of their evaluation (n=35) were included in this study; investigation of metachronous lesions or routine follow-up screening of head and neck cancer patients, n=17; dysphagia, n=9; blood tinged saliva, n=4; to determine the cause of vocal fold paralysis as screening tool, n=4; suspicious esophageal foreign body, n=1 (Table 1). We excluded the patients who had esophagogastrofiberscopy for last one year. To assess patient's subjective discomfort, a visual analogue scale (VAS) was used for patient's satisfaction (0, worst; 5, fair; 10, best), and pain score during esophagoscopy (0, no; 1, mild; 2, moderate; 3, most severe pain). This study was reviewed and approved by the ethics committee of two institutions. All participants were given detailed explanation of the study from researchers, and provided written informed consent relevant to this investigation.
Participants of LPRD were interviewed in search of symptoms relevant to LPRD. A common self-administered questionnaire, the Reflux Symptom Index (RSI) developed by Belafsky et al. [1], was used during the interview for symptom assessment. Subject with a summed up RSI larger than 13 is considered to positive. Experienced otolaryngologists (EJC and SWL) evaluated the appearance using a laryngoscope and assessed laryngeal findings according to the Reflux Finding Score (RFS) [2]. Total scores can range from 0 (normal) to 26 (worst), and RFS in total of more than 7 is regarded as positive.
Topical nasal anesthesia and decongestion was achieved with intranasal pontocaine and neosynephrine, and a short spray of 10% benzocaine was used in the oropharynx for further analgesia. Patients were examined fully awake and sitting upright with a Pentax flexible endoscope (VE-1530, Pentax Precision Instrument Co., Orangeburg, NY, USA). A lidocaine gel is used as a lubricant on the endoscope. The endoscope was advanced along the floor of the nose into the nasopharynx and turned inferiorly to allow visualization of the nasopharynx, oropharynx, supraglottis, and glottis. The patient was then asked to burp and swallow several times to allow visualization of the postcricoid space, and the endoscope was gently advanced until it was seen and felt to enter the esophagus. The entire length of the esophagus was evaluated after air insufflation, with special attention to the gastroesophageal junction. Slow withdrawal of the endoscope allowed re-evaluation of the esophagus and the best examination of the postcricoid area. If mucosal lesions or irregularities are noted, biopsy forceps are passed through the working channel and multiple biopsies are obtained.
Pearson χ2 tests were used for dichotomous variables, whereas t-tests were used for continuous variables. All tests were two-tailed using the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). A P-value less than 0.05 was considered significant.
Go to : 
There was no significant difference between two hospital group (groups A and B) in RSI, VAS (satisfaction, pain), complication rate, and the number of patients with LPRD.
Fifty-three patients (38.7%) had positive findings on TNE. Positive finding ratio was highest in group of dysphagia (7 among 9 patients, 78%). One hundred and two patients underwent TNE for screening examination for LPRD. Forty-two patients (41.1%) were found to have pathology (esophagitis, 41; esophageal diverticulum, 1), and the remaining 60 patients (58.9%) had no identifiable pathology. Nine patients were examined to look for a cause of dysphagia. Pharyngeal or esophageal stricture was seen in four patients. These patients were dilated successfully with esophageal balloon dilator (CRE esophageal balloon dilator, Boston Scientifics, Natick, MA, USA). Esophageal cancer was confirmed in one patient with dysphagia using subsequent directed biopsy. Esophagitis was confirmed in two patients with dysphagia. TNE was used to investigate metachronous lesions or routine follow-up screening in seventeen head and neck cancer patients. One second primary cancer was identified during the routine follow-up after total laryngectomy. Four patients were examined to look for a cause of blood tinged saliva. Positive finding was identified in one patient (esophagitis). We could not notice any positive finding in patients with vocal fold paralysis.
The average pain score on a VAS (0, no; 1, mild; 2, moderate; 3, most severe pain) was tolerable (mean score, 1.13±0.78), and the patients' satisfaction score (0, worst; 5, fair; 10, best) was fair (mean score, 6.34±1.49) (Table 2).
The procedure had to be abandoned in no patient. There was no significant complication in any of the patients. Three patients (2%) suffered from a vasovagal syncope due to direct stimulation of vagus nerve during TNE (Table 2).
Go to : 
Traditional esophagoscopy is performed with a large caliber flexible endoscope requiring intravenous sedation for patient comfort or with rigid endoscopes under general anesthesia in the operating room. Otolaryngologists are quite familiar with endoscopic intranasal anatomy and performing office-based procedures without needing conscious sedation. TNE allows endoscopic visualization of the aerodigestive tract from the nasal vestibule to the gastric cardia and 'one stop' service in investigations thus avoiding delays, costs and risks of contrast studies and rigid endoscopy [2,3,4,5,6,7,8]. Our experience demonstrates that the examination is easily performed, well tolerated, and safe procedure.
Our indications for performing TNE was the evaluation of LPRD, metastatic work-up or routine follow-up screening for head and neck cancer patients, to determine the cause of vocal fold paralysis, evaluation of dysphagia, blood-tinged saliva, or esophageal foreignbody. The 38.7% rate of positive esophageal findings in our patient population closely estimates that of Belafsky et al. [2] (44%). Our complication rates and discomfort level scores compare favorably with other authors. Aviv et al. [4]described a small series of 14 patients in which he reported similar tolerability scores of 2 of 10 on a visual analogue scale.
Most complications related to conventional upper endoscopy are due to conscious sedation; cardiopulmonary events comprise over 60% of all major complications [9]. Conscious sedation may result in oversedation, hypoxemia, arrhythmia, and vaso-vagal reaction. Unsedated TNE necessarily obviates the primary source of complications related to upper endoscopy. In addition, using air insufflation, irrigation, we were able to definitively examine all the pouches, ruling out the presence of tumor, without requiring further investigation.
In conclusion, TNE is a safe and well-tolerated procedure available to otolaryngologists that can be safely performed in an office setting. It provides a 'one stop' diagnosis service of immediate review and efficient management of a wide range of esophageal findings.
Go to : 
References
1. Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. 2002; 6. 16(2):274–277. PMID: 12150380.

2. Belafsky PC, Postma GN, Daniel E, Koufman JA. Transnasal esophagoscopy. Otolaryngol Head Neck Surg. 2001; 12. 125(6):588–589. PMID: 11743456.

3. Postma GN, Bach KK, Belafsky PC, Koufman JA. The role of transnasal esophagoscopy in head and neck oncology. Laryngoscope. 2002; 12. 112(12):2242–2243. PMID: 12461347.

4. Aviv JE, Takoudes TG, Ma G, Close LG. Office-based esophagoscopy: a preliminary report. Otolaryngol Head Neck Surg. 2001; 9. 125(3):170–175. PMID: 11555750.

5. Postma GN, Cohen JT, Belafsky PC, Halum SL, Gupta SK, Bach KK, et al. Transnasal esophagoscopy: revisited (over 700 consecutive cases). Laryngoscope. 2005; 2. 115(2):321–323. PMID: 15689759.

6. Aviv JE. Transnasal esophagoscopy: state of the art. Otolaryngol Head Neck Surg. 2006; 10. 135(4):616–619. PMID: 17011427.

7. Andrus JG, Dolan RW, Anderson TD. Transnasal esophagoscopy: a high-yield diagnostic tool. Laryngoscope. 2005; 6. 115(6):993–996. PMID: 15933508.

8. Price T, Sharma A, Snelling J, Bennett AM, Qayyum A, Bradnam T, et al. How we do it: the role of trans-nasal flexible laryngo-oesophagoscopy (TNFLO) in ENT. One year's experience in a head and neck orientated practice in the UK. Clin Otolaryngol. 2005; 12. 30(6):551–556. PMID: 16402984.

9. Chan MF. Complications of upper gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 1996; 4. 6(2):287–303. PMID: 8673329.

Go to : 




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download