This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
Coblation is operated in low temperature, so it is proposed that tonsillectomy with coblation involves less postoperative pain and allows accelerated healing of the tonsillar fossae compared with other methods involving heat driven processes. However, the results of the previous studies showed that the effect of coblation tonsillectomy has been equivocal in terms of postoperative pain and hemorrhage. Though, most of the previous studies which evaluated coblation tonsillectomy were performed in children. Recently, electrocautery tonsillectomy has been used most widely because of the reduced intraoperative blood loss and shorter operative time compared to other techniques. This prospective study compared intraoperative records and postoperative clinical outcomes in adolescents and adults following coblation and electrocautery tonsillectomies.
Methods
Eighty patients over 16 years of age with histories of recurrent tonsillitis were enrolled. The patients were randomly allocated into coblation (n=40) and electrocautery tonsillectomy groups (n=40). All operations were performed by one surgeon who was skilled in both surgical techniques. Intraoperative parameters and postoperative outcomes were checked.
Results
Postoperative pain and otalgia were not significantly different between the two groups; however, there was a tendency towards reduced pain and otalgia in the coblation group. More cotton balls for swabbing the operative field were used introoperatively in the electrocautery group (P=0.00). There was no significant difference in postoperative hemorrhage, wound healing, commencement of a regular diet, and foreign body sensation between the groups.
Conclusion
Only cotton use, which represented the amount of blood loss, was less in the coblation tonsillectomy group. Coblation tonsillectomy warrants further study with respect to the decreased postoperative pain and otalgia.
Go to :

Keywords: Coblation, Electrocautery, Tonsillectomy
INTRODUCTION
Coblation is a kind of radiofrequency surgery. The technique involves passing radiofrequency energy through a conductive medium (such as isotonic sodium chloride) and producing a plasma field. By coblation the medium is dissociated into free sodium ions, which are responsible for the destruction of intercellular bonds, resulting in tissue dissociation. This reaction is achieved at temperatures between 60℃ and 70℃ (compared with 400℃ to 600℃ in electrosurgery). The presence of cool, irrigating isotonic saline helps to limit the amount of heat delivered to the surrounding structures [
1,
2]. Coblation is operated in low temperature, so it is proposed that tonsillectomy with coblation involves less postoperative pain and allows accelerated healing of the tonsillar fossae compared with other methods involving heat driven processes.
However, the effect of coblation during tonsillectomy has not been fully determined, and the results in many studies have been equivocal in terms of postoperative pain and hemorrhage [
3]. In addition, most of the studies involving coblation tonsillectomies have focused on children whose clinical data were not easy to obtain directly and were not as reliable as in adolescents and adults [
2,
4,
5]. Pediatric tonsillectomy is also different with adult tonsillectomy in that pediatric tonsillectomy is often done for sleep apnea without history of inflammation while adult tonsillectomy often has an increased tendency toward scarring, adhesion and hypervascularity of the tonsil fossa because of the inflammation.
Since the first tonsil removal was performed by Celsus in 30 BC, multiple surgical techniques and a variety of instruments have evolved: electrocauterization, laser dissection, cryosurgery, bipolar dissection scissors, coblation-assisted tonsillectomy, and ultrasonic scalpel tonsillectomy [
6]. During recent decades, electrocautery tonsillectomy has been used most widely compared to other surgical methods based on the reduced intraoperative blood loss and shorter operative time. However, electrosurgery is associated with increased postoperative pain [
7,
8].
Therefore, the present prospective randomized study was designed to evaluate the intraoperative records and postoperative clinical outcomes between coblation and electrocautery tonsillectomy procedures in adolescents and adults.
Go to :

MATERIALS AND METHODS
Subjects
Patients who underwent tonsillectomy with a history of recurrent tonsillitis in the Department of Otorhinolaryngology-Head and Neck Surgery of Korea University Guro Hospital between August 2009 and June 2010 were recruited. Patients with acute inflammation, sleep apnea, congenital anomalies, a history of peritonsillar abscess, coagulation disorders, a history of taking anticoagulants, neoplasms, and tonsillectomy with adenoidectomy for children were excluded.
Test procedures
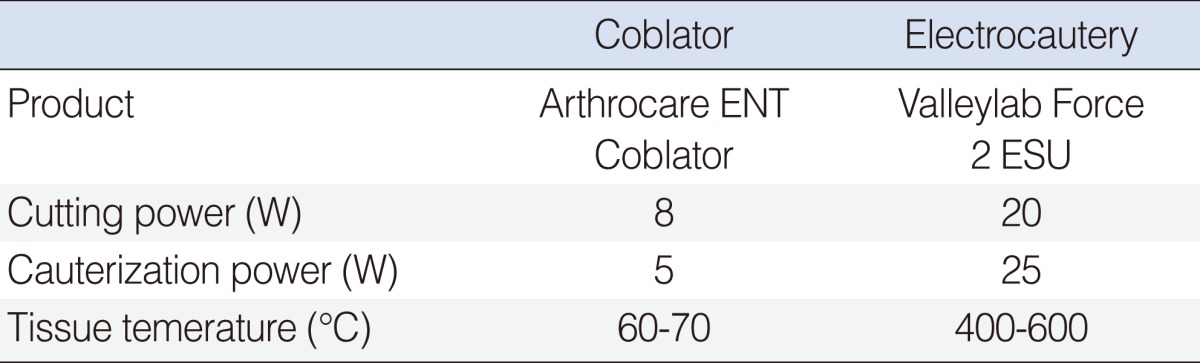
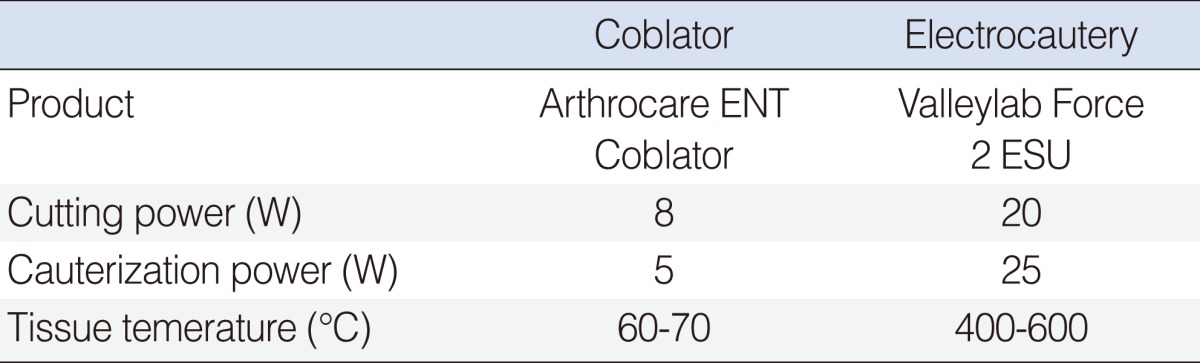
Patients were randomized into two groups: forty patients with coblator tonsillectomy and the other 40 patients with electrocautery tonsillectomy. The patients and their families were given detailed information about the study. Informed consent was obtained. Institutional Review Board approval was granted to carry out this study (MD 10008-004). All operations in this study were performed with the patients under general anesthesia and the patients were unaware of the surgical technique used. In each operation, coblation (Arthrocare ENT Coblator II, Sunnybale, CA, USA) or electocauterization (Valleylab Force 2 ESU, Boulder, CO, USA) was used; the power settings are summarized in
Table 1. All operations were performed by the same surgeon who was skilled in both surgical techniques and was unaware of the operative technique until entering the operation room. The operation time and cotton counts were recorded. The operation time was measured from the first incision to completion of hemostasis of the tonsillar bed. Cotton balls, 1 cm
3 in size, were counted to evaluate the intraoperative blood loss and the surgeon did not use any suctioning for intraoperative hemorrhage. Cottons entirely soaked with blood were counted. Intramuscular analgesics during the hospitalization and oral analgesics after discharge were used for pain control. All patients were discharged on postoperative day (POD) 2 and all patients used the same medications after discharge. Postoperative clinical outcomes included pain score by visual analoge scale (VAS), presence of otalgia, postoperative hemorrhage, wound healing, foreign body sensation, and the POD that a regular diet commenced. The pain score and otalgia were evaluated on PODs 0, 1, 2, 7, and 14. Postoperative hemorrhage was divided into acute (within 24 hours) and delayed categories (after 24 hours). Hemorrhage was defined as bleeding requiring medical or surgical intervention. Foreign body sensation was evaluated on PODs 14 and 28. Wound healing was subjectively evaluated by the operating surgeon, who had no information about the procedure that had been used. The subjective assessment was based on the following grade explanations at the operation site: 25%, visible white plaque incompletely covering the operative site; 50%, white plaque covering the operative site completely; 75%, visible, incomplete epithelized mucosa; 100%, completely epithelized operative site.
Table 1
Comparisons between coblator and electrocautery tonsillectomies

Statistical analysis
The results were analyzed with SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) using the Mann-Whitney U-test. A P-value<0.05 was considered significant.
Go to :

RESULTS
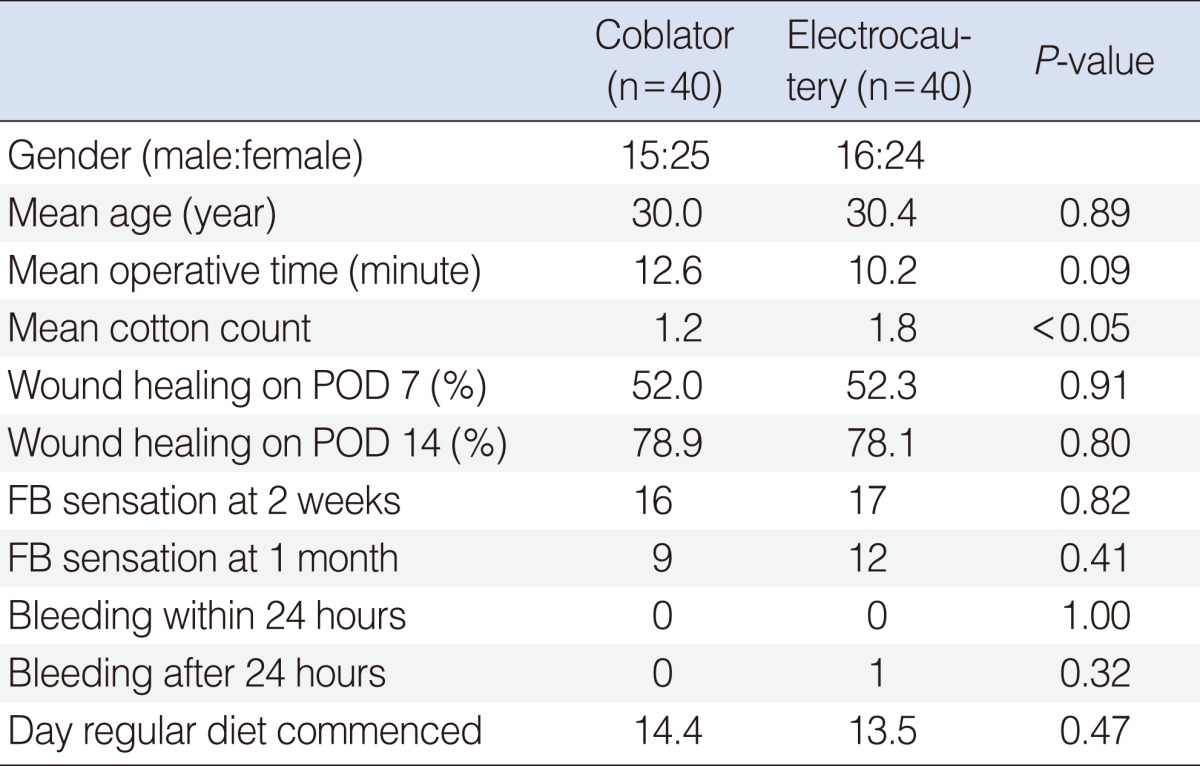
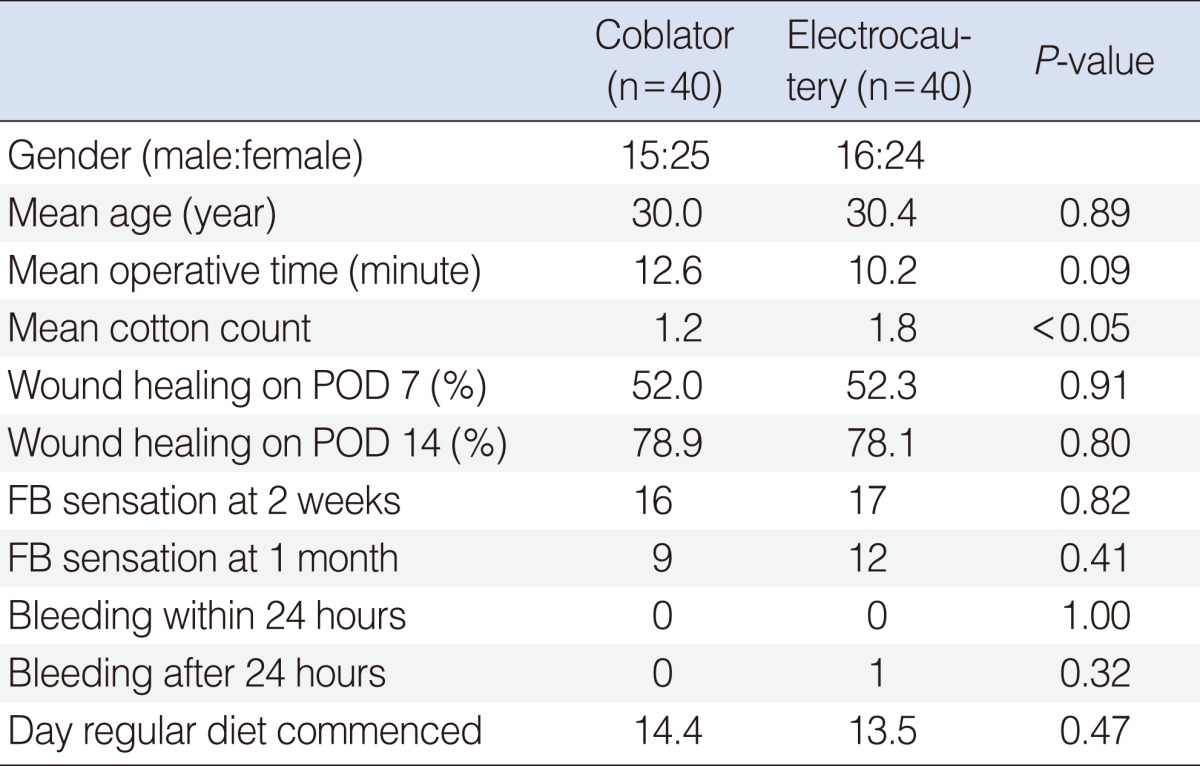
Thirty-one males and 49 females were enrolled in the current study (age range, 16 to 53 years). There was no significant difference in the age and gender between the two groups.
The mean operative time was 12 minutes 36 seconds in the coblation group, and 10 minutes 12 seconds in the electrocautery group. The difference between the groups was not significant but considerable (P=0.09).
Pain scores and postoperative otalgia were not different between the groups (
Figs. 1,
2); however, there was a tendency towards less postoperative pain and otalgia in the coblation group than the electrocautery group.
 | Fig. 1Postoperative visual analoge scale (VAS) pain scores. No significant difference was evident between the coblator and electrocautery groups; however, there was a tendency towards less pain in the coblation group. P-values at postoperative day (POD) 0, 1, 2, 7, and 14 are 0.31, 0.99, 0.59, 0.19, and 0.41 each. 
|
 | Fig. 2Postoperative number of patients with otalgia. A tendency towards less otalgia was evident in the coblation group. P-values at postoperative day (POD) 0, 1, 2, 7, and 14 are 0.42, 1.00, 0.79, 0.81, and 0.46 each. 
|
More cotton balls were used in tonsillectomies with electrocauterization (
P<0.05). There was no significant difference in wound healing, day a regular diet commenced, and foreign body sensation between the two groups (
Table 2). There was no acute postoperative hemorrhage in both groups. Delayed postoperative hemorrhage occurred in one patient in the electrocautery group. The hemorrhage was controlled with bipolar cautery (
Table 2).
Table 2
Patient demographics and results

Go to :

DISCUSSION
Coblation tonsillectomy was introduced in 1998 [
9]. Coblation was thought to reduce postoperative pain and improve recovery time compared to existing techniques [
9-
12]. In reality, whether or not coblation tonsillectomy alleviates postoperative pain compared to other surgical techniques is undetermined. In one study, pediatric patients undergoing tonsillectomy with the coblator device reported less pain over a 10-day period than patients undergoing tonsillectomy with electrocautery or an ultrasonic scalpel [
11]. Another study demonstrated that coblation tonsillectomy for recurrent tonsillitis was significantly less painful than dissection tonsillectomy on days 1 (
P<0.001), 2 (
P=0.003), and 3 (
P=0.018) [
12]; however, opposing results have been reported with no reduction in pain scores with coblation compared to cold dissection or electrosurgery [
3,
10,
13]. A 2005 study concluded that the use of coblation to perform tonsillectomy does not confer any symptomatic benefits to the patient over conventional cold dissection tonsillectomy [
13]. These studies were all performed in pediatric patients except only one study.
The present study sought to clarify the clinical advantages of coblation by accessing clinical outcomes of coblation tonsillectomy compared to electrocautery tonsillectomy especially in adolescents and adults. As reported herein, there was no significant benefit in the coblator group compared to the electrocautery group, except that fewer cotton balls were used to absorb blood. The follow-up pain scores and the number of patients with otalgia tended to be lower in the coblator group compared to the electrocautery group.
The mean operative time was longer, albeit not significantly, in the coblation group (
P=0.09). We consider this difference could be significant if larger number of patients are included in the study. This result is quite similar to previous studies [
10,
11,
14].
Delayed postoperative hemorrhage occurred in one patient in the electrocautery group. Most previous studies have shown no significant difference in the postoperative hemorrhage rates [
15,
16]. Postoperative hemorrhage did not influence postoperative pain and other parameters.
Wound healing was measured by carefully observing the tonsillar fossa. In the present study, no significant difference existed between the groups (
P=0.80. However, a study that analyzed results from 10 adults reported that coblation resulted in more rapid healing of the tonsillar fossa than bipolar dissection [
17]. We consider that this difference reflects the subjective method and small sample size. A study undertaken to objectively evaluate tissue damage after tonsillectomy, including a histologic evaluation of the tonsil margins, showed significantly shallower tissue injuries in the coblation group compared to the electrocautery group [
14].
The day a regular diet commenced and foreign body sensation were also evaluated, and no significant difference existed in these parameters. Foreign body sensation after coblation tonsillectomy has not been reported. We believe that foreign body sensation is not influenced by the dissection method or a difference in the temperature within the surgical field. The starting day of a regular diet has been evaluated in many studies, but the results have been equivocal [
10,
11,
13]. The present data provide further information that will help clarify this issue.
The number of cotton balls used was significantly less in the coblation group than the electrocautery group. We consider this difference to be due to the hemostatic function and reduced tissue damage caused by the coblator; however, the present finding conflicts with earlier studies. Comparions of coblator and monopolar electrosurgery tonsillectomies have shown similar hemostatic abilities [
11,
18]. The dichotomy between the current and previous results may reflect the different methods used to estimate the amount of blood loss. In the present study we used the number of cotton balls as an indicator of blood loss, while previous studies visually estimated the amount of blood loss intraoperatively. Although there could be a little difference in the amount of blood soaked in one cotton, we consider our method is more objective than other studies.
Many studies have evaluated the intraoperative records and postoperative clinical outcomes of coblation tonsillectomy compared to other techniques. Compared to previous studies, the present study had some advantages. Most of the previous studies focused on children, whose clinical data were not always easy to obtain directly and thus lacked reliability, and pediatric tonsillectomy is often done for sleep apnea without history of inflammation while adult tonsillectomy often has an increased tendency toward scarring, adhesion and hypervascularity of the tonsil fossa because of the inflammation. The current study focused on adolescents and adults, from whom more accurate and reliable data were obtained.
From this study, we could not conclude that coblation tonsillectomy is a less painful technique than electrocautery tonsillectomy in adolescents and adults. However, coblation tonsillectomy warrants further research because of the tendency towards less postoperative pain and otalgia.
Go to :

ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Health technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A090084).
Go to :

Notes
Go to :

References
1. Belloso A, Chidambaram A, Morar P, Timms MS. Coblation tonsillectomy versus dissection tonsillectomy: postoperative hemorrhage. Laryngoscope. 2003; 11. 113(11):2010–2013. PMID:
14603065.

2. Plant RL. Radiofrequency treatment of tonsillar hypertrophy. Laryngoscope. 2002; 8. 112(8 Pt 2 Suppl 100):20–22. PMID:
12172233.

3. Burton MJ, Doree C. Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev. 2007; 7. (3):CD004619. PMID:
17636769.

4. Mitic S, Tvinnereim M, Lie E, Saltyte BJ. A pilot randomized controlled trial of coblation tonsillectomy versus dissection tonsillectomy with bipolar diathermy haemostasis. Clin Otolaryngol. 2007; 8. 32(4):261–267. PMID:
17651267.

5. Parker D, Howe L, Unsworth V, Hilliam R. A randomised controlled trial to compare postoperative pain in children undergoing tonsillectomy using cold steel dissection with bipolar haemostasis versus coblation technique. Clin Otolaryngol. 2009; 6. 34(3):225–231. PMID:
19531171.
6. Curtin JM. The history of tonsil and adenoid surgery. Otolaryngol Clin North Am. 1987; 5. 20(2):415–419. PMID:
3299218.
7. Maddern BR. Electrosurgery for tonsillectomy. Laryngoscope. 2002; 8. 112(8 Pt 2 Suppl 100):11–13. PMID:
12172230.

8. Lowe D, van der Meulen J. National Prospective Tonsillectomy Audit. Tonsillectomy technique as a risk factor for postoperative haemorrhage. Lancet. 2004; 8. 364(9435):697–702. PMID:
15325834.
9. Shah UK, Dunham B. Coblation for tonsillectomy: an evidence-based review. ORL J Otorhinolaryngol Relat Spec. 2007; 69(6):349–357. PMID:
18033972.

10. Stoker KE, Don DM, Kang DR, Haupert MS, Magit A, Madgy DN. Pediatric total tonsillectomy using coblation compared to conventional electrosurgery: a prospective, controlled single-blind study. Otolaryngol Head Neck Surg. 2004; 6. 130(6):666–675. PMID:
15195050.

11. Parsons SP, Cordes SR, Comer B. Comparison of posttonsillectomy pain using the ultrasonic scalpel, coblator, and electrocautery. Otolaryngol Head Neck Surg. 2006; 1. 134(1):106–113. PMID:
16399189.

12. Polites N, Joniau S, Wabnitz D, Fassina R, Smythe C, Varley P, et al. Postoperative pain following coblation tonsillectomy: randomized clinical trial. ANZ J Surg. 2006; 4. 76(4):226–229. PMID:
16681537.

13. Philpott CM, Wild DC, Mehta D, Daniel M, Banerjee AR. A double-blinded randomized controlled trial of coblation versus conventional dissection tonsillectomy on post-operative symptoms. Clin Otolaryngol. 2005; 4. 30(2):143–148. PMID:
15839866.
14. Shah UK, Galinkin J, Chiavacci R, Briggs M. Tonsillectomy by means of plasma-mediated ablation: prospective, randomized, blinded comparison with monopolar electrosurgery. Arch Otolaryngol Head Neck Surg. 2002; 6. 128(6):672–676. PMID:
12049562.
15. Friedman M, LoSavio P, Ibrahim H, Ramakrishnan V. Radiofrequency tonsil reduction: safety, morbidity, and efficacy. Laryngoscope. 2003; 5. 113(5):882–887. PMID:
12792327.

16. Glade RS, Pearson SE, Zalzal GH, Choi SS. Coblation adenotonsillectomy: an improvement over electrocautery technique? Otolaryngol Head Neck Surg. 2006; 5. 134(5):852–855. PMID:
16647547.

17. Timms MS, Temple RH. Coblation tonsillectomy: a double blind randomized controlled study. J Laryngol Otol. 2002; 6. 116(6):450–452. PMID:
12385358.

18. Chang KW. Randomized controlled trial of Coblation versus electrocautery tonsillectomy. Otolaryngol Head Neck Surg. 2005; 2. 132(2):273–280. PMID:
15692541.

Go to :






 Citation
Citation Print
Print



 XML Download
XML Download