Abstract
Objectives
The clinical features of various facial deformities in Korean leprosy patients were evaluated according to the type of leprosy.
Methods
One hundred ninety six patients with leprosy were examined for various facial deformities using a nasal speculum, endoscope, and digital camera. The frequency and severity of external nasal deformities and septal perforations were evaluated according to the type of leprosy. Eye deformities, ear deformities, and facial palsy were also assessed.
Results
Seventy-one patients (36.2%) displayed external nasal deformities: 28 minimal contractures, three cartilage contractures, two bony-cartilage contractures, and 38 skin defects. The external nasal deformity and severe form deformity in lepromatous types were more frequent compared to other types (P<0.05 for each variable). Twenty-three patients (9%) displayed septal perforations, among whom 11 had cartilaginous perforations and 12 had bony-cartilaginous perforations. The frequency of septal and bony-cartilaginous perforations did not differ significantly between the types of leprosy (P>0.05 for each variable). Sixty-one patients (31.1%) had eye deformities and 19 patients (9.7%) had facial nerve palsy, common in the borderline type. No cases of ear deformities were observed.
Go to : 
Leprosy, or Hansen disease, is an infectious disease caused by Mycobacterium leprae, first characterized by G. Armauer Hansen in 1873. This disease displays a long latency period and a diverse clinical course. It is an immune system-related disease, with various types according to individual immune responses and it can resolve spontaneously [1]. Because the respiratory organs, particularly the nasal cavity, are the major injection route of airborne germs, the nasal mucosa is the main affected site. Findings in the nasal cavity have been useful in the diagnosis of leprosy [2]. And among them, nasal deformities proceed, in sequence, from nasal mucosal atrophy to invasive nodules, septal perforations, columellar retraction, and the saddle nose [3]. The invading bacillus has three main targets: peripheral neural tissues (Schwann cells), small vessels, and monocytes [4]. Nerve damage occurs at a later disease stage toward the end of the lepromatous spectrum, when sensory loss generally involves the distal extremities, with the facial nerve being commonly involved [5].
Ridley and Jopling [6] first classified leprosy in an immunological sense on the basis of skin findings, motor and sensory changes, and biopsy findings as indeterminate (I), tuberculoid (TT), borderline tuberculoid (BT), mid-borderline (BB), borderline lepromatous (BL), and lepromatous (LL). TT primarily affects the skin and peripheral nerves, while LL primarily affects the skin and mucosa and displays higher infectivity than TT. In LL, bacterial proliferation is not suppressed, leading to spread to other systemic organs. Mucosal tissues are commonly violated, as is the first half of the eyeball and the upper airways. Particularly in the early disease stages, the nasal mucosa is involved in more than 95% of all LL cases [7-9]. To date, the facial deformities of the patients with leprosy have been studied only in the Caucasian population [1-5,7-9]. We therefore attempted to analyze the extent of facial deformities according to the type of leprosy in Korean patients.
Go to : 
From 2005 to 2009, we examined 350 patients with leprosy residing in the leper colony in the town of Doyang, Sorok Island (Sorok-ri, Doyang-eup, Goheung-gun, Jeollanam-do). To reduce selection bias, 144 patients who died during the survey period were excluded. In total, the 196 patients (122 men and 74 women) were included. Their mean age was 71 years (range, 26 to 104 years), and 146 patients (74.5%) were over 65 years of age. We performed physical examinations by visiting the patients rather than have them visit an outpatient clinic. This study was approved by the Institutional Review Board of Chuncheon Sacred Heart Hospital.
The types of leprosy were classified into TT, borderline (B), or LL based on medical records. We took digital pictures of the facial shapes to record facial deformities, with the informed consent of the patients. In addition, we confirmed the structural deformities and nasal septal perforation of the nasal cavity using a nasal speculum and a 0° nasal endoscope (4 mm; Carl Zeiss AG, Oberkochen, Germany).
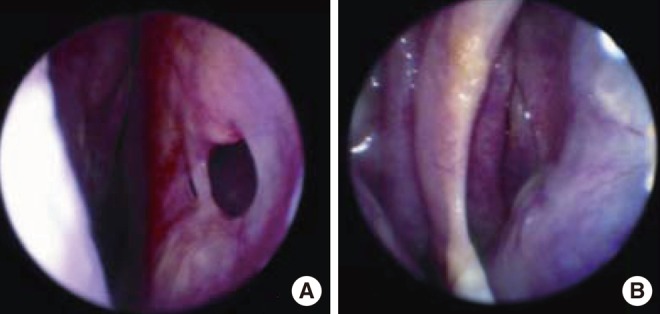
The facial deformities included nasal deformity, nasal septal perforation, eye deformities, external ear involvement, and facial nerve palsy. Nasal deformities were divided into four classes according to the extent of damage to nasal skeleton: minor deformity (minimal contracture), moderate (cartilage contracture), and severe deformity (severe contracture due to cartilage and nasal bone destruction), as well as skin defects. The nasal septal perforations were divided into two classes according to the perforation site: cartilaginous type (when the perforation was restricted to the cartilage) and bony-cartilaginous type (when the perforation included the bony portion, with the cartilage) (Fig. 1). In addition, external eye and external ear deformities were assessed. The facial nerve palsies were divided into six classes (I-VI) according to the House-Brackmann grading system [10], and classes above II were included in the facial nerve palsy group.
The chi-square test was used to analyze the differences in the facial deformities between each type of leprosy. The data were analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Probability values of P<0.05 were deemed to indicate statistical significance.
Go to : 
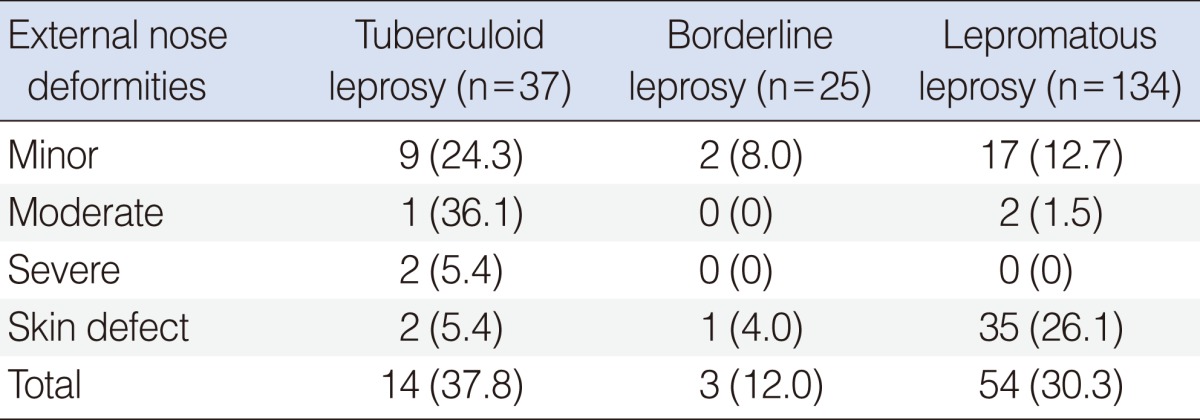
Thirty-seven patients (18.9%) displayed TT, 25 patients (12.8%) had B, and 134 patients (68.4%) had LL. Of the 196 patients, external nasal deformities occurred in 71 patients (36.2%). The frequencies of external nasal deformities were 14 of 37 patients (37.8%) in the TT group, 3 of 25 patients (12%) in the B group, and 54 of 134 patients (30.3%) in the LL group. The TT group displayed the highest frequency, and the difference among the three groups was significant (P<0.001) (Table 1). Two patients (1%) with severe deformities and 38 (19.4%) with skin defects were observed, which were 4 of 14 patients (28.6%) in the TT group, 1 of 3 patients (33.3%) in the B group, and 35 of 54 patients (64.8%) in the LL group. The LL group displayed the highest percentage of severe deformities (P=0.007).
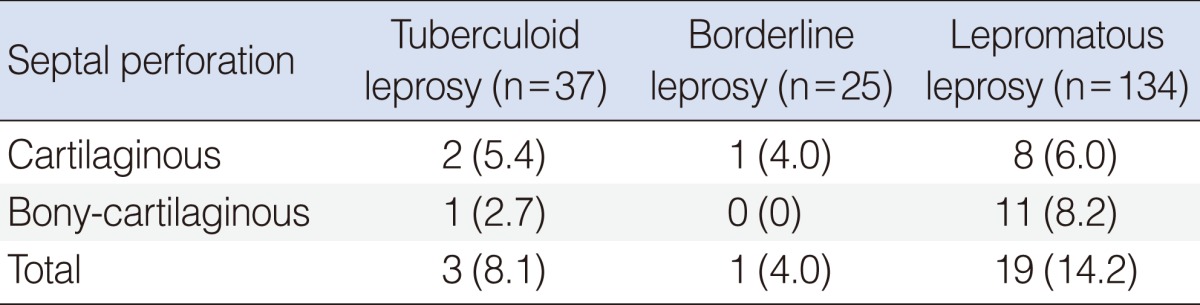
Twenty-three patients (9%) displayed septal perforations: 3 of 37 patients (8.1%) in the TT group, 1 of 25 patients (4%) in the B group, and 19 of 134 patients (14.2%) in the LL group. Septal perforations were most common in the LL group, but these differences were not significant (P=0.455) (Table 2). Twelve bony-cartilaginous perforations (6.1%) were observed, 1 of 3 patients (33.3%) in the TT group, none of 3 patients (0%) in the B group, and 11 of 19 (57.9%) in the LL group. No significant differences were observed among the groups (P=0.413).
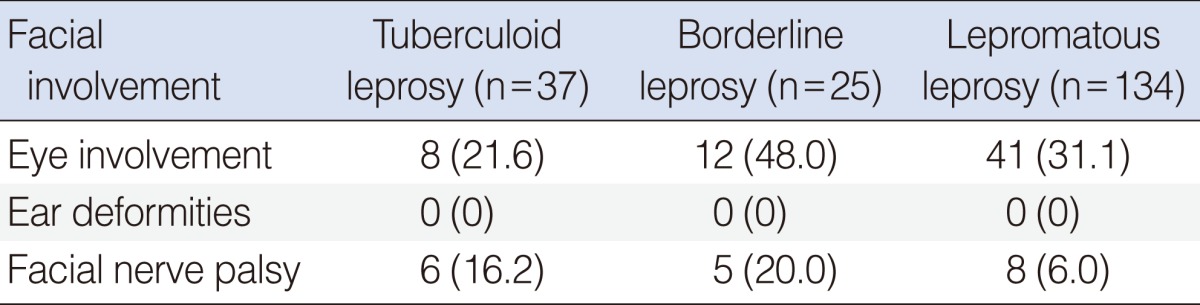
Sixty-one cases (31.1%) of eye deformities were observed, which were 8 of 37 patients (21.6%) in the TT group, 12 of 25 patients (48%) in the B group, and 41 of 134 patients (30.6%) in the LL group. Eye deformities were most common in the B group, but the finding was not significant (P=0.086). We found no cases of ear deformities. Nineteen patients (9.7%) had facial nerve palsies: 6 of 37 patients (16.2%) in the TT group, 5 of 25 patients (20%) in the B group, and 8 of 134 patients (6%) in the LL group. The LL group displayed the significantly lowest prevalence of facial palsy (P=0.033) (Table 3).
Go to : 
The majority of facial deformity studies have been based on Caucasian characteristics [11-13]. In the present study, we analyzed the facial deformities in a large group of Korean patients with leprosy. Nasal deformities were observed in 36.2% patients, septal perforation in 9%, eye deformities in 31.1%, and facial nerve palsies in 9.7%. No ear deformities were observed.
The prevalence of leprosy is known to be decreasing. However, the disease is still widely distributed, primarily in underdeveloped countries like India, South America, and Africa. Leprosy primarily affects the peripheral nervous system, and numerous secondary sites including the skin and nasal mucosa. The disease is accompanied by numerous complications and sequelae, and these manifestations appear somewhat differently in each disease type. In the early stages, TT typically affects the peripheral nerves asymmetrically, and can produce numbness, tenderness, thickening, and muscle weakening. Moreover, it can induce facial nerve palsy and eyelid palsy, accompanied by keratitis and corneal ulcers. The intranasal lesions are uncommon in TT. In contrast, in LL, the skin and the mucosa are initially affected, with the erosion of the nasal mucosa leading to infiltrative nodules, crust formation, nasal obstruction, nasal bleeding, septal perforations, columellar retraction, and saddle nose in a regular sequence [7]. The neurologic changes come later in LL. The neural invasion progresses very slowly, bilaterally, and symmetrically, and it is independent of the skin lesions [4,14].
Shehata et al. [11] found a 97% instance of nasal involvement in 260 male patients. Among them, nasal deformities occurred in 47.7% patients and septal perforation in 34%. These frequencies were higher than those in our study (36.2% and 9%, respectively). We additionally found that nasal deformities were more commonly encountered in TT than B and LL. This finding indicated that facial deformities appeared in numerous patients with TT and B in addition to LL. However, severe deformities and skin defects, representing more serious deformities, were more frequent in LL than TT and B. Unlike previous reports [7], the incidence of septal perforations was similar regardless of the type of leprosy. In addition, no significant occurrence of bony cartilage representing a more severe condition occurred according to the type of leprosy.
Loss of the eyebrows and eyelashes was noted in 21%-38% of LL, and eye disease was encountered in almost all LL cases [12,13]. Ear deformities of Caucasian patients with leprosy were reported in 38%-73% of patients [12,13]. However, in this study, Korean patients with leprosy showed more frequent eye deformities in the B group (48%) than in the TT (21.6%) and LL (30.6%) groups, and ear deformities were not observed. Facial nerve paralysis was seen in less than 25% of all cases of leprosy [12,13,15]. No previous studies have reported the differences in the frequency of facial nerve palsy by the disease type. In the present study, facial nerve palsy was assessed in 9.7% of patients and displayed the lowest incidence in LL. This result supports that in LL, unlike TT, the disruption of neural tissue is typically not severe and is preserved for a longer time period [4,14].
In this study, the frequency and severity of external nasal deformities, septal perforation, eye involvement, ear deformities, and facial nerve palsy according to the leprosy type showed clear differences from previous reports. These facial deformities findings are based on the assertion that each subdivision by variation of the host resistance is flexibly shifted [3].
Limitations of this study must be acknowledged. We could not classify the borderline type into BT, BB, and BL and analyze the clinical manifestations according to the prevalence periods, as many of the medical records were produced 3 to 4 decades ago and did not display a sufficiently accurate classification of leprosy or the prevalence period. In addition, we did not objectively assess the deformities. Nevertheless, compared to other studies of non-Asian patients, we presume that these manifold differences between the races gave rise to the variable results observed in this study.
This study showed that external nasal deformities and septal perforations occur not only in LL, but additionally in TT or B types, and that eye involvement and facial nerve palsy are common in the B type. However in Korean leprosy, unlike in Caucasians, ear deformities were not observed, suggesting that considerable differences in facial deformities exist among the races. Additional studies are now required to further explore these racial discrepancies.
Go to : 
ACKNOWLEDGMENTS
This work was supported by a grant from the Hallym University Medical Center Research Fund (01-2011-17) and Bio-industry Technology Development (112007-05-1-SB010), Ministry for Food, Agriculture, Forestry and Fisheries, Republic of Korea.
Go to : 
References
2. Gupta A, Seiden AM. Nasal leprosy: case study. Otolaryngol Head Neck Surg. 2003; 11. 129(5):608–610. PMID: 14595291.

3. Barton RP. Clinical manifestation of leprous rhinitis. Ann Otol Rhinol Laryngol. 1976; Jan-Feb. 85(1 Pt 1):74–82. PMID: 1259317.
4. Abulafia J, Vignale RA. Leprosy: pathogenesis updated. Int J Dermatol. 1999; 5. 38(5):321–334. PMID: 10369539.

6. Ridley DS, Jopling WH. Classification of leprosy according to immunity: a five-group system. Int J Lepr Other Mycobact Dis. 1966; Jul-Sep. 34(3):255–273. PMID: 5950347.
7. Barton RP. A clinical study of the nose in lepromatous leprosy. Lepr Rev. 1974; 6. 45(2):135–144. PMID: 4421363.

8. Davey TF, Rees RJ. The nasal dicharge in leprosy: clinical and bacteriological aspects. Lepr Rev. 1974; 6. 45(2):121–134. PMID: 4608620.
9. Davey TF, Barton RP. Multiple nasal smears in early lepromatous leprosy. Lepr Rev. 1974; 6. 45(2):158–165. PMID: 4608404.

10. House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985; 4. 93(2):146–147. PMID: 3921901.

11. Shehata MA, Abou-Zeid SA, El-Arini AF. Leprosy of the nose clinical reassessment. Int J Lepr Other Mycobact Dis. 1974; Oct-Dec. 42(4):436–445. PMID: 4617723.
12. Antia NH. Reconstruction of the face in leprosy. Ann R Coll Surg Engl. 1963; 2. 32:71–98. PMID: 14013322.
13. Reichart P. Facial and oral manifestations in leprosy: an evaluation of seventy cases. Oral Surg Oral Med Oral Pathol. 1976; 3. 41(3):385–399. PMID: 1061926.
14. McDougall AC, Rees RJ, Weddell AG, Kanan MW. The histopathology of lepromatous leprosy in the nose. J Pathol. 1975; 4. 115(4):215–226. PMID: 1099180.
15. Lighterman I, Watanabe Y, Hidaka T. Leprosy of the oral cavity and adnexa. Oral Surg Oral Med Oral Pathol. 1962; 10. 15:1178–1194. PMID: 13930596.

Go to : 




 Citation
Citation Print
Print


 XML Download
XML Download