Abstract
Objectives
Vascular leiomyoma is an uncommon benign tumor of smooth muscle origin that arises from the muscularis layer of blood vessel walls. We report our experiences with the clinical manifestations, pathologic characteristics, and management of vascular leiomyoma in the head and neck.
Methods
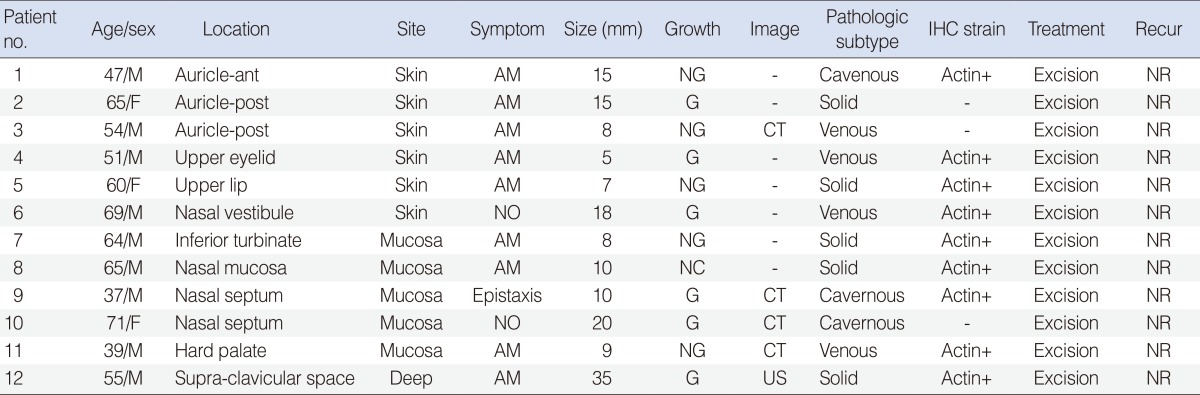
The clinical records of 12 patients with vascular leiomyoma of the head and neck in the 11-year period were reviewed retrospectively.
Results
The 12 patients included nine men and three women. The locations of the tumors were variable, including nasal cavity, auricle, hard palate, upper lip, upper eyelid, and supraclavicular space. All but three patients reported an asymptomatic spherical mass; the other three patients complained of intermittent epistaxis or unilateral nasal obstruction resulting from the tumor originating in the nasal cavity. All tumors were painless. Computed tomography consistently revealed a well-defined, intensely enhanced small mass on the mucosa. No case was dignosed corretly as vascular leiomyoma before surgical excision. All patients underwent localized surgical excision of the tumor without recurrence. Five of 12 tumors (42%) were of solid type, four (33%) were of venous type, and three (25%) were of cavernous in histological classification. The histologic type was not related to gender, site of occurrence, and presence of pain.
Vascular leiomyoma, which is derived from the smooth muscle of blood vessels, may occur anywhere in the skin or subcutaneous tissue [1]. The tumor usually occurs in the lower extremities as a slow-growing, firm, mobile and occasionally painful mass [2,3]. Vascular leiomyoma is an uncommon type of leiomyoma and rarely occurs in the head and neck. Vascular leiomyoma occuring on various anastomical sites in the head and neck have been described in case reports [4-13]. Description of head and neck vasclar leiomyomas with large case series are rare. We report our 11-year experience with the clinical manifestations, pathologic characteristics, and management of vascular leiomyoma in the head and neck.
The clinical records of 12 patients with vascular leiomyoma of the head and neck in the 11-year period between 2000 and 2010 were reviewed retrospectively. The clinical informations were summarized in Table 1. Pathologic specimen from each tumor was reviewed by the pathologist to confirm the diagnosis and subtype classification proposed by Morimoto [3]. This study was approved by the Institutional Review Board of Chonnam National University Hwasun Hospital.
Among the 12 patients, nine (75%) were male and three (25%) were female. The ages ranged from 37-71 years with a mean age of 49.3±7.9 years. Eight patients out of 12 (67%) were in their fifth and sixth decade. The locations of the tumors were variable, including the nasal cavity, auricle, upper eyelid, upper lip, hard palate, and supraclavicular space (Table 2). All except one tumor located deep in the supraclavicular space developed in the skin or mucosa such as the oral or nasal mucosa. There were no multiple cases in our series.
Most patients presented with an asymptomatic, well-defined spherical mass in the head and neck (Table 3). In three patients, the tumors originated in nasal cavity; these patients complained of progressive nasal obstruction and/or recurrent epistaxis. No patients in our series complained of pain. The tumors ranged in size from 5-35 mm with a mean of 13.3±6 mm. All but one tumor was under 20 mm in diameter. The large tumor measured 35 mm in diameter and it presented as an asymptomatic mass in the supraclavicular space. Six of the 12 patients (50%) subjectively complained of a slow-growing mass after they noted the mass. The mean size of five tumors originating from the nasal cavity was 13.2 mm, which is similar to that of the patients with other head and neck vascular leiomyomas.
Computed tomography (CT) for preoperative evaluation was performed in four patients. CT consistently revealed a well-defined, intensely enhanced small mass on the mucosa (Fig. 1). Ultrasonography yielded no characteristic findings for preoperative diagnosis. Fine needle aspiration biopsy was performed in three patients, but was not diagnostic as contamination by blood occurred. Neither case was dignosed correctly as vascular leiomyoma before surgical excision. All patients underwent localized surgical excision of the tumor. Three patients underwent tumor excision with a cuff of adjacent normal tissue. Nine patients underwent only enucleation of the tumor. Regardless the extent of resection, no patients had experienced a recurrence with a mean follow-up period of 52 months.
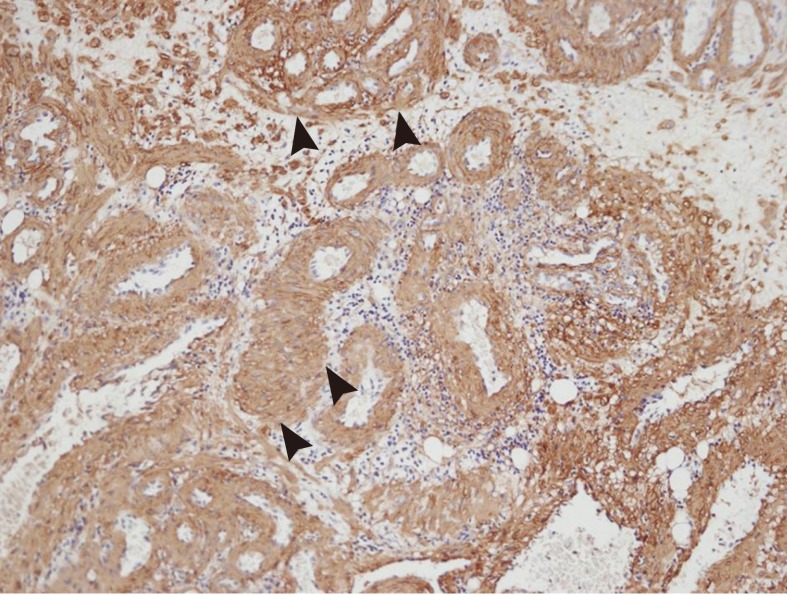
All 12 tumors shared the same basic histopathologic features revealed by hematoxylin and eosin (H&E) staining. The tumors were well-circumscribed and showed the presence and abundance of vascular spaces, surrounded by thick muscular walls composed of circumferentially arranged smooth muscle cells (Fig. 2). Immunohistochemical staining for actin and other special markers including desmin, CD31, and CD34 was performed in nine patients. Immunohistologic findings for actin showed strong positive reaction to smooth muscle fibers in all nine tumors (Fig. 3). In the histological classification proposed by Morimoto [3], five of 12 tumors (42%) were of the solid type, four (33%) were of the venous type, and three (25%) were of the cavernous type. The histologic subtype was not related to gender, site of occurrence, and symptoms including pain.
Vascular leiomyoma is a distinct subset of leiomyomas, most often presenting in the subcutaneous tissues of the extremities [1-4]. Only 8.5% of tumors arise from the head and neck area [2]. The mean age of the patients in our present series was 49.3 years, which is similar to that of the patients with non-head and neck vascular leiomyoma [2]. However, a male preponderance was observed in our head and neck series, in contrast to a female preponderance with non-head and neck vascular leiomyoma.
The locations of vascular leiomyoma in the head and neck varied. Vascular leiomyomas occuring in various anastomical sites such as auricle, larynx, tonsil, oral cavity, submandibular gland, parotid gland, turbinate, nasal cavity, retropharyngal space, and carotid sheath, have been reported [2-16]. In the present series, the most common sites of occurrence were the nasal cavity and auricle. Hachisuga et al. [2] also reported that the ear, lip, and nasal cavity were the most common sites. In addition, most of the tumors were located in the skin and mucosa in the present series and previous reports [2,14-16]. Vascular leiomyomas in the deep neck space were rare.
Vascular leiomyoma in the head and neck have the characteristic small tumor size (≤2 cm in diameter) in the present and previous studies [2,14-16]. The small tumor size may be due to their easily detectable superficial location and slow-growing nature [15]. If a vascular leiomyoma is deep seated, it could grow large, such as the 35 mm sized tumor originating from the supraclavicular space in our series. Five tumors that originated from the nasal cavity were similar to that of the patients with other head and neck vascular leiomyoma. However, they led to nasal symptoms such as nasal obstruction, and/or epistaxis due to the limited space of nasal cavity. They may be detected early due to these symptoms despite their hidden location. Vascular leiomyomas, except tumors in the nasal cavity, are asymptomatic. Although pain was the most characteristic subjective symptom in patients with vascular leiomyoma in the other regions, no patients in our head and neck series complained of pain.
Morimoto [3] proposed a classification system, which divided vascular leiomyoma into solid, cavernous, and venous types, and reported that these pathologic subtypes were related to clinical manifestations. Previous studies have reported that venous type develops more often in the head regions and the solid type is usually painful [2,3]. Although our case series was not large for definative conclusions, the solid type was the most common and the histologic subtypes had similar distribution. Regardless of the subtype, no patient had a painful or tender mass. The histologic subtype was not related to clinical manifestations such as gender, site of occurrence, and symptoms in the present series. Therefore, Morimoto's classification may not have clinical significance for head and neck vascular leiomyomas.
Preoperative diagnosis of the vascular leiomyoma is difficult. CT shows an intense enhanced submucosal or subcutaneous small mass, and could be helpful in cases of clinical suspicion of vascular leiomyoma. Cytological study was not diagnostic because of the rich vascularity in vascular leiomycoma. Localized surgical excision with histopathological study is the diagnosis and the treatment of choice. Despite their vascular nature, significant bleeding during the surgical excision is rarely seen [15,16]. Recurrences are notably rare [2,4]. In our series, nine patients of 12 (75%) underwent only enucleation of the tumor and no patients had experienced a recurrence. Although our case series would be small sample size for definite conclusions, we suggest that enucleation of the tumor is sufficient management with regard to the extent of tumor resection. We also have experienced no severe bleeding regardless of the location and subtype.
Most vascular leiomyomas can be correctly diagnosed by microscopy with conventional H&E staining [15]. Immunohistochemical stain for smooth muscle cells, such as actin, myosin, desmin, and for vascular endothelium such as CD31 and factor VIII can contribute to differential diagnosis, especially to rule out other spincle cell tumors such as hemangioma, angiofibroma, fibroma, angiomyolipma, and angiomyosarcoma [17].
In conclusion, vascular leiomyoma presents as a small and painless mass in various locations of the head and neck region. Localized surgical excision is the only way to make the diagnosis and gives excellent results. The histologic subtype classification does not affect the clinical manifestations and prognosis.
ACKNOWLEDGMENTS
This study was supported by a grant (CRI 10086-1) from Chonnam National University Hospital Research Institute of Clinical Medicine.
References
1. Duhig JT, Ayer JP. Vascular leiomyoma: a study of sixtyone cases. Arch Pathol. 1959; 10. 68:424–430. PMID: 13818517.
2. Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma: a clinicopathologic reappraisal of 562 cases. Cancer. 1984; 7. 54(1):126–130. PMID: 6722737.

3. Morimoto N. Angiomyoma (vascular leiomyoma): a clinicopathological study. Med J Kagoshima Univ. 1973; 24:663–683.
4. Anderson TD, Weinstein GS. Recurrent angiomyoma (vascular leiomyoma) of the larynx after laser excision. Otolaryngol Head Neck Surg. 2000; 11. 123(5):646–647. PMID: 11077360.

5. Choe KS, Sclafani AP, McCormick SA. Angioleiomyoma of the auricle: a rare tumor. Otolaryngol Head Neck Surg. 2001; 7. 125(1):109–110. PMID: 11458228.

6. Shetty SC, Kini U, D'Cruz MN, Hasan S. Angioleiomyoma in the tonsil: an uncommon tumour in a rare site. Br J Oral Maxillofac Surg. 2002; 4. 40(2):169–171. PMID: 12180214.

7. Leung KW, Wong DY, Li WY. Oral leiomyoma: case report. J Oral Maxillofac Surg. 1990; 7. 48(7):735–738. PMID: 2358952.

8. Ide F, Mishima K, Saito I. Angiomyoma in the submandibular gland: a rare location for a ubiquitous tumour. J Laryngol Otol. 2003; 12. 117(12):1001–1002. PMID: 14738618.

9. Kido T, Sekitani T. Vascular leiomyoma of the parotid gland. ORL J Otorhinolaryngol Relat Spec. 1989; 6. 51(3):187–191. PMID: 2660056.

10. Nall AV, Stringer SP, Baughman RA. Vascular leiomyoma of the superior turbinate: first reported case. Head Neck. 1997; 1. 19(1):63–67. PMID: 9030948.

11. Marioni G, Marchese-Ragona R, Fernandez S, Bruzon J, Marino F, Staffieri A. Progesterone receptor expression in angioleiomyoma of the nasal cavity. Acta Otolaryngol. 2002; 6. 122(4):408–412. PMID: 12125998.

12. Martínez Ferreras A, Rodrigo Tapia JP, Fresno MF, Suarez Nieto C. Angiomyoma of the retropharyngeal space. Acta Otorrinolaringol Esp. 2004; 12. 55(10):488–490. PMID: 15658559.
13. Reiner SA, Medina J, Minn KW. Vascular leiomyoma of the carotid sheath simulating a carotid body tumor. Am J Otolaryngol. 1998; Mar-Apr. 19(2):127–129. PMID: 9550446.

14. Natiella JR, Neiders ME, Greene GW. Oral leiomyoma: report of six cases and a review of the literature. J Oral Pathol. 1982; 11(5):353–365. PMID: 6815315.

15. Wang CP, Chang YL, Sheen TS. Vascular leiomyoma of the head and neck. Laryngoscope. 2004; 4. 114(4):661–665. PMID: 15064620.

16. Brooks JK, Nikitakis NG, Goodman NJ, Levy BA. Clinicopathologic characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 8. 94(2):221–227. PMID: 12221390.

17. Maeda Y, Hirota J, Osaki T, Hayashi K, Sonobe H, Otsuki Y. Angiomyoma of the upper lip: report of a case with electron microscopic and immunohistochemical observation. Br J Oral Maxillofac Surg. 1989; 6. 27(3):236–242. PMID: 2663055.

Fig. 1
Contrast enhanced neck axial computed tomography (CT) finding. (A) CT scan showed well-circumscribed, strong enhanced mass (white arrow head) on the mucosa of anterior nasal septum. (B) CT scan showed round enhanced mass (white arrow head) on left anterior portion of hard palate.

Fig. 2
Photomicroscopic finding showing thick-walled blood vessels (black arrow head) and smooth muscle bundles (white arrow head) (H&E, ×40).

Fig. 3
Immunohistologic finding for actin showing strong positive reaction to actin filament of smooth muscle fibers (black arrow head) (×100).




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download