MATERIALS AND METHODS
We prospectively evaluated patients who visited our hospital between May 2009 and December 2010 within 7 days of onset of unilateral facial palsy. Patients were excluded if they 1) presented with Bell palsy more than 1 week after onset; 2) were suspected of having Varicella zoster virus infection, based on physical and serologic examinations; 3) had a history of trauma or otologic surgery; 4) had other types of neurologic deficits; 5) had recurrent facial palsy; or 6) had a psychiatric disease. This study was approved by the Ethical Committee of Kyung Hee University Hospital, and all patients provided written informed consent.
All 60 included patients were treated with oral methylprednisolone for 12 days (64 mg/day for 4 days, 48 mg/day for 2 days, 40 mg/day for 2 days, 20 mg/day for 2 days, and 8 mg/day for 2 days). None of the patients received an antiviral agent. All patients were hospitalized for 7 days and followed-up as outpatients at 3 weeks, 6 weeks, and 3 months. During hospitalization, each patient was graded every 12 hours (twice per day) by both the HB scale and FNGS 2.0 grading system. Patients were also evaluated by both scales at each follow-up time point, with each patient evaluated at least twice for both systems by an otolaryngologist who understood both grading systems well. Patients were re-evaluated if there was any difference in the results of each grading system, and the final result was documented.
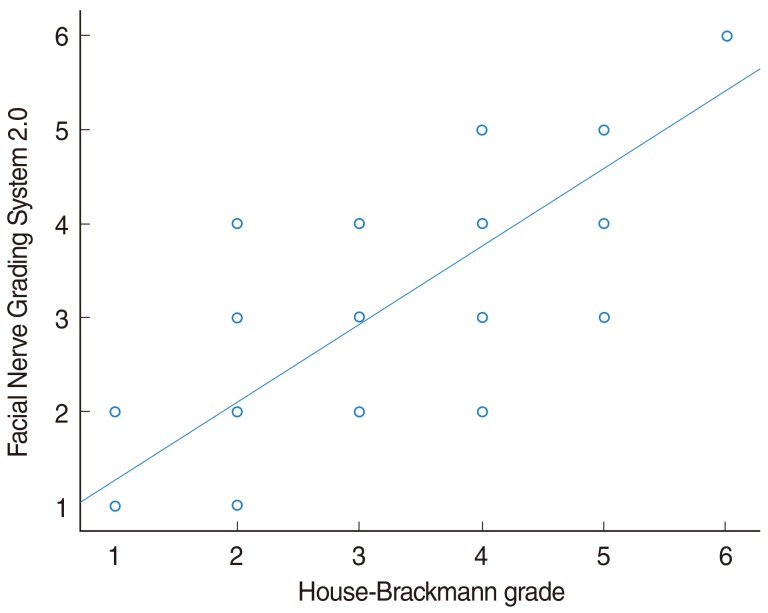
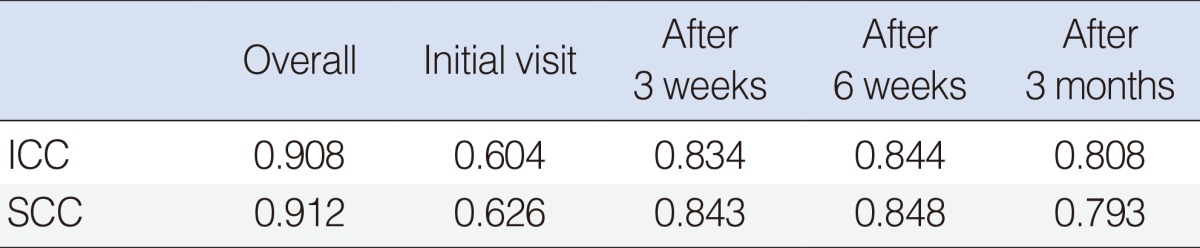
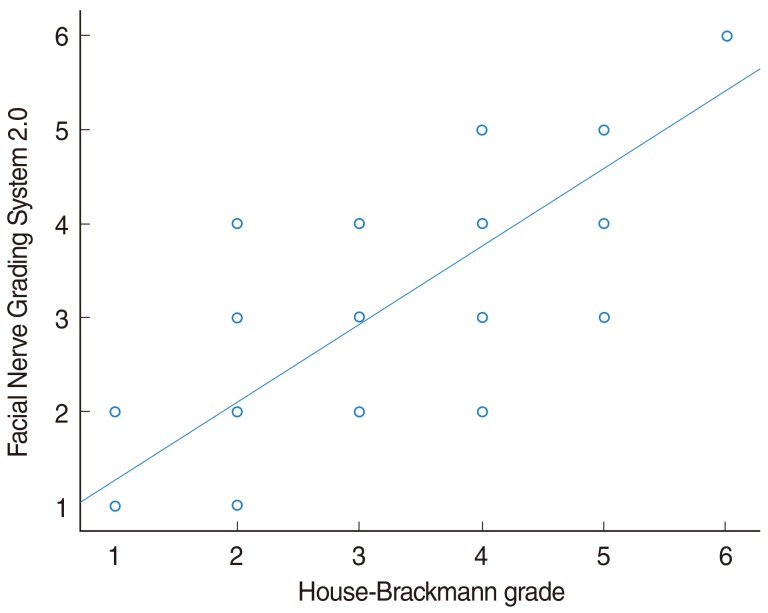
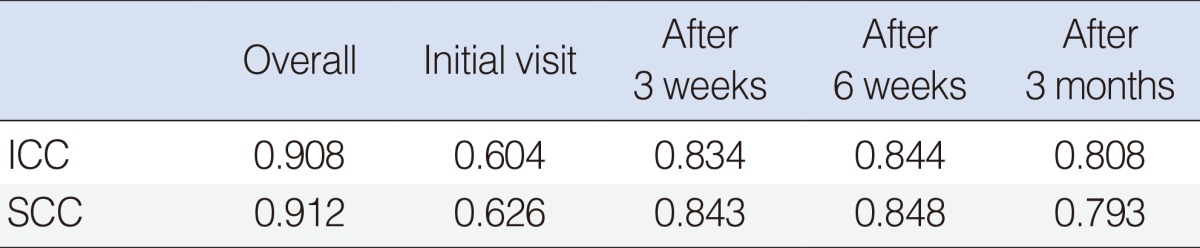
Agreement between the grading systems and their evaluation of patient prognosis were calculated by intraclass correlation coefficient (ICC), Spearman correlation analysis (SCC), and overall percentage agreement. Grade I at 3 months was considered the standard for complete recovery for evaluation of prognosis. Chi squared analysis was used to determine any difference between the two scales in judging recovery. Finally, the difference was confirmed by comparing the final results of the two grading systems and the results of regional assessments of the brow, eye, nasolabial fold, and oral region. All statistical analyses were performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA), and a P<0.05 was considered to indicate statistical significance.
Go to :

DISCUSSION
The HB grading system, which was chosen as the standard by the FND Committee of the American Academy in 1985, remains the most widely used facial nerve grading system [
1]. The motor function of the facial nerve can be rapidly and conveniently categorized into six HB grades. However, this system provides only gross impressions, thus limiting its usefulness. HB grading has several shortcomings, including: 1) regional assessment results are not properly reflected in the evaluation of overall grade of paralysis; 2) it can be difficult to evaluate patients with differing extent of weakness in each branch; 3) the HB system is not sensitive to changes in paralysis status; and 4) it can be difficult to compare clinically different recoveries [
2,
5-
7]. To minimize these shortcomings, studies have explored the Yanagihara and Sunnybrook grading systems.
Introduced in 1976, the Yanagihara system is a regional scale most frequently used in Japan. This system evaluates movements of 10 facial muscles, assigning each a score of 0-4 points, resulting in a maximum score of 40 points. When compared with HB grading, the kappa value was 0.64, indicating moderate agreement [
6]. Scores of 0-6, 8-14, 16-22, 24-30, 32-38, and 40 points on the Yanagihara system correspond to grades VI, V, IV, III, II, and I, respectively, of HB grading [
8]. In addition to not being widely used outside Japan, this system is too difficult for convenient use as the evaluation criteria are rather complex.
The Sunnybrook system grades paralysis by evaluating symmetry at rest and during voluntary movements, and, following a series of calculations, is used to gauge synkinesis on a 100-point scale. This system is sensitive in assessing changes in facial recovery [
2] and has been reported highly reliable, with intra- and inter-rater reliability similar for beginners and experts [
9]. However, it has been difficult for this system to replace HB grading.
FNGS 2.0, first introduced in 2009, was designed to overcome the limitations of existing grading systems. Although unquantifiable sensory deficits cannot be evaluated, detailed regional assessments of the brow, eye, nasolabial fold, and oral regions are possible, as are assessments of movement at any point of paralysis. In addition, the HB grading system ambiguously scored synkinesis as grade II or III, whereas the FNGS 2.0 system categorizes synkinesis in a separate category and scaled 0-3 depending on its severity, as well as evaluating final facial paralysis. The FNGS 2.0 also was designed to more clearly categorize grades difficult to distinguish in actual use, such as HB grades III and IV [
4].
We found that the rate of complete recovery was lower on the FNGS 2.0 (63%) than on the HB grading system (71%). Moreover, among patients with incomplete recovery, grades II and III were distributed differently on the two scales. These differences are likely due to the more detailed analysis on the FNGS 2.0, including regional assessment and evaluation of synkinesis, The FNGS 2.0 can be considered superior to HB grading, due to its stricter evaluations. Thus, the FNGS 2.0 is not only more useful in distinguishing between grades III and IV, but in differentiating low grade paralysis such as grades I-III. Proper assessment of complete recovery requires a stricter assessment system. This is especially applicable when evaluating, for example, the effects of antiviral agents on prognosis in patients with Bell palsy.
The reasons for the disagreement over grade I outcomes between the two scales remains unclear. In theory, normal is normal no matter what scale is used. We assumed that the difference in grade I may reflect inter-examiner variation. Because every known scale has subjective characteristics, examiners are unable to fully assess facial function [
4]. Although this possibility cannot be excluded, we believe that the principal reason for the difference between the scales is the ambiguity of HB grading in most cases, preventing accurate analysis without strict regional assessment [
4].
When we compared the results of regional assessment with the final grade, it differed from results observed using existing "regional" HB grading [
5]. In that study, the final grade match was highest for the eyes (61%), followed by the mid-face (40%) and mouth (32%). In comparison, we found that the highest HB grade match was for the eyes (67%), whereas the grade match on the FNGS 2.0 was higher for the mouth (72%) than for the eyes (63%).
Previously, evaluators focused primarily on whether the eye closed during different degrees of paralysis of each branch of the facial nerve [
5]. Although not identical, as the evaluation criteria differ for the "regional" grading system and FNGS 2.0, the scope of interest has widened beyond the eyes. Our more systematic regional assessment confirmed that the FNGS 2.0 has the advantage of assessing the various paralysis states of each nerve, and of these states being reflected in the final grade.
This study had several limitations. First, all patients were evaluated on both systems by a single examiner. Had patients been evaluated by two or more examiners, we could have calculated interobserver differences, enhancing the value of our results. Second, the final follow-up was performed 3 months after treatment; however, this period is too short to make decisions on facial paralysis. We had hypothesized that patients with Bell's "paresis" would completely recover within 3 months [
10], and we therefore regarded 3 months as the minimum period for determining patient prognosis. Since the main objective of this study was to assess the difference between the two facial nerve grading systems, the follow-up period itself was not a huge limitation. In other studies, many observers watch videos of patients [
4,
9,
11,
12]. In addition, a longer follow-up period increases the likelihood that some patients will drop out of the study, especially since patients may go elsewhere for a second opinion or seek alternative treatments. These problems may be overcome and long term results obtained by a multi-center study with larger numbers of patients.
Another limitation of this study was that we did not evaluate patients whose paralysis was due to other causes such as external injury or surgery. However, the purpose of this study was to compare the two grading systems in patients with unilateral Bell palsy. Future studies are needed to evaluate these grading systems in patients whose paralysis was due to other causes.
The future use of the FNGS 2.0 to grade patients with facial paralysis may result in a more objective evaluation of patient condition and recovery, both by regional assessment and by determination of level of synkinesis. Regional assessments using the HB grading system may enhance communication between researchers [
5].
Due to its simplicity and convenience, the HB grading system will be difficult to replace. However, the time required for FNGS 2.0 grading is not much longer. This system, which can overcome the shortcomings of the existing system may be a good tool for the more accurate evaluation of patients.
In conclusion, FNGS 2.0 showed moderate agreement with HB grading. The regional assessment capacity of the FNGS 2.0 yields stricter and more evaluations, enhancing the ability to assess patient grade and prognosis.
Go to :