INTRODUCTION
A mastoidectomy is performed as a surgical method to completely remove inflammatory tissues or cholesteatoma and to prevent recurrence in chronic otitis media (COM) patients. The procedure can be classified as a canal wall down mastoidectomy (CWDM, also known as open cavity mastoidectomy [OCM]) or canal wall up mastoidectomy (CWUM). In the case of CWDM, it is possible to remove the lesion completely by securing a sufficient surgical view. However, the disadvantages of CWDM include cavity problems, such as otorrhea and dizziness, and difficulty in wearing hearing aids after surgery. On the other hand, CWUM does not appreciably change the anatomical structure, however the recurrence rate is higher than CWDM because of the limited surgical view. In addition, a retraction pocket may develop if the Eustachian tube function is insufficient in CWUM [
1,
2]. To compensate for these disadvantages of CWDM, reconstruction of the posterior wall of the external auditory canal (EAC) and mastoid obliteration have been attempted, especially when the mastoid cavity volume is too large to prevent a cavity problem. In CWUM, obliterating the epitympanum and mastoid cavity is performed to prevent the retraction pockets [
2,
3].
Autografts, such as bone, cartilage, bone pate, abdominal fat, and musculoperiosteal flap have been used for a long time as the ideal materials of the graft for mastoid obliteration. However, each has disadvantages; the amount of cartilage or bone pate is insufficient, a large amount of fat is resorbed, and the length of the musculoperiosteal flap is short. Therefore, the mastoid cannot be obliterated completely and the obliteration materials gradually atrophies [
4,
5]. To compensate for these limitations, xenografts or artificial materials such as hydroxyapatite have been tried [
6].
β-Tricalcium phosphate and polyphosphate (β-TPP) is a novel artificial bone. It has been used in orthopedic surgery (e.g., artificial hip joint surgery, spine surgery), plastic surgery (e.g., craniofacial plastic surgery), and dental surgery (e.g., dental implant surgery), indicating its usefulness as a substitute bone graft material.
The aim of this prospective study was to analyze the treatment efficacy of mastoid obliteration using β-TPP after CWUM in patients who showed poor gas exchange ability but for whom CWDM was inappropriate. Additionally, its efficiency was also evaluated in animal models.
Go to :

DISCUSSION
CWUM is one of the surgical methods in COM patients that can maintain the original contour of the EAC. However, a retraction pocket may occur in patients who have poor Eustachian tube function due to negative pressure in the preserved air-reserved epitympanum and mastoid cavity. The more air-filled spaces there are, the greater the probability that a retraction pocket will occur [
1].
Mastoid obliteration is used to prevent cavity problems in patients with large mastoids during CWDM, and to prevent the occurrence of a retraction pocket in CWUM. Temporalis muscle, autologous cortical bone pate, cartilage, abdominal fat, alloplastic materials, and biosynthetic materials have been introduced for use in mastoid obliteration [
8-
12]. The most commonly used material is the musculoperiosteal flap, which is easily designed in the same operation field and has a good prognosis [
8,
9]. The musculoperiosteal flap including pedicled flaps that include the anteriorly based Palva flap, inferior based flap, and Rambo flap can be used for mastoid obliteration [
13-
15]. These flaps have an advantage of resistance to infection. However, resorption and contraction can occur postoperatively [
13-
16]. A donor site defect and difficulty in harvesting large volumes are additional problems. Various artificial materials are being used to compensate for the problems of autografts [
17-
20].
Hydroxyapatite (HA) is a bioinert, alloplastic material comprised of a calcium phosphate ceramic. It has been used as an ossicular prosthesis material or for reconstruction of the posterior EAC wall in the otologic field [
21]. As HA is a mineral matrix in bone tissue, it completely combines with bone tissue after being inserted in human bone. In one study, HA granules marketed as Bongros® (Bio@ Co., Seoul, Korea) were applied into the bulla of guinea pigs as a bone graft and there was successful substitution with normal new bone formation without inflammatory reaction or inner ear toxicity reported [
22]. In another study, bone formation was induced by HA implantation in the temporal dorsal bulla of guinea pigs without inflammation after 1 year and there was no recurrence in a cholesteatoma patient after mastoid obliteration with HA granules 2 years postoperatively [
23]. HA cement marketed as Mimix® (Walter Lorenz Surgical Inc, Jacksonville, FL, USA) has been used as a reconstruction material after the middle cranial fossa or posterior cranial fossa approach [
24]. However, complications such as delayed osseointegration failure, infection, and severe osteitis have been documented after performing mastoid obliteration using HA cement, despite complete coverage with fascia, flap, and skin [
25].
The PolyBone® used in this study is a new artificial bone comprised of β-TPP. It is available both in powder and granule form. PolyBone® contains an osteoinduction factor that stimulates the differentiation of osteoblasts and increases the expression of bone morphogenetic protein-4. The mechanism of stimulating bone formation involves participation of the polyphosphate in bone mineralization through the control of Ca concentration and pH in osteoblasts, which affects signal transduction to induce the stimulation of bone formation. In addition, PolyBone® has high biocompatibility without producing an inflammatory reaction. Synthetic materials with higher biocompatibility have been recently evaluated in animal experiments concerning orthopedic use. However, there have been few reports of the otologic clinical applicability of such materials [
2,
21,
26].
PolyBone® has lower strength, similar to that of cancellous bone. It has an advantage in bone union because the absorption rate of the implanted bone and the rate of bone growth closely corresponds. Therefore, PolyBone® is frequently used in posterior lumbar interbody fusion or posterolateral fusion in orthopedic surgery and neurosurgery [
27].
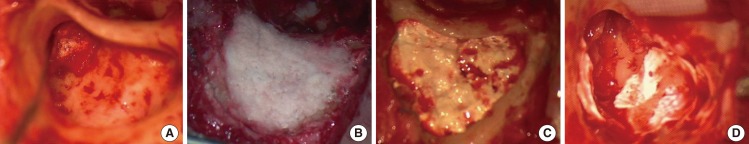
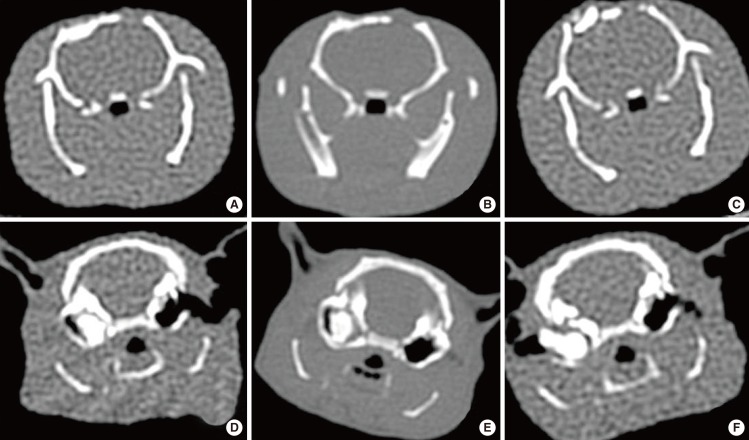
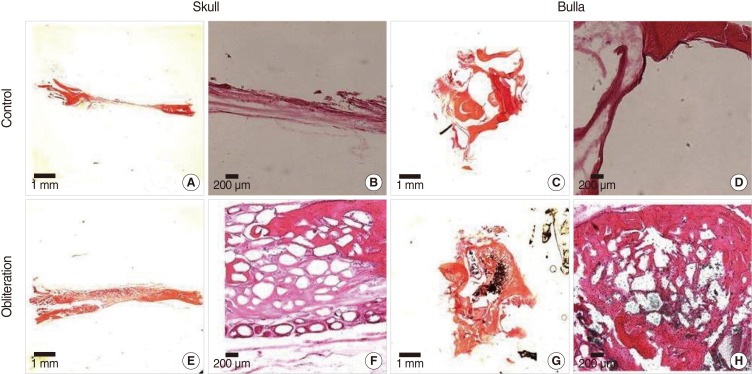
In one study, the granule type of PolyBone® was more effective than the powder type in the obliteration of bullae in guinea pigs [
28]. They commented that the granule type produced relatively low inflammatory reactions and obvious new bone formation with biodegraded graft materials. On the other hand, the powder type caused serious inflammatory reactions with unresolved materials until 20 weeks after obliteration. Despite these observations, the powder type of PolyBone® was applied to all 20 patients in this study, because the mastoid area is not subject to load and because obliteration is performed on the premise that inflammation had completely been removed. The authors considered that it is more important to completely obliterate the mastoid cavity to prevent a TM retraction caused by negative pressure than to induce osseointegration between new bone formation and degradable synthetic materials in a short time.
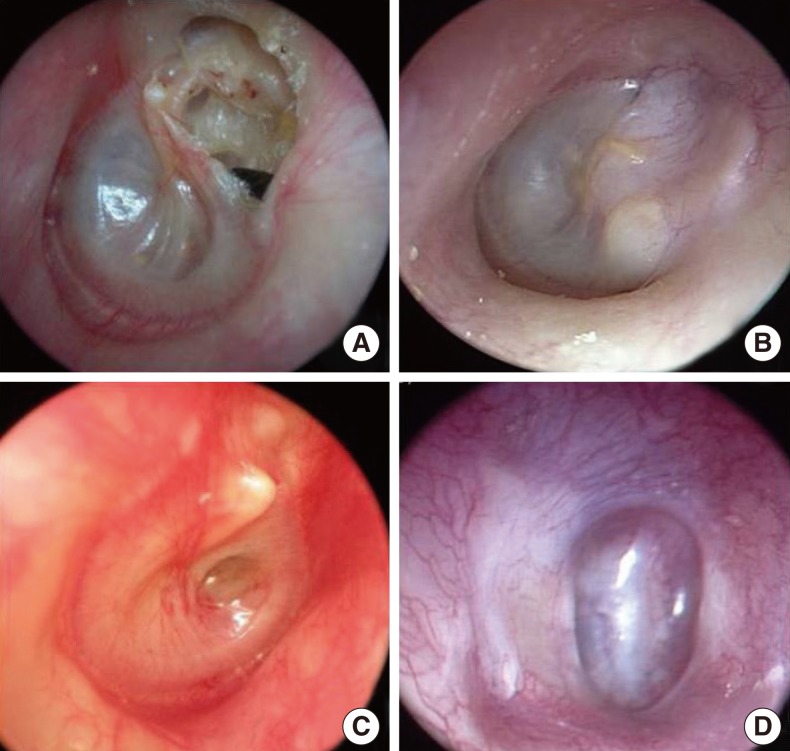
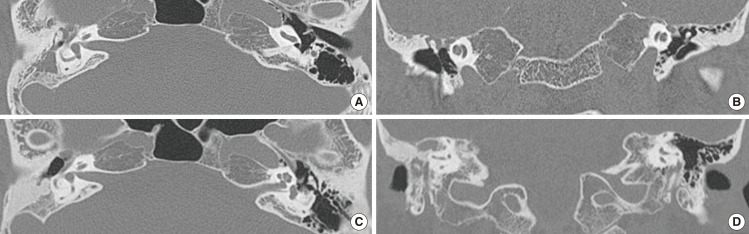
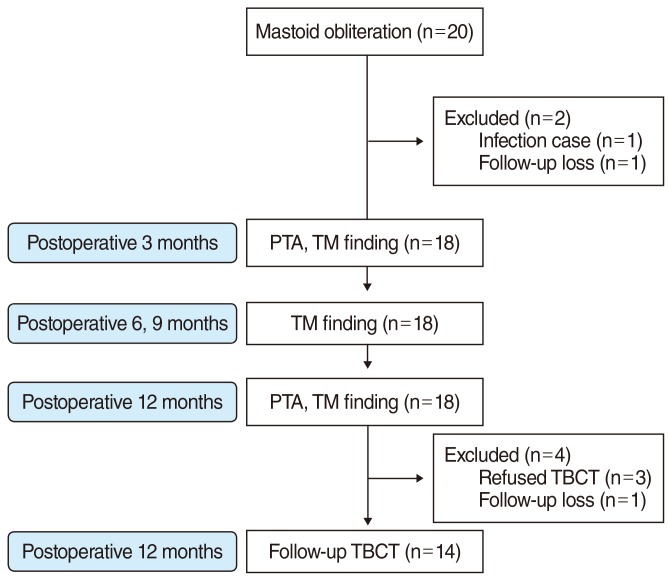
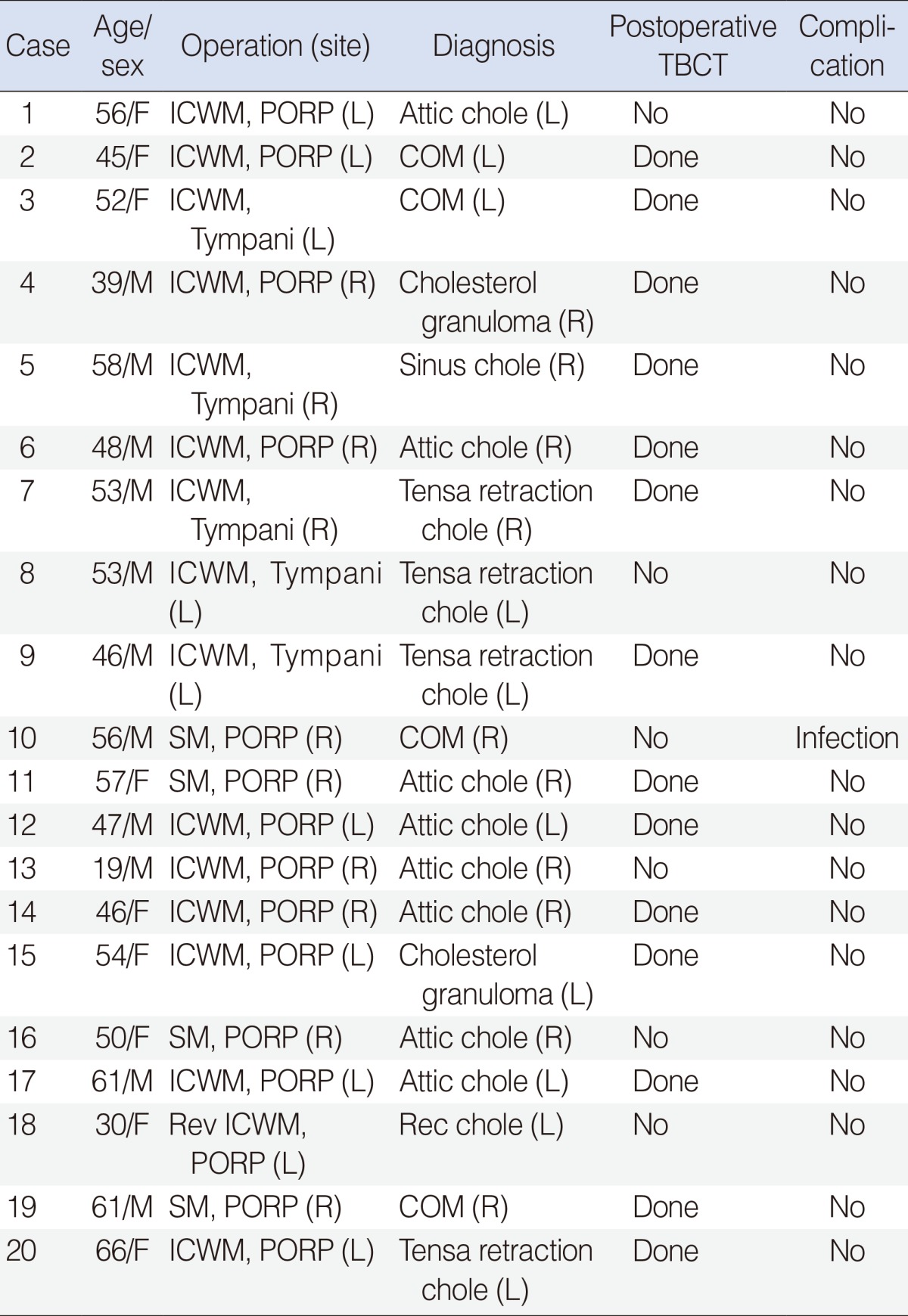
The purpose of mastoid obliteration after CWUM is to prevent the recurrence of a retraction pocket in patients who showed poor gas exchange ability. In this study, patients without a retracted TM preoperatively did not show a retracted TM postoperatively. Among the 15 cases which had a retracted TM preoperatively, 13 cases were followed-up. Eleven cases (73.3%) showed no retraction postoperatively. All fourteen TBCT obtained at 12 months after surgery demonstrated no bone resorption in obliterated mastoids. Pre- and postoperative hearing tests produced various results depending on whether ossiculoplasty had been performed or not. In the animal experiments, new bone formation was observed around obliterated PolyBone® without inflammatory cells and showed successful osseointegration.
PolyBone®, which was developed as a new biomaterial substitute for bone implantation, produces nearly no inflammatory reaction due to high biocompatibility. However, we confined candidates of mastoid obliteration with PolyBone® to patients without otorrhea and infection, due to the possibility of a foreign body reaction to alloplastic materials. During the operations, we collected an autologous bone pate from a non-inflammed mastoid cortex bone before a mastoidectomy. In all cases, we covered the autologous bone pate thoroughly over obliterated PolyBone® with care not to contact with patient's subcutaneous tissue to reduce the possibility of foreign body reaction. In one patient with complications, MRSA was isolated preoperatively from otorrhea culture. Mastoid obliteration using PolyBone® was performed, because no inflammatory sign was shown in intraoperative findings, except for a slightly wet middle ear mucosa. However, erythema and swelling occurred on postoperative day 5 and PolyBone® was removed on postoperative day 10. This experience highlights the importance of avoiding this technique in infected conditions, especially in a wound infected with antibiotic resistant bacteria. The remaining 19 patients have been followed-up in the outpatient clinic without postoperative complications, such as infection or foreign body reaction. However, surgeons must keep in mind the possibility of minor and major infection or foreign body reaction during performing mastoid obliteration with PolyBone®.
Mastoid obliteration is one of the effective options to prevent ear TM retraction after middle ear surgeries for patients with poor gas exchange ability. Although long-term follow-up data are needed, PolyBone® can be a relatively safe and effective material in mastoid obliteration in a COM operation when patients are accurately selected that have no inflammation or otorrhea, and by monitoring during the performance of the procedure to cover PolyBone® with an autologous bone pate to avoid exposure to surrounding subcutaneous soft tissue.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download