Abstract
A 53-year-old woman presented with left mandibular area pain, trismus, and facial numbness that had persisted for 4 years. Physical examination revealed a 3×5 cm, hard, non-tender, and round mass on the left mandibular area. Computed tomography and magnetic resonance imaging revealed an expansile tumor involving the left mandibular ramus and temporomandibular joint area with bone destruction, extending to the base of middle cranial fossa and left zygomatic bone. The mass at the segment of left mandible and zygomatic bone, and base of middle cranial fossa was removed. Pathological examination of the mass revealed a giant cell tumor. The defect was reconstructed with iliac bone for the mandible and temporal bone and fascia for the cranial bone and dura. The case is described along with a review of the literature.
Go to : 
Giant cell tumors (GCTs) are benign bone tumors arising from bone marrow, which account for about 5% of all biopsied primary bone tumors (1-3). GCTs arising in the head and neck region constitute approximately 2% of all GCTs, with the majority occurring in the sphenoid, ethmoid, or temporal bones (4, 5). To date, only a few reports of GCT arising from the craniofacial skeleton have been published, including from the parieto-occipital bones (6, 7), maxilla (8, 9), zygomatic bone (10, 11), and laryngeal cartilages (12). Only two studies have addressed treatment of the mandible giant cell tumors, especially with skull base extension (13, 14). We present a case of GCT arising from the mandible.
Go to : 
A 53-year-old female was referred to our head and neck cancer clinic for a mass lesion at the mandibular area. The patient presented with left mandibular area pain, trismus, and facial numbness that had persisted for 4 years. The patient had a medical history of osteoarthritis and osteoporosis. Physical examination revealed a 3×5 cm, hard, non-tender, and round mass on the left mandibular area. No other otorhinolaryngological and systemic abnormalities were evident.
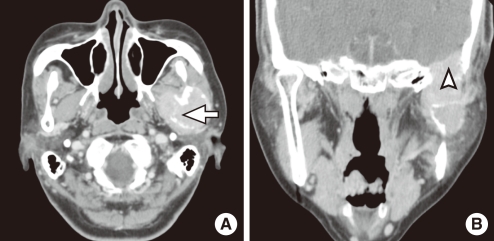
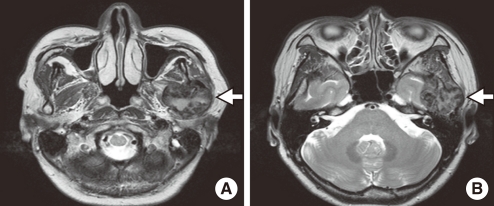
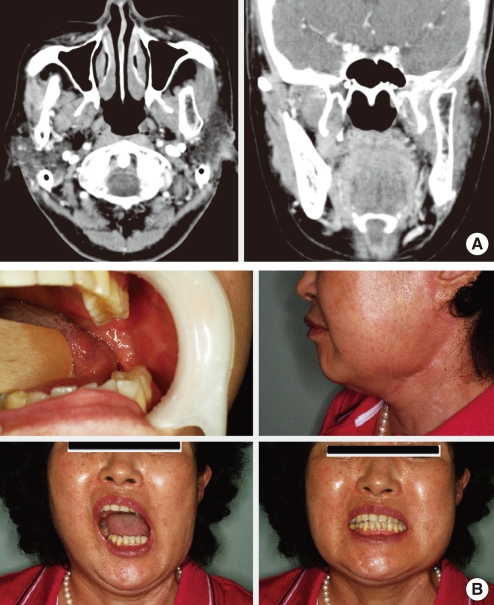
Computed tomography (CT) revealed an expansile tumor involving the left mandibular ramus and temporomandibular joint area with bone destruction, extending to the base of middle cranial fossa (Fig. 1). The tumor also extended to the left zygomatic bone. Magnetic resonance imaging (MRI) showed a 3×5 cm, heterogenous, well-defined, and expansile mass displacing the lateral pterygoid and temporalis muscle laterally, and involving the dura at the base of the middle cranial fossa (Fig. 2). On positron emission tomography-CT, elevated uptake of fludeoxyglucose was noted at the left masticator space, and no metastatic lesion was observed. We initially considered ameloblastoma, lymphoma, chondrosarcoma, and giant cell tumor. The patient did not undergo preoperative biopsy because an imaging study and preoperative biopsy including fine needle aspiration is often not sufficient for a diagnosis. Based on the clinical and radiographic criteria, this case was classified as an aggressive form (15). Therefore, we planned wide complete excision and reconstruction.
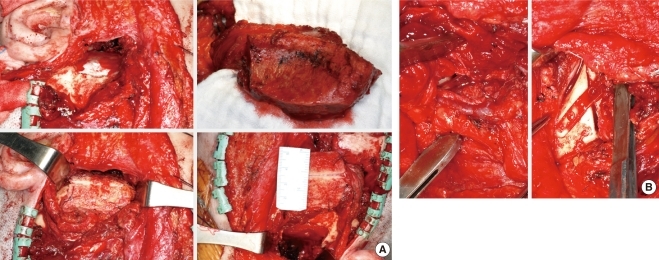
The patient underwent mass excision using a modified Blair and cervical incisions to preserve the parotid gland. The mass was resected with a segment of the left mandible and zygomatic bone (Fig. 3). The mass at the base of middle cranial fossa was also removed. The defect was reconstructed with iliac bone for mandible and temporal bone, and with fascia for cranial bone and dura (Fig. 4). No perioperative complications occurred.
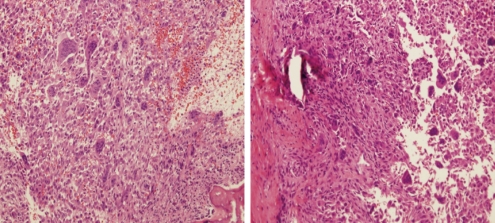
Microscopic examination revealed evenly distributed multinucleated giant cells with surrounding stroma made up of spindle cells. The giant cells displayed nucleoli that were similar to the surrounding spindle cells, suggestive of an osteoclastic type, which was consistent with a GCT (Fig. 5). The tumor involvement of the dura was confirmed and resection margins at the surrounding area were free.
During a 1-year serial clinical and radiological follow-up, there was no evidence of recurrence (Fig. 6). The facial contour and masticatory function was well-preserved, though lateralization of the mandible was observed on the opening of mouth due to pterygoid muscle injury.
Go to : 
GCT is a true neoplastic process originating from the undifferentiated mesenchymal cells of the bone marrow (10). It is generally considered as benign (6) but severe bony destruction may result occasionally depending on the location and clinical presentation of the tumor, making tumor management very challenging (9). GCTs are usually mono-ostotic, although they may occasionally present in a polyostotic form, which is usually of a high grade (16).
Patients with head and neck GCT may present with diverse symptoms depending on the location of primary lesion; symptoms include swelling, pain, epistaxis, neurological deficits, proptosis, visual defects, tinnitus, and hearing loss. In this case, GCT arising from the mandible caused temporo-mandibular pain and trismus.
Radiologic examination of GCT usually reveals a well-circumscribed lytic lesion surrounded by little or no sclerosis. The tumors may infrequently break through the cortex and invade the soft tissue or the articular space (4, 17). A CT scan can provide a detailed assessment of GCT, showing the soft tissue mass of the lesion, cortical perforation, amount of bony destruction, and extension toward important adjacent anatomic structures such as the cranial base (9). MRI is superior to CT in delineating the extent of soft tissue tumor because of its improved contrast resolution (9). Bone scintigraphy shows increased radionuclide uptake in the majority of GCTs (9).
The differential diagnosis of GCT includes aneurismal bone cyst, chondroblastoma, dermoid cyst, chondrosarcoma, giant cell reparative granuloma, and pigmented villonodular synovitis (4, 17). When an aggressive growth pattern is evident, the possibility of chondrosarcoma, osteosarcoma, and metastatic lesion cannot be ruled out until confirmation by histologic examination.
The final diagnosis is established only on the basis of a biopsy (5). Histologically, GCTs are composed of multinucleated giant cells in a vascular stroma of epitheloid or spindle-shaped mononuclear cells (18). The pathologic differential diagnosis of GCT is also extensive, including giant cell reparative granuloma, brown tumor of hyperparathyroidism, osteoblastoma, chondroblastoma, aneurismal bone cyst, non-ossifying fibroma, foreign body reaction, and osteosarcoma with abundant giant cells. These can be difficult to distinguish from one another, particularly at fine needle aspiration or with frozen section specimens (9).
Although it is regarded as benign, the giant cell tumor is locally aggressive, and can even metastasize to the lung (17). Malignant giant cell tumors have been reported (6), usually resulting from secondary malignant transformation after radiation treatment (19). They present with marked atypia and pleomorphism with mitotic activity and vascular invasion (20).
The treatment of choice of GCT is surgical excision (10). Regardless of the site of presentation, partial resection or curretage results in a recurrence rate of up to 70%, whereas recurrence after wide resection is about 7% (21). Radiotherapy is generally avoided and is reserved for GCTs that are considered inoperable, due to the risk of sarcomatous transformation (9), although some authors have advocated the use of radiotherapy in the management of GCT. Other treatment modalities including cryotherapy, chemotherapy, and curretage with adjuvant agents have been tried, but have yielded less effective results (10). GCTs generally recur within the first 3 years if recurrence occurs. But, continuous evaluation up to 5 years is recommended, since late distant metastasis have been reported (9).
After extended GCT resection, reconstruction of the defect is often required for functional and esthetical reasons. Osteoarticular autograft, allograft, and prosthetic reconstruction have been described (9, 22). A previous report suggested that the use of autologous tissue enables the rapid incorporation with a lower risk of infection, especially with vascularized grafts (9).
In conclusion, GCT arising from the mandible is a rare disease whose diagnosis is difficult. Imaging and preoperative biopsy including fine needle aspiration is often not sufficient to make the diagnosis. Therefore, the possibility of GCT should be included in the differential diagnosis of a bony lesion of craniofacial bones until a final diagnosis is made using a permanent pathologic specimen. Wide complete excision is required since incomplete excision results in a high incidence of recurrence.
Go to : 
References
1. Dahlin DC, Cupps RE, Johnson EW Jr. Giant-cell tumor: a study of 195 cases. Cancer. 1970; 5. 25(5):1061–1070. PMID: 4910256.

2. Marcove RC, Lyden JP, Huvos AG, Bullough PB. Proceedings: Giant cell tumors treated by cryosurgery: an analysis of 25 cases. Proc Natl Cancer Conf. 1972; 7:951–957. PMID: 4764952.
3. Marcove RC, Lyden JP, Huvos AG, Bullough PB. Giant-cell tumors treated by cryosurgery: a report of twenty-five cases. J Bone Joint Surg Am. 1973; 12. 55(8):1633–1644. PMID: 4804985.
4. Saleh EA, Taibah AK, Naguib M, Aristegui M, Vassallo G, Landolfi M, et al. Giant cell tumor of the lateral skull base: a case report. Otolaryngol Head Neck Surg. 1994; 9. 111(3 Pt 1):314–318. PMID: 8084641.

5. Rosenbloom JS, Storper IS, Aviv JE, Hacein-Bey L, Bruce JN. Giant cell tumors of the jugular foramen. Am J Otolaryngol. 1999; May-Jun. 20(3):176–179. PMID: 10326755.

6. Leonard J, Gökden M, Kyriakos M, Derdeyn CP, Rich KM. Malignant giant-cell tumor of the parietal bone: case report and review of the literature. Neurosurgery. 2001; 2. 48(2):424–429. PMID: 11220389.

7. Harris AE, Beckner ME, Barnes L, Kassam A, Horowitz M. Giant cell tumor of the skull: a case report and review of the literature. Surg Neurol. 2004; 3. 61(3):274–277. PMID: 14985001.

8. Mooney WW, Bridger GP, Baldwin M, Donellan M. Recurrent giant cell tumour of the maxilla associated with both Paget's disease and primary hyperparathyroidism. ANZ J Surg. 2003; 10. 73(10):863–864. PMID: 14525586.
9. Marioni G, Marchese-Ragona R, Guarda-Nardini L, Stramare R, Tognazza E, Marino F, et al. Giant cell tumour (central giant cell lesion) of the maxilla. Acta Otolaryngol. 2006; 7. 126(7):779–781. PMID: 16803721.

10. Sethi A, Passey JC, Mrig S, Sareen D, Sharma P. Giant cell tumour (osteoclastoma) of the zygoma: an extremely unusual neoplasm. Acta Otolaryngol. 2006; 3. 126(3):327–329. PMID: 16618665.

11. Muszynski P, Modrzejewski M, Kotarba E. Osteoclastoma of temporal and zygomatic bone. Otolaryngol Pol. 1995; 49(4):324–328. PMID: 8532351.
12. Wieneke JA, Gannon FH, Heffner DK, Thompson LD. Giant cell tumor of the larynx: a clinicopathologic series of eight cases and a review of the literature. Mod Pathol. 2001; 12. 14(12):1209–1215. PMID: 11743042.

13. Hamlin WB, Lund PK. "Giant cell tumors" of the mandible and facial bones. Arch Otolaryngol. 1967; 12. 86(6):658–665. PMID: 6058414.

14. Kang SH, Kim HJ, Cha IH, Nam W. Mandibular condyle and infratemporal fossa reconstruction using vascularised iliac crest and vascularised calvarial bone graft. J Plast Reconstr Aesthet Surg. 2008; 12. 61(12):1561–1562. PMID: 18707927.

15. Dewsnup NC, Susarla SM, Abulikemu M, Faquin WC, Kaban LB, August M. Immunohistochemical evaluation of giant cell tumors of the jaws using CD34 density analysis. J Oral Maxillofac Surg. 2008; 5. 66(5):928–933. PMID: 18423282.

16. Sanghvi V, Lala M, Desai S, Chaturvedi P, Rodrigues G. Synchronous multicentric giant cell tumour: a case report with review of literature. Eur J Surg Oncol. 1999; 12. 25(6):636–637. PMID: 10556015.

17. Silvers AR, Som PM, Brandwein M, Chong JL, Shah D. The role of imaging in the diagnosis of giant cell tumor of the skull base. AJNR Am J Neuroradiol. 1996; 8. 17(7):1392–1395. PMID: 8871731.
18. Mafee MF, Yang G, Tseng A, Keiler L, Andrus K. Fibro-osseous and giant cell lesions, including brown tumor of the mandible, maxilla, and other craniofacial bones. Neuroimaging Clin N Am. 2003; 8. 13(3):525–540. PMID: 14631689.

19. Goldenberg RR, Campbell CJ, Bonfiglio M. Giant-cell tumor of bone. An analysis of two hundred and eighteen cases. J Bone Joint Surg Am. 1970; 6. 52(4):619–664. PMID: 5479455.
20. Icihikawa K, Tanino R. Soft tissue giant cell tumor of low malignant potential. Tokai J Exp Clin Med. 2004; 9. 29(3):91–95. PMID: 15595466.
21. Murphey MD, Nomikos GC, Flemming DJ, Gannon FH, Temple HT, Kransdorf MJ. From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: radiologic-pathologic correlation. Radiographics. 2001; Sep-Oct. 21(5):1283–1309. PMID: 11553835.
22. Kocher MS, Gebhardt MC, Mankin HJ. Reconstruction of the distal aspect of the radius with use of an osteoarticular allograft after excision of a skeletal tumor. J Bone Joint Surg Am. 1998; 3. 80(3):407–419. PMID: 9531209.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download