This article has been
cited by other articles in ScienceCentral.
Abstract
A serious midface defect involving resection of squamous cell carcinoma originating from the hard palate was treated by an unusual reconstructive strategy. After tumor resection, surgical reconstruction was accomplished in one stage using one free flap with one distant and local flap: a radial forearm flap to reconstruct the upper lip, a forehead flap to reconstruct the external nose, a cantilever calvarial bone graft to replace the nasal skeleton and a nasolabial flap and split thickness skin graft to cover the internal nasal lining. The rationale for this one-stage reconstruction and the problems associated with midfacial reconstruction after wide tumor excision are discussed.
Go to :

Keywords: Surgical flaps, Midface, Radical tumor resection
INTRODUCTION
Midfacial defects caused by radical tumor surgery or trauma involve various structures, such as the palate, teeth, nasal cavity and maxillary sinus (
1). The unique anatomy of the midface with its aesthetic and functional importance makes its reconstruction challenging. How it should be done remains a matter of debate. Although the reconstructive option depends on the extent of the bony and soft tissue defect, various pedicled and free tissue transfer techniques with and without bone grafts have been used (
2-
5). Midfacial reconstruction using multiple free flaps has more advantages than a prosthesis or osseointegrated implants, and staged reconstruction has been recommended (
5). However, vascularized or local flaps are not always viable options due to the amount of missing tissue and nasomaxillary defects need prosthetical reconstruction to enhance their oral function and aesthetics (
6). This report presents a case of surgical reconstruction in a patient with a large midfacial defect after radical tumor resection. The problems associated with midfacial and oral cavity reconstruction are discussed.
Go to :

CASE REPORT
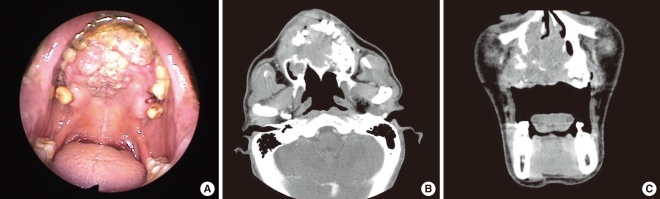
A 54-year-old man was referred to the Otolaryngology Department of Chung-Ang University College of Medicine due to nasal obstruction and a known intranasal mass. A huge necrotic mass protruded to the upper gingiva and the mucosal surface of the upper lip. Tumor invasion to the hard palate and upper teeth from right third molar to left first molar was observed (
Fig. 1A). Paranasal sinus computed tomography (CT) revealed that the primary mass arose in the right hard palate and invaded across the opposite palate, and extended into the bilateral upper gingiva, nasal cavity and nasal septum. The destruction of the anterior side of right maxilla was also detected and the tumor protruded onto the subcutaneous tissue of the anterior maxillary wall (
Fig. 1B, C). Posterior portions of the right inferior turbinate and nasal septum were intact. An intranasal biopsy was performed and the pathologic report revealed squamous cell carcinoma. There was no evidence of distant metastasis or enlargement of the cervical lymph node.
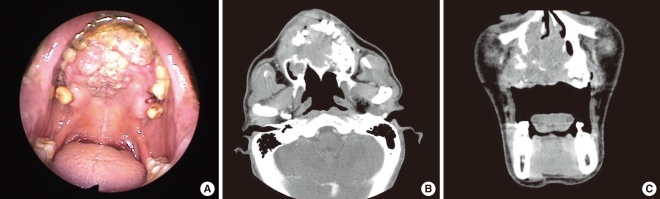 | Fig. 1Preoperative view and paranasal sinus computed tomography (CT) of the patient with squamous cell carcinoma, originated from hard palate. (A) Endoscopic findings showing the mass destroying the hard palate and protruding into the oral cavity. Axial (B) and coronal CT (C) scans showing the lesion arising from the hard palate, filling the anterior nasal cavity and extending into both maxilla and gingiva. 
|
Surgical technique and clinical sourse
Radical tumor resection (clinical stage T
4aN
0M
0), including composite bilateral infrastructure maxillectomy, total rhinectomy, near total upper lip resection and total hard palatectomy was performed (
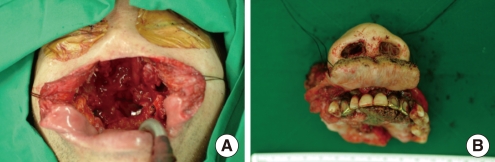
Fig. 2). After tumor resection, surgical reconstruction was accomplished by the plastic and reconstructive surgeon. The operative plan was based on the simultaneous transfer of one free flap with one distant and local flap, and immediate placement of a temporary palatal surgical obturator in one stage: a radial forearm flap to reconstruct the upper lip, a forehead flap to reconstruct the external nose, a cantilever calvarial bone graft to replace the nasal skeleton, a nasolabial flap and split thickness skin graft to cover the internal nasal lining and a palatal surgical obturator to substitute the hard palate temporarily. The surgical procedures were as follows. Firstly, a temporary obturator, which was made preoperatively by a dentist, was secured with stainless steel wires to both sides of the pterygoid plates for palatal reconstruction. Secondly, a 6×6 cm radial forearm free flap was harvested and transferred to the missing upper lip area. The proximal ends of the radial artery and two venae commitantes were anastomosed to the facial artery, submental and facial vein. Thirdly, a 6×1 cm calvarial bone was harvested from the left parietal bone and anchored with two screws to the remnant nasal bone as a cantilever bone graft. The inner side of the calvarial bone graft was covered with a single nasolabial flap from the left cheek. Lastly, a forehead gull-wing flap was elevated for total nasal coverage and the inner side was covered with split-thickness skin graft. Then, the forehead gull-wing flap was inserted to the reconstructed upper lip and palatal obturator (
Fig. 3). Pedicle division and final revisions, including a full-thickness skin graft to the forehead flap donor site, were performed 4 weeks later (
Fig. 4A) Postoperative radiotherapy was carried out with 7,000 cGY on the primary lesion and the patient made an uncomplicated recovery (
Fig. 4B). Two years following surgery, the patient had no evidence of recurrent disease.
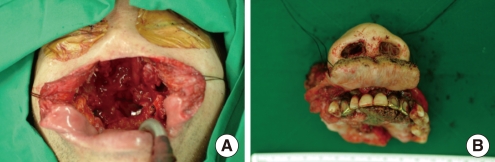 | Fig. 2Intraoperative view of the surgical procedure. (A) Operative view of midfacial defect after composite bilateral infrastructure maxillectomy, total rhinectomy, near total upper lip resection and total hard palatectomy. (B) A photograph showing the specimen, including primary tumor after surgical resection. 
|
 | Fig. 3Immediate postoperative view of patient. The midface defect was reconstructed with a radial forearm free flap to reconstruct the upper lip, a forehead flap to reconstruct the external nose, a cantilever calvarial bone graft to replace the nasal skeleton and a nasolabial flap and split thickness skin graft to cover the internal nasal lining. 
|
 | Fig. 4Postoperative views of the patient. (A) Postoperative view at 4 weeks after reconstruction. (B) Postoperative view at 9 weeks after reconstruction. 
|
Go to :

DISCUSSION
Complex head and neck defects are seen in patients having oncologic resection or trauma and often demand composite reconstruction of mucosal lining, skeletal support, soft tissue and skin coverage (
7-
9). Furthermore, midfacial defects, including both the perioral and nasomaxillar areas are not common and are more difficult to reconstruct because of complex multidimensional characteristics of the area. There are several options that can be applied to those extensive defects, such as prosthetic devices, osseointegrated implants, pedicled flaps with the aid of autologous or alloplastic grafts and microvascular free flaps (
8,
9). Staged procedures have been more useful for midfacial reconstruction using a prosthetic device, distant flap, and one or multiple autologous free flaps (
5,
9). However, these staged techniques require a prolonged operation time and may cause serious problems, such as wound infection, psychiatric problems, scarring from a nonfunctional upper lip, contraction of free flaps and weak support of palate. In one report, three free flaps were used to reconstruct the middle and lower facial defect in one-stage, which provided better aesthetic and functional outcomes, resulting in prevention of contraction of the remaining facial soft tissues (
6).
In the present case, we decided on a one-stage surgical reconstruction after en-bloc tumor resection and performed the combined reconstructive method in our patient with a massive midfacial defect. For the large nasal defect, we used a full-thickness forehead rotational flap including a calvarial bone graft for the caudal portion of nasal skeleton. For the defect in both upper cheeks, we used the radial forearm free flap. For the defect of the hard palate, we planned to use a composite graft. However, we could not find an adequate donor site for graft with a good blood supply due to the patient's long history of smoking. Lastly, we applied a temporary prosthesis instead of a composite graft. We intended to replace the temporary obturator by a permanent one, but a long-term follow-up of the patient did not occur. Nevertheless, we found that temporary obturator preserved its structural support during the available follow-up period, even after radiotherapy. The maintenance of structural support by a temporary prosthesis during a long-lasting step-wise therapy after large maxillectomy has been reported (
10). We found that both the microvascular and pedicled flaps associated with the prosthetic device were resistant to radiotherapy and that a one-stage midfacial defect reconstruction including the nose, hard palate, and upper lip, using those flaps was versatile, comparing with multiple microsurgical free flaps or staged surgical reconstruction.
The presently-reported reconstructive procedure using a distant free flap, local flap and obturator is not an absolute operative option for reconstruction of extensive midfacial defects. In particular, a viable flap may be preferable to an obturator, considering the postoperative function of the oropharynx. However, we conclude that a one-stage reconstruction can be an effective and alternative method for total nose, hard palate and upper lip reconstruction, even if surgical options are variable.
Go to :






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download