This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
To evaluate the usefulness of silicone blocks as graft material for mastoid cavity obliteration in the prevention of problematic mastoid cavities after canal wall down mastoidectomies.
Methods
Retrospective evaluation of 20 patients who underwent mastoid obliteration with silicone blocks between 2002 and 2009 at the Chonnam National University Hospital. The cases consisted of 17 patients with chronic otitis media with cholesteatoma and 3 patients with adhesive otitis media. The postoperative follow-up period was an average 49 months (range, 6 to 90 months). The surgical technique used at our institution composed four major steps: First, the canal wall down mastoidectomy was performed and the middle ear procedure was completed. The silicone blocks were used to fill up the mastoidectomized cavity. Then, a cortical bone pate was used to cover the surface of the silicone blocks. Finally, temporalis fascia and a split musculoperiosteal flap were used to surround the bone pate for reinforcement of the reconstructed canal wall. We examined postoperative success rate and hearing outcomes.
Results
In 19 cases (95%), the reconstructed canal wall maintained a cylindrical shape and the ear drum healed without perforation. In only 1 case (5%), the reconstructed canal wall was destroyed with ear drum perforation. The mean improvement in air-bone gap was about 12 dB (P<0.05), and the mean improvement in air-conduction was about 16 dB (P<0.05).
Conclusion
We suggest that silicone blocks could be valuable resources as graft materials for mastoid obliteration after canal wall down mastoidectomies.
Go to :

Keywords: Cholesteatoma, Silicones, Mastoid, Reconstructive surgical procedures
INTRODUCTION
A canal wall down tympanomastoidectomy is a very effective technique for eradication of advanced chronic otitis media or cholesteatomas. The advantages of canal wall down mastoidectomy include excellent exposure for disease eradication and postoperative monitoring, and low rates of residual and recurrent disease. However, the disadvantages of canal wall down mastoidectomy include cavity problems, such as continuous ear drainage, accumulation of keratin debris, frequent vertigo attacks following temperature or pressure changes, and difficulty in fitting a hearing aid (
1,
2). In addition, the final hearing gained after staged ossiculoplasties in patients who have undergone canal wall down mastoidectomies is usually 5-10 dB worse than patients who underwent canal wall up tympanomastoidectomy due to ineffective sound transmission (
3,
4). Thus, to overcome cavity problems, many reports about the mastoid obliteration technique have been introduced. Materials used to fill the cavity include several kinds of muscle flap (
5), cortical bone pate (
6,
7), allogenous/autogenous bone chips, cartilage (
7,
8), and hydroxyapatite (
9). However, all of the techniques have advantages and disadvantages. Herein, we introduce silicone blocks for mastoid obliteration materials. Silicone blocks are flexible enough to handle and to fit into cavities of variable size, and rigid enough to prevent collapse in the mastoid. Also, silicone blocks are much cheaper than other alloplastic materials.
Go to :

MATERIALS AND METHODS
Patients
A retrospective review of patient records was performed on a consecutive series of 20 patients who underwent canal wall down tympanomastoidectomies and mastoid obliteration with silicone block for treatment of chronic otitis media with cholesteatoma and adhesive otitis media over a 7-year period (2002-2009). This study was approved by institutional review board (IRB) of our hospital.
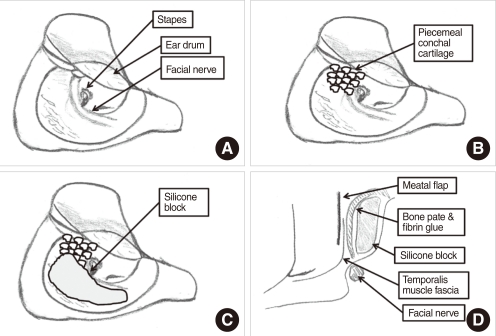
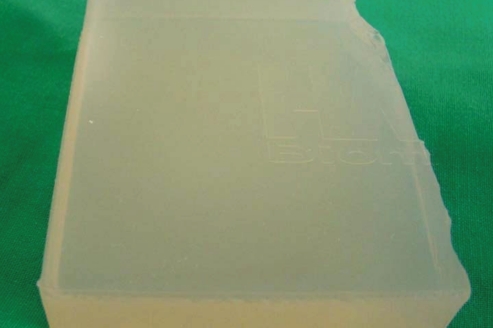
Silicone preparation
We cut the silicone (Hansbiomed Co., Daejeon, Korea) (
Fig. 1) into small pieces ranging from 2-4 mm in size (group A) and 15-20 mm (group B), and henceforth referred to as silicone blocks.
 | Fig. 1Silicone (Hansbiomed Co., Daejeon, Korea) is soft enough to be cut by scarpel and easy to be designed, but solid enough to exist in the mastoid lifelong. 
|
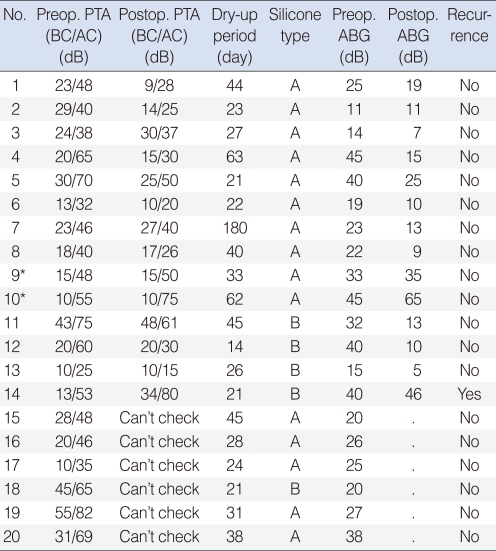
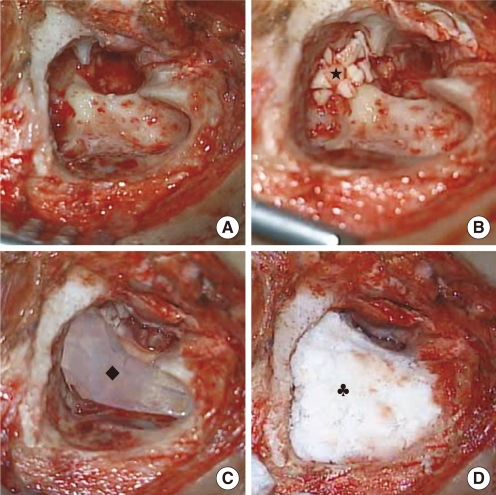
Surgical technique
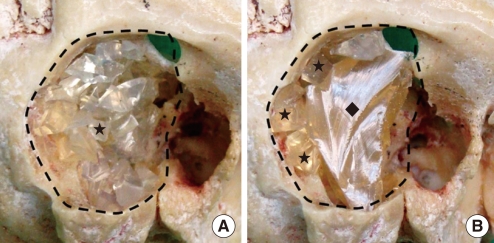
First, we performed a conventional post-auricular skin incision and elevated the anterior-based musculoperiosteal flap. Then, we harvested the temporalis fascia and elevated the posterior meatal skin flap. Healthy cortical bone pate was collected using a specially designed suction line, including a bone dust filter. Canal wall down mastoidectomy was performed and we removed all pathologic lesions within the mastoid and middle ear cavities (
Figs. 2A,
3A). Cartilage was harvested from the cymba portion of the concha cartilage, and cut into small pieces ranging from 1-3 mm in size. The obtained piecemeal cartilage was usually just sufficient to allow complete obliteration of the epitympanic space to re-create the annulus superiorly to the same lateral level as the facial ridge below (
Figs. 2B,
3B). It is at this point that the new technique differs from other techniques. Silicone blocks were used to obliterate the mastoid cavity in the perilabyrinthine and retrofacial areas and form a smooth contour lateral to the facial ridge (
Figs. 2C,
3C). Group A only used piecemeal silicone blocks (
Fig. 4A), while group B used large silicone blocks and supplied the deficiency with piecemeal silicone blocks (
Fig. 4B). The blocks were fixed using fibrin-based adhesive (Green-plast; Green-Cross, Seoul, Korea). The silicone blocks were then covered with the previously harvested cortical bone pate and temporalis fascia was used to enclose the bone pate (
Figs. 2D,
3D). The anterior-based musculoperiosteal flap was split into a muscle and a periosteal layer. We then placed the periosteal layer between the fascia and bone pate for strengthening the reconstructed external auritory canal. The postauricular wound was closed in the standard fashion.
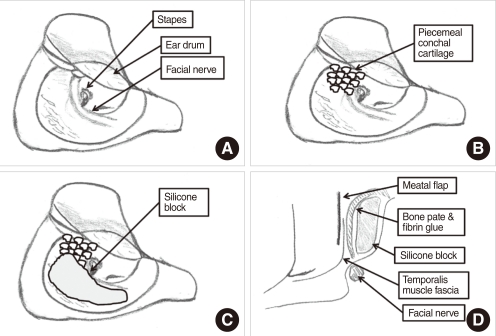 | Fig. 2Schematic figures of operating technique. (A) A canal wall down mastoidectomy is performed for removing of diseases. (B) The epitympanic cavity is obliterated with piecemeal cartilage. (C) Mastoid cavity is obliterated with silicone blocks. (D) Coronal view. Silicone blocks are covered with bone pate and temporalis muscle fascia. 
|
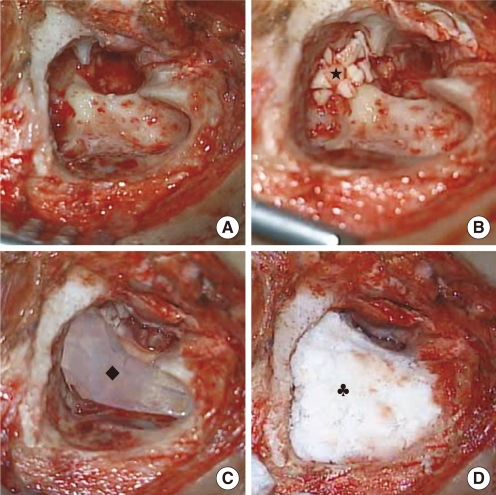 | Fig. 3Surgical procedures for mastoid obliteration with silicone blocks and bone pate. (A) After elevation of the anterior-based flap, a canal wall down mastoidectomy is performed. (B) The epitympanic cavity is obliterated with piecemeal cartilage. (C) Silicone blocks are used to fill the mastoid cavity. (D) Silicone blocks are fixed using fibrin glue and covered with bone pate. ★, piecemeal conchal cartilage; ◆, silicone block; ♣, bone pate. 
|
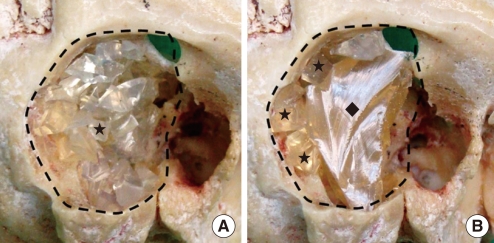 | Fig. 4Group A, mastoid obliteration with piecemeal silicone blocks and filling with bone pate. Group B, mastoid obliteration with large silicone block and supplying the deficiency with piecemeal silicone blocks and bone pate. Dotted line, mastoid cavity; ★, piecemeal silicone blocks; ◆, large silicone block. 
|
Audiologic evaluation
The audiometric evaluation included pre- and postoperative air-bone gap (ABG), air-conduction thresholds (AC) and bone-conduction thresholds (BC). The hearing threshold (dB) was calculated as the mean value of the threshold for 500, 1,000, 2,000, and 4,000 Hz. Paired-samples t-test was used for comparison of the pre- and postoperative air conduction hearing thresholds and ABGs. A P<0.05 was accepted as statistically significant.
Go to :

RESULTS
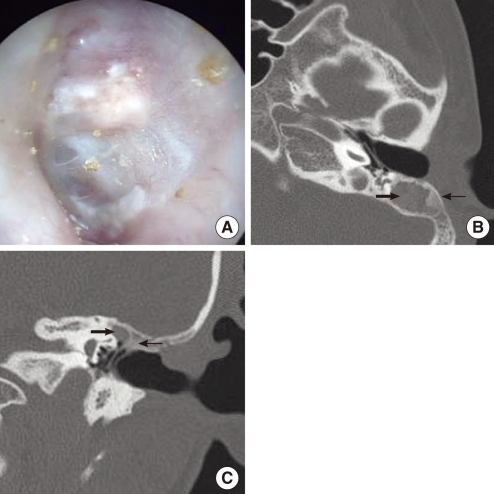
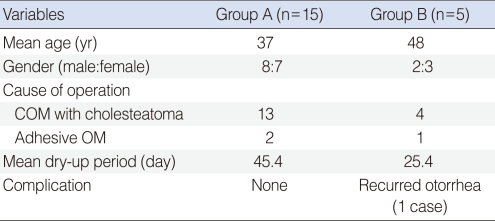
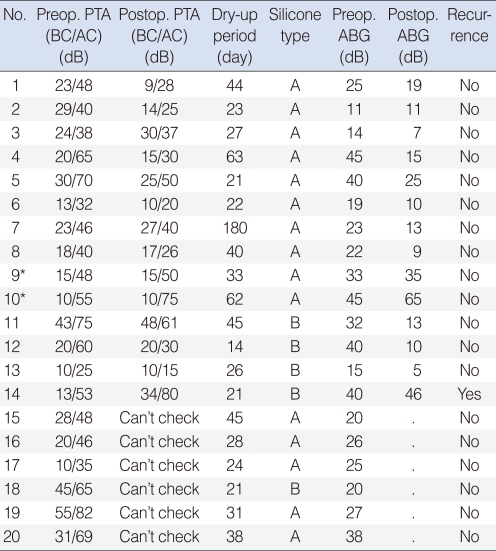
Twenty patients underwent mastoid obliteration using silicone blocks and cortical bone pate between 2002 and 2009. Ten patients were male and ten were female. The average age of the patients was 39.8 years (range, 9 to 62 years). The length of follow-up ranged from 6 to 90 months (average, 49 months). Fifteen patients used piecemeal silicone blocks (group A) and five patients used large silicone blocks (group B) (
Table 1). All patients in group A had dry ears with good canal contour at the time of chart review (
Fig. 5). In group B, one patient with chronic otitis media with cholesteatoma was considered a failure because of otorrhea and ear drum perforation with a destructed posterior ear canal 37 months later after operation. During the revision operation, the silicone blocks and granulation tissue were removed. A revision canal wall down mastoidectomy and tympanoplasty type III was performed; postoperatively the ear drum was dry and healthy. Thus, the method used in group B give rise to more complications than group A. However, statistical analysis was not performed because the number of group B patient was so small. The mean dry up period was 40.4 days. We performed postoperative pure tone audiograms in 14 patients. With the exception of 1 patient with disease recurrence and 2 patients with planned 2nd look operations, the postoperative air-bone gap decreased to <25 dB. The mean improvement in air-bone gap was about 12 dB (
P<0.05), and the mean improvement in air-conduction was about 16 dB (
P<0.05) (
Table 2).
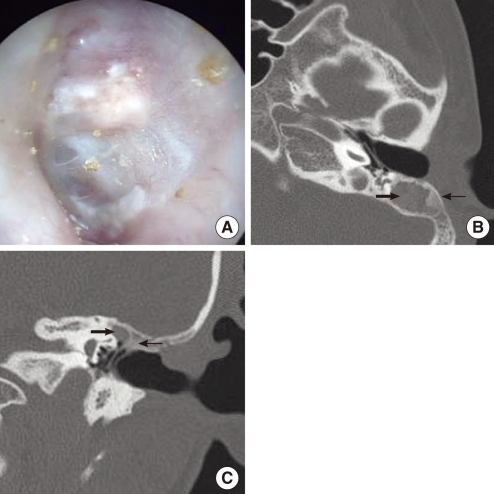 | Fig. 5Postoperative findings after mastoid obliteration (7 months after surgery). (A) Photograph of drum and external auditory canal. Reconstructed posterior wall is well maintained. (B, C) Axial and coronal temporal bone CT scan. The mastoid cavity is well obliterated by the silicone blocks (thick arrow) and bone pate (thin arrow). 
|
Table 1
Demographic data for both groups
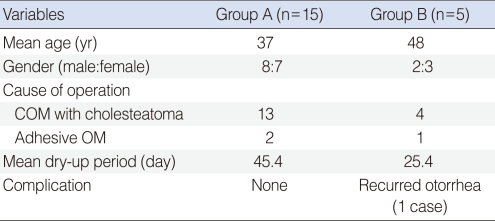

Table 2
Clinical and audiologic features of patients who underwent mastoid obliteration with silicone blocks

Go to :

DISCUSSION
The management of chronic ear disease occasionally requires canal wall down mastoidectomy for appropriate surgical management. However, there are some complications with canal wall down mastoidectomy, such as delayed healing of the wound, chronic ear drainage, and an inadequate canal contour for a hearing aid. Otologists have recognized these problems more than 100 years ago, and tried to develop techniques and materials for mastoid obliteration. A number of materials, both biological and alloplastic, have been used for mastoid obliteration (
10-
15). Each of the techniques has advantages and disadvantages. Biological materials, including fat, cartilage, bone and various flaps, are resistant to infection, but have the disadvantage of resorption, atrophy, curvature, difficulty in fashioning, and donor site morbidity. Alloplastic materials, including hydroxyapatite, have the advantages of being readily available, no resorption, and no donor site morbidity; however, hydroxyapatite has been associated with the risk of infection and exposure (
16). Based on these advantages and disadvantages, we consider silicone blocks with bone pate and musculoperiosteal flaps to be useful materials in mastoid obliteration.
Many reports have already concluded that silicone materials are safe because there is no evidence of an immunotoxic response (
17). Thus, silicone is widely used as a medical device, such as CSF shunts, IV tubing, arthroplasty prostheses, cardiac valves, intraocular lens implants, and rhinoplasty implants. In otologic surgery, silicone sheeting, ventilation tubes, cochlear implants and silicone ossiculoplasty prostheses are used.
In our study, 19 patients had a dry canal and good contour on their regular return visit. One patient in group B had otorrhea and ear drum rupture with a destructed posterior ear canal 37 months after the operation. We considered the reason for failure was infection of the bone pate. We performed a revision procedure and removed the silicone blocks. Currently, the ear is dry and clean. As a preliminary clinical report, our results indicate that silicone blocks with a bone pate and musculoperiosteal flap are likely to be useful for mastoid obliteration. As with any graft material for mastoid obliteration, long-term follow-up and additional case review will be necessary to evaluate the stability of the material over a prolonged period of time. A prospective case-control study is needed.
Based on these results, piecemeal silicone blocks with a bone pate and musculoperiosteal flap appears to be very effective for mastoid obliteration. The coverage of the bone pate by a split musculoperiosteal flap appears to prevent infection of the bone pate and exposure of the silicone blocks. We suggest that silicone blocks could be one of valuable resources as graft materials for mastoid obliteration after canal wall down mastoidectomies.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download