Abstract
Pulsatile tinnitus is tinnitus that coincides with the patient's heartbeat. It constitutes a small portion of all tinnitus, but it is often the first or sole manifestation of a serious disease in the nervous system. Aneurysm of the internal carotid artery is known as a rare cause of pulsatile tinnitus and, in the main, aneurysms of the petrous portion have been reported as a cause of pulsatile tinnitus. We present an interesting case of pulsatile tinnitus that was caused by a paraclinoid aneurysm in this report and discuss clinical features and treatment of paraclinoid aneurysm.
Pulsatile tinnitus is almost always the result of the sound of non-laminar blood flow that is transmitted to the inner ear [1]. This can occur in systemic disease causing a general alteration in the hemodynamics or in local disorders that are anatomically close to or within the petrous bone [1]. The most common local causes of pulsatile tinnitus include a high jugular bulb, atherosclerosis of the carotid artery, and a dural arteriovenous fistula [1, 2]. Aneurysm of the internal carotid artery (ICA) is a rare cause of pulsatile tinnitus and, in the main, aneurysms of the petrous portion of the ICA have been reported as a cause of pulsatile tinnitus in the literature [3-5].
Recently, we experienced a very interesting case of pulsatile tinnitus that was caused by an aneurysm of the paraclinoid portion of the ICA, and successfully treated her with endovascular embolization.
A 54-year-old woman visited our tinnitus clinic because of pulsatile tinnitus on the right side or inside her head for several years. She had taken hypertension medicine for 5 years, but her blood pressure was well controlled and she denied any trauma history to her neck or head. On physical examination, her tympanic membrane and external auditory canal showed normal appearance, and she did not present any neurological signs. Her tinnitus could not be auscultated around the neck and auricle, and did not disappear after putting digital pressure on her neck. Audiologic examination showed mild sensorineural hearing loss of high-pitched tones on both sides.
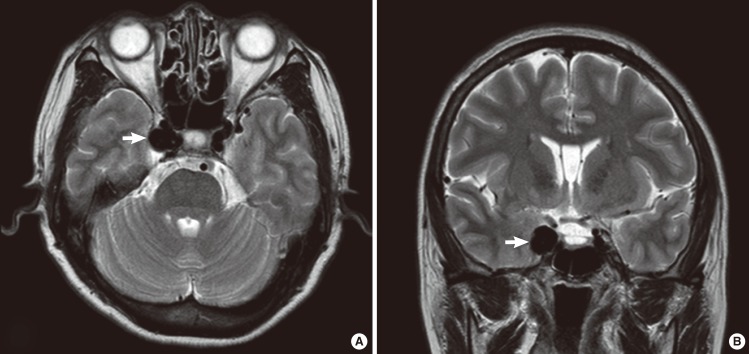
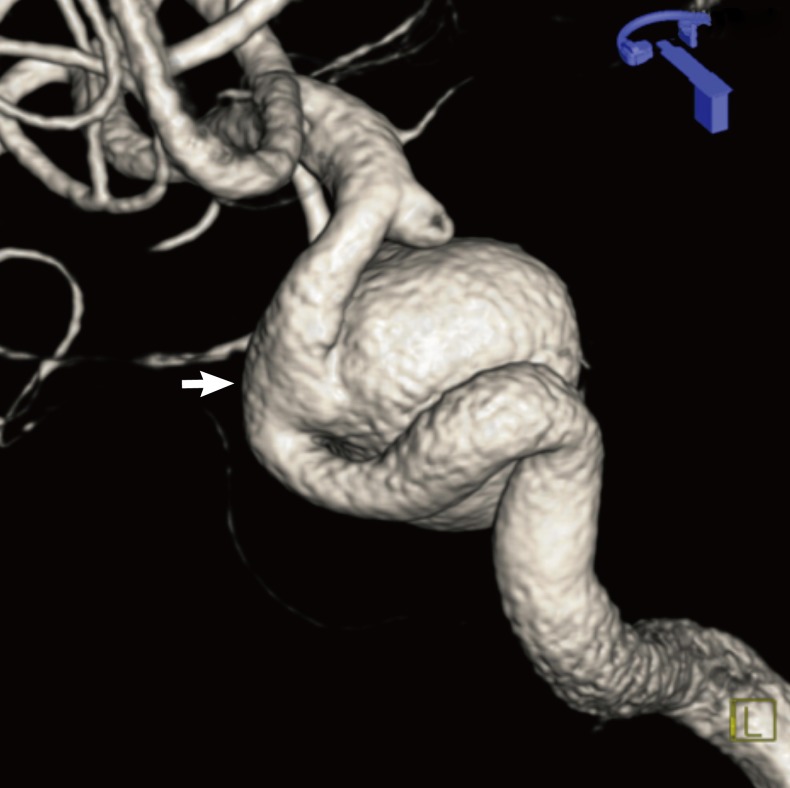
On imaging study, temporal bone computed tomography (CT) looked normal, but her brain magnetic resonance imaging (MRI) showed a 1.4-cm signal void in the paraclinoid region of the right ICA (Fig. 1). For further evaluation, intra-arterial angiography was performed and confirmed a large saccular aneurysm arising from the posterior side of the paraclinoid segment of the ICA (Fig. 2).
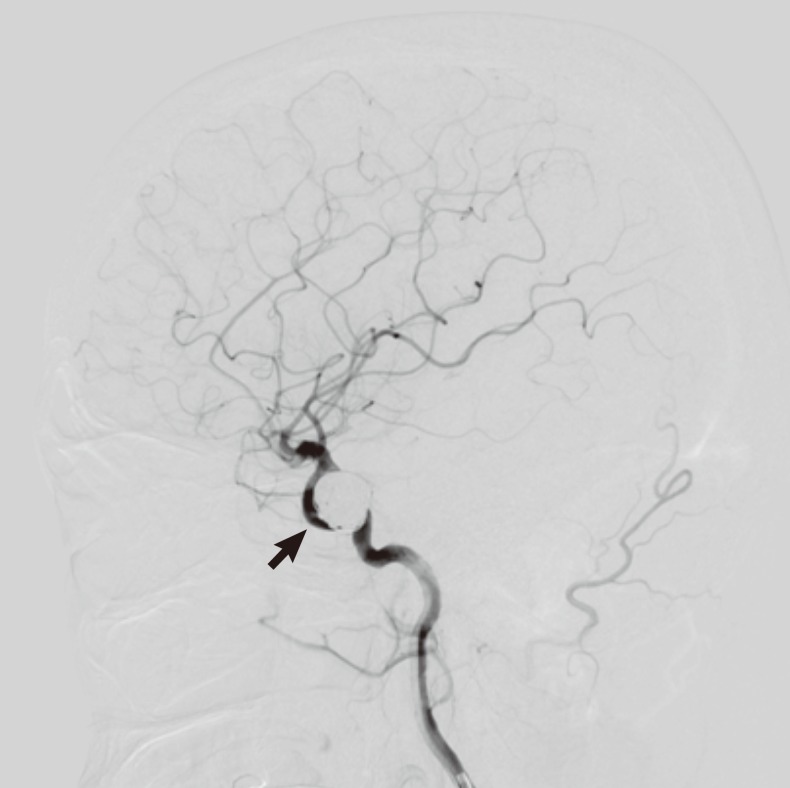
Upon this diagnosis, she was referred to the neurosurgery department for fur further workup and treatment. Neurological examination including extraocular muscle function, facial sensation, mastication power and meningeal irritation sign conducted by a neurosurgeon to rule out cavernous sinus mass lesion revealed no abnormal findings. She underwent transfemoral transarterial coil embolization of her aneurysm and the aneurysm was completely occluded on an intraoperative angiographic image (Fig. 3). After successful embolization, the tinnitus disappeared immediately and no neurological complications developed. Six months after the procedure, she still did not experience tinnitus, and the follow-up magnetic resonance angiographic image showed a completely occluded aneurysm.
Pulsatile tinnitus is tinnitus that coincides with the patient's heartbeat. It constitutes a small portion of all tinnitus, but needs aggressive radiologic evaluation because it is often the first or even sole manifestation of a pathology that, potentially, has serious effects on the nervous system [1].
Contrast enhanced high-resolution CT is regarded as the imaging modality of choice for diagnosis because it can reveal most neoplasms and abnormities that produce pulsatile tinnitus [2]. However, it has limitations with regard to diagnosing local lesions like arteriovenous fistulas, which do not show any abnormities on CT. The next additional investigation is MRI, but magnetic resonance angiography (MRA), ultrasound, and intra-arterial cerebral angiography can also be used, depending on the physician's impression.
Pulsatile tinnitus can ensue from various diseases. Sonmez et al. [2] reviewed 74 patients with pulsatile tinnitus and investigated the underlying pathology. Among them, 50 patients (67.6%) showed local causes of pulsatile tinnitus radiologically, and high jugular bulb (21%) was the most common cause in their series. Atherosclerosis, dehiscent jugular bulb and dural arteriovenous fistula followed high jugular bulb in this regard. Aneurysm of the ICA was detected in 3 patients (4.0%), but exact locations and treatments of the aneurysms were not described in the report. In other studies, analyzing 84 patients with pulsatile tinnitus, dural arteriovenous fistula was the most common cause (20.2%) and ICA aneurysm was found in only one patient [1].
One of interesting points of our case was that pulsatile tinnitus was the sole manifestation of aneurysm in the paraclinoid portion of the ICA. Paraclinoid segments span the ICA from where it exits the cavernous sinus and enters the subarachnoid space to the origin of the posterior communicating artery. Because of the distance between aneurysm and inner ear, patients with paraclinoid ICA aneurysm rarely present with bruit and, frequently, presentations of those patients are incidental, including headache, subarachnoid hemorrhage, visual change, transient ischemic attack, among other symptoms [6]. However, the patient in our case showed the pulsatile tinnitus as a sole manifestation of aneurysm in the paraclinoid portion of the ICA, which gives us interesting information that a large aneurysm in this relatively remote part of ICA from inner ear even causes pulsatile tinnitus.
Treatment of paraclinoid ICA aneurysm is challenging. From the surgical perspective, satisfactory clipping of paraclinoid aneurysms while attempting to preserve the ophthalmic artery and maintain patency of the ICA can be technically difficult. In addition, anterior clinoid process often obscures the surgical field [6]. Endovascular techniques have rapidly emerged as an alternative to surgical clipping with the recent development of neurointerventional devices and techniques, but total obliteration with endovascular treatment is still not as likely as it is with surgery [6, 7]. A variety of aneurismal directions in combination with the tortuous carotid siphon is regarded as the major cause of difficult or failed access in endovascular treatment of paraclinoid aneurysm [7].
In this case, we performed endovascular treatment and successfully occluded the aneurysm. The patient showed no abnormal neurological signs, and the tinnitus had completely disappeared.
In conclusion, pulsatile tinnitus is often the first or sole manifestation of a serious disease of the nervous system and needs aggressive radiologic evaluation. ICA aneurysm also has to be considered as a local cause of pulsatile tinnitus and has to be diagnosed and treated appropriately.
References
1. Waldvogel D, Mattle HP, Sturzenegger M, Schroth G. Pulsatile tinnitus: a review of 84 patients. J Neurol. 1998; 3. 245(3):137–142. PMID: 9553842.

2. Sonmez G, Basekim CC, Ozturk E, Gungor A, Kizilkaya E. Imaging of pulsatile tinnitus: a review of 74 patients. Clin Imaging. 2007; Mar-Apr. 31(2):102–108. PMID: 17320776.

3. Moonis G, Hwang CJ, Ahmed T, Weigele JB, Hurst RW. Otologic manifestations of petrous carotid aneurysms. AJNR Am J Neuroradiol. 2005; Jun-Jul. 26(6):1324–1327. PMID: 15956490.
4. Liu JK, Gottfried ON, Amini A, Couldwell WT. Aneurysms of the petrous internal carotid artery: anatomy, origins, and treatment. Neurosurg Focus. 2004; 11. 17(5):E13. PMID: 15633978.

5. Palacios E, Gomez J, Alvernia JE, Jacob C. Aneurysm of the petrous portion of the internal carotid artery at the foramen lacerum: anatomic, imaging, and otologic findings. Ear Nose Throat J. 2010; 7. 89(7):303–305. PMID: 20628987.
6. Hoh BL, Carter BS, Budzik RF, Putman CM, Ogilvy CS. Results after surgical and endovascular treatment of paraclinoid aneurysms by a combined neurovascular team. Neurosurgery. 2001; 1. 48(1):78–89. PMID: 11152364.

7. Kwon BJ, Im SH, Park JC, Cho YD, Kang HS, Kim JE, et al. Shaping and navigating methods of microcatheters for endovascular treatment of paraclinoid aneurysms. Neurosurgery. 2010; 7. 67(1):34–40. PMID: 20559090.

Fig. 1
Axial (A) and coronal (B) T2-weighted MRI shows a 1.4-cm signal void (arrow) in the paraclinoid region of the right internal carotid artery.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download