Abstract
Objectives
To evaluate the surgical outcomes of endoscopic dacryocystorhinostomy followed by canalicular trephination and silicone stenting in patients with distal or common canalicular obstructions.
Methods
The medical records of 29 patients (31 eyes) from January 2001 to December 2009 who underwent endoscopic dacryocystorhinostomy followed by canalicular trephination and silicone tube insertion for the treatment of distal or common canalicular obstructions were retrospectively reviewed. The level of obstruction was confirmed by intraoperative probing. The outcome of the surgery was categorized as a complete success, partial success, or failure according to the functional and anatomic patency.
Results
The average age of the patients was 52 years. The duration of silicone intubation ranged from 4 to 11 months with an average of 5.7±1.6 months. The follow-up period after stent removal ranged from 4 to 15 months with an average of 8.2±3.3 months. Complete success was achieved in 25 out of 31 eyes (80.6%), partial success in 4 out of 31 eyes (12.9%), and failure in 2 out of 31 eyes (6.5%).
In more than 90% of individuals, the superior and inferior canaliculi merge to form a common canaliculus before entry into the lacrimal sac (1). Adult onset epiphora is common in the elderly, and, although this results mostly from nasolacrimal duct obstruction, it may also concurrently or independently involve the canaliculi (2).
Canalicular obstruction may be one of the most difficult lacrimal conditions to treat. The treatment of canalicular obstruction depends on the level of the obstruction. Although conjunctivodacryocystorhinostomy (CDCR) with Jones tube insertion was regarded as the standard surgical method for either canalicular obstruction or malfunction, it was invasive and accompanied by a relatively high rate of complications and poor patient satisfaction (3, 4). Dacryocystorhinostomy (DCR) with retrograde intubation is applicable to proximal or midcanalicular obstructions but not to distal or common canalicular obstructions (5). These two procedures aim to bypass the nonfunctioning canaliculi by creating a new channel rather than restore a physiologic tear passage.
Endoscopic DCR has been used as treatment for nasolacrimal duct obstruction (6), and it allows us to observe the internal opening of the common canaliculus during operation.
Some studies on lacrimal trephination for the treatment of canalicular obstruction have been reported (7-9). However, the surgical results of endoscopic DCR and trephination in patients with lacrimal canalicular obstruction have rarely been reported (10). We conducted this study to evaluate the surgical outcomes of endoscopic DCR followed by canalicular trephination and silicone stenting in patients with distal or common canalicular obstructions.
A retrospective review of the medical records of 29 patients (31 eyes) between January 2001 and December 2009 who presented with epiphora caused by distal or common canalicular obstructions was performed. These patients underwent endoscopic DCR followed by canalicular trephination and silicone stent intubation. Approval for this study was obtained from the Hospital Medical Ethics Committee and informed consent was obtained from all subjects.
All patients were evaluated by an ophthalmologist before surgery. Preoperative evaluation consisted of a thorough eyelid and lacrimal evaluation, including Jones test and a dacryocystogram. The level of obstruction was based on preoperative probing and irrigation, and was measured in millimeters from the puncta to the end of the probe where the obstruction was felt. Proximal canalicular obstruction was classified as within 4 mm of the punctum, distal canalicular obstruction as those 5 mm or greater from the punctum, and common canalicular obstruction as those 10 mm or greater from the punctum (9). Only those cases where the distal or common canaliculus had been affected were included. The patients with proximal canalicular obstruction and those who had previous DCR were excluded.
Statistical analyses were conducted using the SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). The chi-square test was used to compare the success rate according to the levels of canalicular obstruction. P<0.05 was regarded as significant.
The surgery was performed using 0° and 30° 4-mm rigid endoscopes under general anesthesia in all cases. The nasal mucosal incisions were started approximately 8 mm above the insertion of the middle turbinate on the lateral nasal wall and carried anteriorly for approximately 10 mm. The incision was extended vertically down the frontal process of the maxilla about half of the anterior length of the middle turbinate, and then taken posteriorly to the uncinate process. The nasal mucosal flap was elevated off the maxillary bone posteriorly to the thin lacrimal bone. The elevated flap was tucked around the middle turbinate. The thin lacrimal bone and thick bone of the frontal process of the maxilla were removed using the appropriate curettes and diamond DCR bur (15°, Medtronic Xomed, Jacksonville, FL, USA). A lacrimal probe was passed from the canaliculi to tent the medial wall of the sac, and the medial sac wall was removed.
The level of obstruction was confirmed by intraoperative probing with a 2-0 Bowman probe that was advanced until a soft stop was encountered. A canalicular trephine (BD Visitec, Warks, UK) was inserted into the punctum with the stylet in place and carefully advanced within the canaliculus to the obstruction site. When blockage was encountered, the stylet was removed and the trephine was rotated in a boring manner until the tip emerged into the lacrimal sac. Extreme care was taken to avoid the formation of a false passage. Irrigation was carried out to confirm the patency of the canaliculi.
Standard silicone stents (0.64 mm outer diameter, Medtronic Xomed) were passed through the canaliculi, directed out of the nasal cavity, and tied intranasally in all patients. A through-cutting forceps was used to trim the center of the original nasal mucosal flap. The trimmed nasal mucosal flap was repositioned to cover the denuded bone area (Fig. 1). A small gelfoam patches soaked in antibiotic ointment were placed over the flap anastomosis to keep it in position during the initial healing period.
Oral and topical antibiotics, nasal steroid spray were applied for 2-3 weeks postoperatively. Patients were followed up weekly for a month. During follow-up endoscopic examination of nasal cavity was performed in order to remove crusts, granulation tissues and adhesions (if any) and to check the patency of the rhinostomy site using lacrimal irrigation. Subsequent follow up was at monthly intervals for three or four months and then every three months until it was needed. The silicone tubes were removed between 4 and 11 months postoperatively.
Postoperative evaluation included asking about subjective symptoms of epiphora, lacrimal irrigation, and endoscopic evaluation of the surgical site.
Functional patency was classified as good when the patients did not have epiphora in usual condition, as fair when the patients had improvement of epiphora but tearing occurred occasionally, and as poor when the patients had epiphora in usual condition. Anatomic patency was classified as good when irrigation passed completely through the rhinostomy site into the nose, as fair when irrigation passed but showed slight reflux or resistance, and as poor when irrigation could not completely pass.
The outcome of the surgery was categorized as a complete success, partial success or failure. Complete success was defined as good functional and anatomic patency. Partial success was defined as fair functional patency with an anatomic patency that was more than fair. All other cases were considered to be failed surgeries. In our study, postoperative endonasal endoscopy with dye test was performed in failed and partially successful cases.
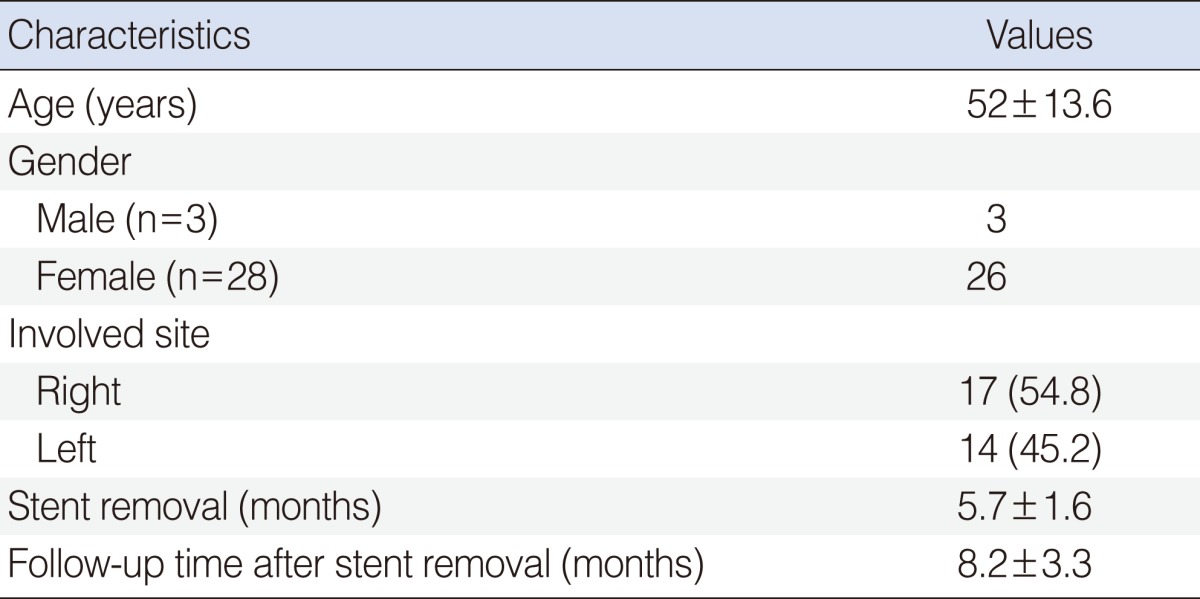
There were a total of 29 patients who underwent 31 procedures. All patients underwent primary endoscopic DCR followed by canalicular trephination and silicone stenting. The average age of the patients was 52 years and the female/male ratio was 8.7:1. The mean duration of the stent insertion was 5.7 months (range, 4 to 11 months). The mean follow-up period after stent removal was 8.2 months (range, 4 to 15 months) (Table 1).
The location of the canalicular obstruction was the common canaliculus in 17 eyes, the distal lower canaliculus in 9 eyes, and the distal bicanaliculi in 5 eyes.
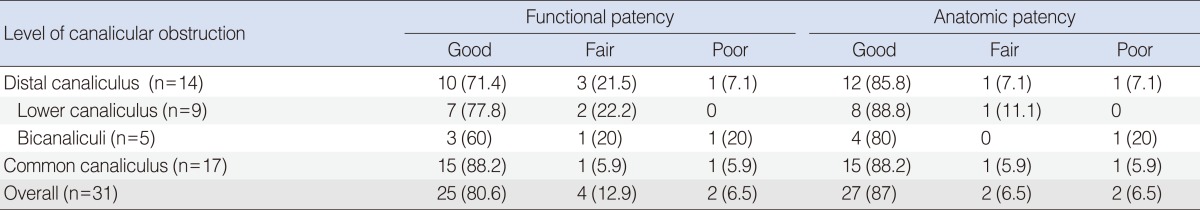
The anatomical and functional patency was assessed, and outcome of the surgery was analyzed according to the level of obstruction found at the time of surgery. Complete success was achieved in 25 out of 31 eyes (80.6%), partial success in 4 out of 31 eyes (12.9%), and failure in 2 out of 31 eyes (6.5%). When classified according to obstruction site, distal lower canalicular obstruction was treated most successfully (77.8% complete and 22.2% partial success), followed by common canalicular obstruction (88.2% complete and 5.9% partial success) and distal bicanalicular obstruction (60% complete and 20% partial success) (Table 2). However, the success rates according to the level of obstruction did not differ statistically (P=0.34, chi-square test).
Postsurgical complications were minimal. Small sized granulation tissues developed around rhinostomy site about 3 to 4 weeks after surgery in 26 eyes (83.8%), but it could be readily removed by suction tips or forceps during follow-up. Adhesions between the lateral nasal wall and middle turbinate were occurred in 19 eyes (61.3%), but were treated using the appropriate instruments as soon as they were found. No cases of orbital tissue damage, cerebrospinal fluid leak, sump syndrome, or uncontrolled bleeding had occurred.
One of the two failed cases appeared to be without problems at the rhinostomy site in the nasal cavity. However, during the irrigation test saline refluxed through the ipsilateral punctum, and the distance from the punctum to the obstruction site was 9 mm. The patient was thought to have complete reobstruction in distal canaliculus. In the other failed case the size of the bony window was thought to be sufficient, but scar tissue was noted around the rhinostomy site. In this patient, during the irrigation test saline refluxed through the contralateral punctum. The patient showed negative primary Jones test and positive secondary Jones test. In secondary Jones test clear saline without fluorescein was recovered. The distance from the punctum to the obstruction site was 11 mm. So the patient was thought to have severe restenosis in common canaliculus and also in lacrimal sac opening.
CDCR and DCR with retrograde intubation aim to bypass the nonfunctioning canaliculi by creating a new channel into nasal cavity. As other treatment modalities for canalicular obstruction, silicone stent intubation after lacrimal probing, trephination or laser canaliculoplasty and balloon catheter dilation (BCD) and BCD following lacrimal trephination have been introduced (11-16). These techniques aim to reconstruct normal canalicular channel with fewer invasion compared with CDCR and DCR with retrograde intubation.
The trephine was developed to allow for opening a canaliculus that was occluded distally (7).
Khoubian et al. (9) inserted a silicone tube after trephination in patients with canalicular obstruction. They categorized the level of canalicular obstruction as proximal obstruction, distal obstruction, and common canalicular obstruction. The outcome was divided into a complete relief, partial relief, and no improvement, according to the degree of epiphora relief at the end of the follow-up. If the patients with proximal canalicular obstruction were excluded from the subjects of their study, complete epiphora relief was achieved in 18 out of 28 eyes (64.3%), partial relief in 8 out of 28 eyes (28.6%), and no improvement in 2 out of 28 eyes (7.1%) (10). If we compare our surgical result to Khoubian's result, the overall success rates were similar to each other, but the proportion of patients with complete epiphora relief was much higher in our study than in Khoubian's study (80.6% vs. 64.3%).
Endoscopic DCR is a commonly performed technique to alleviate epiphora caused by nasolacrimal duct obstruction, and it is not difficult to identify the internal opening of the common canaliculus during the procedure.
In patients with canalicular obstruction, whether or not nasolacrimal duct obstruction was accompanied could not be assessed prior to surgery. So the necessity of performing endoscopic DCR in the treatment of the canalicular obstruction may be controversial. But we think that endoscopic DCR in the process of surgery for canalicular obstruction has two advantages. First, because this procedure is performed under high magnification and while watching the inside of the lacrimal sac, it enables the safe opening of the obstructed portion of the canaliculus with a probe or trephine. Second, even if the surgery fails, this procedure makes it easy to insert a Jones tube.
Yung and Hardman-Lea (17) performed endoscopic DCR with probing, and silicone stent intubation for individual canalicular and common canalicular obstructions. They reported complete epiphora relief in 79.3% of cases and partial relief in 13.8% of cases at 12 months after surgery. However, the degree of symptomatic improvement (complete, partial) was not clearly defined.
In the treatment of canalicular obstruction, the surgical results of endoscopic DCR and trephination in patients with lacrimal canalicular obstruction have rarely been reported. Nemet et al. (10) performed endoscopic DCR with trephination, mitomycin C administration, and silicone intubation in five patients with distal canalicular or common canalicular obstructions. They reported an 80% success rate. However, the number of subjects was too few.
According to data reported so far the success rates of various surgical procedures which aim to reconstruct normal canalicular channel for canalicular or common canalicular obstruction vary in the range of less than 50-93% with the majority being 70-85% (Table 3). Our surgical outcomes of bicanalicular silicon stenting after endo-DCR with lacrimal trephination have shown relatively good results (93.5%).
Potential complications that could occur during lacrimal trephination are damage to the normal canaliculus or false passage into either the lacrimal sac or another location. To minimize these complications in our study the proximal, normal portion of the canaliculus was sufficiently dilated before trephination and the trephine was advanced as gently as possible following the presumed normal anatomical direction into the lacrimal sac while observing the internal opening of the common canaliculus from the nasal cavity via the endoscope. As a result, there were no specific complications related to lacrimal trephination, and this may be one of the reasons for good results of our study.
The most common reason for failure after endoscopic DCR has been known to be adhesion and restenosis of the rhinostomy site (18). To improve the results of endoscopic DCR several adjunctive methods and surgical techniques are in use, such as preserving nasal mucosal flaps after wide resection of bone (19), insertion of silicone tubes (20), and treatment with mitomycin C (21).
Mitomycin C has been used in many ocular procedures and endoscopic DCR to improve the surgical result (21, 22). However, its effect on the prevention of restenosis after canalicular surgery has not been reported yet.
The necessity of silicone tubing after endoscopic DCR is controversial (23). In almost all past studies, however, silicone tubes were inserted after lacrimal canalicular surgery to prevent postsurgical restenosis. The duration of silicone tube insertion was varied from 5 weeks to 42 months (12), in our study the average duration of silicone stenting was 5.7 months.
In our study, as Table 3 demonstrates that even though the duration of the silicone tube insertion was not longer than in previous reports, the success rate (93.5%) was favorable compared to the previous reported success rates. We therefore think that a longer duration of silicone stenting is not required to ensure good surgical results.
In our study there were two failed patients. One case was symptomatic with persistent obstruction of the distal canaliculus. And the other case showed persistent obstruction of the common canaliculus and scar formation around the rhinostomy site. The possible cause of postoperative canalicular obstruction seemed to be ductal wall damage that might have occurred during trephination or recurrent episodes of canalicular infection, or be idiopathic.
The presumptive reasons for good surgical outcomes in our study are as follows. We removed a bone around lacrimal sac as large as possible, and preserved nasal mucosal flaps to leave the bare bone around rhinostomy site as little as possible. To minimize trephination related complications, normal portion of the canaliculus was sufficiently dilated before trephination and the trephine was advanced into the lacrimal sac as gently as possible while observing the internal opening of the common canaliculus directly from the nasal cavity with endoscope. We regularly cleaned around the rhinostomy site, and granulation tissues or adhesions were removed as soon as being found. These interventions could have yielded the higher success rates in our study.
Our study has several limitations. Our study population was small and we did not have appropriate controls. Ideally, a longer clinical follow-up would strengthen our conclusions.
It is difficult to directly compare the surgical results from our study with other published results because different studies have differences in surgical techniques and use different criteria for success. However, the results of our study show that endoscopic DCR followed by canalicular trephination and silicone stenting can be an effective treatment modality for patients with distal or common canalicular obstruction and the surgical success rates were favorable compared with other procedures. It may be considered for initial treatment of patients with distal or common canalicular obstructions.
References
1. Jones LT. An anatomical approach to problems of the eyelids and lacrimal apparatus. Arch Ophthalmol. 1961; 7. 66(1):111–124. PMID: 13790551.

2. Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction: a clinicopathologic report and biopsy technique. Ophthalmology. 1986; 8. 93(8):1055–1063. PMID: 3763155.
3. Jones LT. The cure of epiphora due to canalicular disorders, trauma and surgical failures on the lacrimal passages. Trans Am Acad Ophthalmol Otolaryngol. 1962; Jul-Aug. 66:506–524. PMID: 14452301.
4. Rosen N, Ashkenazi I, Rosner M. Patient dissatisfaction after functionally successful conjunctivodacryocystorhinostomy with Jones tube. Am J Ophthalmol. 1994; 5. 117(5):636–642. PMID: 8172270.

5. Wearne MJ, Beigi B, Davis G, Rose GE. Retrograde intubation dacryocystorhinostomy for proximal and midcanalicular obstruction. Ophthalmology. 1999; 12. 106(12):2325–2328. PMID: 10599666.
6. McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989; 6. 103(6):585–587. PMID: 2769026.

7. Sisler HA, Allarakhia L. A new ophthalmic microtrephine. Ophthalmic Surg. 1990; 9. 21(9):656–657. PMID: 2250878.

8. Sisler HA, Allarakhia L. New minitrephine makes lacrimal canalicular rehabilitation an office procedure. Ophthal Plast Reconstr Surg. 1990; 6(3):203–206.
9. Khoubian JF, Kikkawa DO, Gonnering RS. Trephination and silicone stent intubation for the treatment of canalicular obstruction: effect of the level of obstruction. Ophthal Plast Reconstr Surg. 2006; Jul-Aug. 22(4):248–252.

10. Nemet AY, Wilcsek G, Francis IC. Endoscopic dacryocystorhinostomy with adjunctive mitomycin C for canalicular obstruction. Orbit. 2007; 6. 26(2):97–100. PMID: 17613855.

11. Keith CG. Intubation of the lacrimal passages. Am J Ophthalmol. 1968; 1. 65(1):70–74. PMID: 5635571.

12. Pashby RC, Rathbun JE. Silicone tube intubation of the lacrimal drainage system. Arch Ophthalmol. 1979; 7. 97(7):1318–1322. PMID: 454271.

13. Dutton JJ, Holck DE. Holmium laser canaliculoplasty. Ophthal Plast Reconstr Surg. 1996; 9. 12(3):211–217.

14. Kuchar A, Novak P, Pieh S, Fink M, Steinkogler FJ. Endoscopic laser recanalisation of presaccal canalicular obstruction. Br J Ophthalmol. 1999; 4. 83(4):443–447. PMID: 10434867.

15. Wilhelm KE, Hofer U, Textor HJ, Boker T, Strunk H, Schild HH. Nonsurgical fluoroscopically guided dacryocystoplasty of common canalicular obstructions. Cardiovasc Intervent Radiol. 2000; Jan-Feb. 23(1):1–8. PMID: 10656900.

16. Yang SW, Park HY, Kikkawa DO. Ballooning canaliculoplasty after lacrimal trephination in monocanalicular and common canalicular obstruction. Jpn J Ophthalmol. 2008; Nov-Dec. 52(6):444–449. PMID: 19089564.

17. Yung MW, Hardman-Lea S. Analysis of the results of surgical endoscopic dacryocystorhinostomy: effect of the level of obstruction. Br J Ophthalmol. 2002; 7. 86(7):792–794. PMID: 12084752.

18. Sprekelsen MB, Barberan MT. Endoscopic dacryocystorhinostomy: surgical technique and results. Laryngoscope. 1996; 2. 106(2 Pt 1):187–189. PMID: 8583851.
19. Tsirbas A, Wormald PJ. Endonasal dacryocystorhinostomy with mucosal flaps. Am J Ophthalmol. 2003; 1. 135(1):76–83. PMID: 12504701.

20. Unlu HH, Toprak B, Aslan A, Guler C. Comparison of surgical outcomes in primary endoscopic dacryocystorhinostomy with and without silicone intubation. Ann Otol Rhinol Laryngol. 2002; 8. 111(8):704–709. PMID: 12184592.

21. Camara JG, Bengzon AU, Henson RD. The safety and efficacy of mitomycin C in endonasal endoscopic laser-assisted dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2000; 3. 16(2):114–118.

22. Dolmetsch AM. Nonlaser endoscopic endonasal dacryocystorhinostomy with adjunctive mitomycin C in nasolacrimal duct obstruction in adults. Ophthalmology. 2010; 5. 117(5):1037–1040. PMID: 20079535.

23. Smirnov G, Tuomilehto H, Terasvirta M, Nuutinen J, Seppa J. Silicone tubing after endoscopic dacryocystorhinostomy: is it necessary? Am J Rhinol. 2006; Nov-Dec. 20(6):600–602. PMID: 17181101.

Fig. 1
Trimmed nasal mucosal flaps are in place around the rhinostomy site to cover the raw bone. IT, inferior turbinate; MT, middle turbinate.
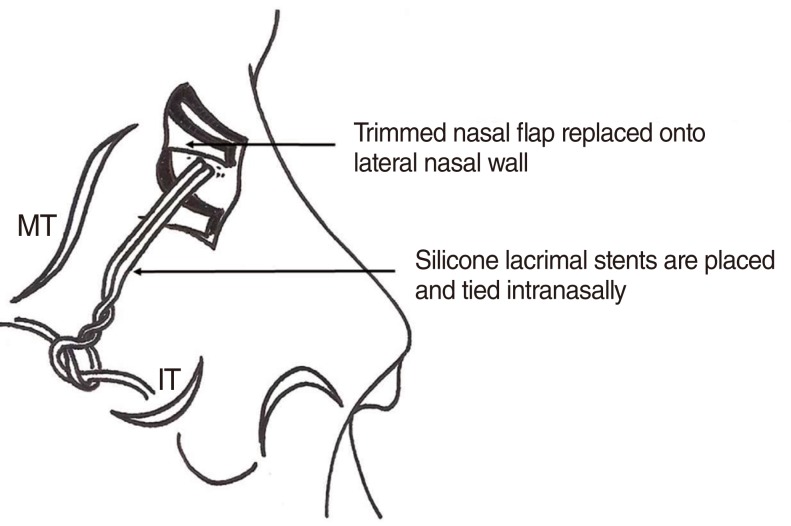
Table 3
Comparison of other surgical results for canalicular obstruction

No., number of affected eyes; C, canaliculus; CC, common canaliculus; DC, distal canaliculus; DCR, dacryocystorhinostomy; MMC, mitomycin C; NM, no mentioned.
*Average period of silicone stent intubation. †84.2% success in cases where an obstruction of less than 2 mm was present. ‡<50% success in cases where an obstruction of more than 2 mm was present.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download