Abstract
Objectives
In the present study, we investigated whether speech-related cognitive function and speech recognition ability under background noise in adults with hearing impairment are improved with the use of hearing aids.
Methods
Participants were recruited from the ENT Department of Eulji Hospital from September 2008 to July 2009. The study group comprised 18 participants (mean age, 69.5±8.3 years) with sensorineural hearing loss who were fitted with hearing aids, and the control group comprised 11 participants of equivalent age (mean age, 63.1±11.8 years) who were not fitted with hearing aids. All participants were assessed using the computerized Korean visual verbal learning test (VVLT) and words-in-noise (WIN) test prior to fitting of hearing aids for the study group and initially for the control group. Both groups were reassessed in both tests after 6 months. For each group, differences in the results between the two assessments were compared using the Friedman test.
Results
There was no difference in mean age between the study group and control group. In the study group, total VVLT score (reflecting short-term memory) was significantly improved from before hearing aid use to 6 months after hearing aid use (P<0.05), and VVLT recognition score (reflecting learning ability) was also significantly improved from before hearing aid use to 6 months after hearing aid use (P<0.05), but there was no change in the control group. For VVLT latency score (reflecting efficiency of memory) and speech discrimination score in the WIN test, no statistically significant difference was found between the initial and 6-month assessments in the study group or in the control group (P>0.05).
An intact auditory system and proper cognitive function of the cerebral cortex are essential for communication using language. The cognitive system contains working memory which enables memorizing of words heard a short time ago, lexical information, and comprehension of context (1, 2). The comprehension of language requires exchange of information between the auditory cortex and frontal cortex or amygdala, which are concerned with cognitive function. A negative relationship between sensory input and cognitive function is commonly explained by neurodegenerative process. Thus, the correlation between sensory function and cognitive ability may increase in older age because both are affected by age-related physiological change in brain function (3). Indeed, older adults show impaired hearing performance by both decreased hearing ability and degenerated cognitive functioning. The dominant components of presbycusis are the gradual degeneration of hair cells (mainly in the basal part of the cochlea) and atrophy of the stria vascularis and spiral ganglion cells; however, sclerotic changes in the brain are attributed as a central component (4). It was demonstrated in an animal study that deprivation of auditory input causes re-organization of the topographic map of the auditory cortex; the cortical lesion innervated by the damaged section of the cochlea becomes covered by expanded innervations of adjacent undamaged parts of the cochlea (5).
Improvement in hearing performance that is related to the central nervous system is termed auditory acclimatization, and is reported in several studies. Plastic changes in the auditory pathway were observed in adults with post-childhood onset of profound unilateral deafness. Comparing these subjects with monoaurally stimulated normal-hearing subjects, auditory-evoked potentials showed significant increases in interhemispheric waveform, cross-correlation coefficients, and peak amplitude correlations (6). However, there is only limited information available regarding improvements in cognitive function associated with long-term hearing-aid use. If the acoustic input from a hearing aid reactivates neurons that have become responsive to boundary or lesion-edge frequencies, auditory performance and cognitive function associated with hearing could be improved. In a randomized controlled trial, Mulrow et al. (7) found that 99 adults who used hearing aids for 4 months had significantly better general cognitive performance than did the control group. In contrast, several studies have reported no improvement in cognitive performance after using hearing aids (8, 9).
The cognitive function test associated with hearing is a good indicator of central auditory ability, while the ability to recognize speech from background noise also reflects central auditory ability, and correlates with the cognitive function test (10).
In the present study, we investigated whether speech-related cognitive function and speech recognition ability under background noise in adults with hearing impairment are improved after using hearing aids.
Participants were recruited from the ENT Department of Eulji Hospital, Korea, from September 2008 to July 2009. The study group comprised 18 participants (mean age, 69.5±8.3 years) with sensorineural hearing loss who were fitted with hearing aids and followed up for at least 6 months. The control group comprised 11 participants of equivalent age (mean age, 63.1±11.8 years) who were not fitted with hearing aids. All participants had sensorineural hearing loss with progressive symptom course; patients with hearing loss due to specific disease such as otitis media, labyrinthitis, and sudden sensorineural hearing loss were excluded.
No participant reported any specific visual problems that would generate visual impairment for the computerized Korean visual verbal learning test (VVLT). All participants were assessed using the VVLT and words-in-noise (WIN) test before hearing aid use for the study group and initially for the control group, and were reassessed in both tests after 6 months.
Cognitive function was examined in all subjects by the computerized Korean VVLT, using the computerized neurocognitive function test 40 (Maxmedica, Seoul, Korea). Fifteen basic words were shown at an interval of 1 second, after which the subject was asked to recall and speak the words in any order. The number of correctly recalled words was then recorded. The same test was repeated 5 times, and the scores summed to obtain the total score. In the latency test, performed 20 minutes after the first test, the subject was asked to recall and speak the basic words one more time. In the recognition test, the original 15 words were shown along with 35 interference words, and the subject was asked to recall and speak only the original words. After completion of the three tests, subset scores (total score, latency score, and recognition score) were calculated automatically using computer software.
Audiologic testing was performed by an Orbiter 922 (GN Otometrics, Copenhagen, Denmark) in a soundproof room (RE-140, Acoustic Systems, Houston, TX, USA) with headphones (TDH-50P, Telephonics, New York, USA). The sound field test was performed by connecting a speaker (Denon SC-M53, Shanghai, China) to the audiologic test equipment through an amplifier (R300 plus, InterM, Los Angeles, CA, USA).
The WIN test was performed in the sound field with signals and noise emitted from a speaker installed 1 m away from the front (0°) of the subject. Twenty-five monosyllables were presented to the subject by live voice under multi-talker babble noise in the Korean language. The intensity of the noise was fixed at 70 dB HL, and the signal-to-noise ratio (SNR) was -3 dB. The correct reaction rate was indicated as speech discrimination score (SDS) in noise (%). The study group was tested without hearing aids.
We used the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis. The ages of the hearing aid group and of the control group were verified by the Mann-Whitney U-test. The Friedman test was used to compare the initial and 6-month results of the VVLT and the WIN test, for each group.
There was no difference in mean age between the study group and control group. Pure tone averages in the study group were 50.3±14.7 dB for the better ear and 64.4±21.2 dB for the worse ear. Pure tone averages in the control group were 40.7±19.0 dB and 44.4±20.8 dB, respectively.
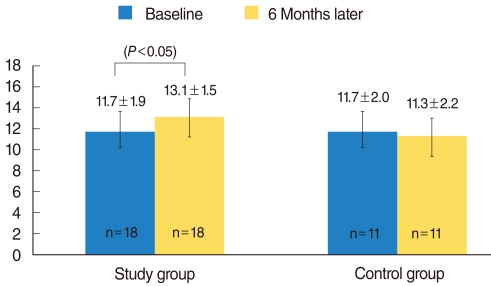
In the initial VVLT test, there was no difference between the two groups for all three subset scores (P>0.05). For the total score of the computerized Korean VVLT, statistically significant differences were found in the study group between before hearing aid use and 6 months after hearing aid use (32.7±8.3 vs. 38.5±11.8; P<0.05) but not in the control group (34.4±6.9 vs. 34.1±7.3) (Fig. 1). For the recognition score, statistically significant differences were found in the control group between before hearing aid use and 6 months after hearing aid use (11.7±1.9 vs. 13.1±1.5; P<0.05), but not in the control group (11.7±2.0 vs. 11.3±2.2) (Fig. 2). For the latency score, no statistically significant difference was found between the initial and 6-month assessments in the study group (7.5±2.9 vs. 8.4±2.5; P>0.05) or in the control group (7.3±1.9 vs. 8.1±3.1; P>0.05) (Fig. 3).
Regarding SDS in noise in WIN test, the initial score was higher in the control group (P<0.05), whereas no statistically significant difference was found between the initial and 6-month assessments in the study group (32.5±18.6 vs. 32.5±21.3; P>0.05) or in the control group (55.5±18.9 vs. 55.9±20.4; P>0.05) (Fig. 4).
The results of the present study indicate that in individuals with hearing impairment, use of hearing aids not only increases input of the auditory signal but also affects the central nervous system, enabling more efficient processing of speech perception. These findings indicate that degenerated cognitive function connected with speech can be acclimatized by using hearing aids.
The cognitive function test employed in the present study is a word-listed learning test comprising 15 words. It was developed into a computerized test to enable more objective and accurate evaluation by selecting Korean words, applying the principle of the Rey auditory verbal learning test, as developed by the Swiss psychologist, Andre Rey (11). The Rey auditory verbal learning test has been used widely in clinical neuropsychological assessment of older adults as a sensitive measure of word list learning and memory. Performance of the Rey auditory verbal learning test was associated with a broad set of isocortical regions that have been implicated in working memory, language, and semantic processing. Auditory verbal working memory is likely critical to the initial trials of a list-learning memory task and crucial for the transfer of information into a long-term store (12, 13). Because the computerized test maintains consistent stimuli, excludes bias of the examiner, and records response accurately, reliable results can be generated without direct tests by psychiatrists or cognitive function test experts. It is important to consider the modality of stimuli when performing the cognitive function test on individuals with hearing impairment. A verbal test might disadvantage individuals with a hearing impairment because effortful listening consumes cognitive resources that could otherwise be allocated to the storage of information in working memory (14, 15). Therefore, we used nonverbal, visually presented cognitive tests. The present study was modified from the original test based on auditory signal, and was conducted by asking the subject to identify words presented on a monitor. We assessed working memory, which indicates personal short-term memory among language learning functions through the summation of recalled words (total score), in the computerized Korean VVLT. The latency test reflects the efficiency of memory in terms of the degree to which newly learned information is maintained. The recognition test indicates learning ability in a short time, regardless of the efficiency of memory. Two subsets of the VVLT (total score and recognition score) showed significant improvement following the use of hearing aids, while latency score showed no significant change. These results can be interpreted to mean that short-term memory for speech recognition is more strongly influenced by hearing aid use than is long-term memory. Another important consideration in this cognitive function test is the exclusion of the learning effect, which can make the test easier the second time. In the present study, we measured cognitive function approximately 6 months after the hearing aids were fitted because habituation to hearing aid use stabilizes after this period of time (16). Because no score showed improvement after 6 months in the control group, we can disregard the possibility of the learning effect.
In 1990, Murlow et al. (7) investigated 194 adults older than 64 years, 95 of whom were fitted with a hearing aid. They found a positive effect on cognitive function between baseline and the 4-month follow-up, using the Short Portable Mental Status test. The authors concluded that hearing aids are effective in treating the social, emotional, and communicational dysfunction caused by hearing loss, and that they also improve cognitive function. In contrast, another study reported no statistically significant improvement of performance in the hearing aid group (age, 51 to 87 years; n=70) after 6 months, using five tests, including speed (digit symbol substitution, digit letter), fluency (animals, letter "s"), and vocabulary (spot-a-word) to test cognitive function (8). In 2005, van Hooren et al. (9) reported that hearing aid use did not affect cognitive performance in older adults over a 12-month period. When the cognitive function of a hearing aid group (56 patients) was compared with that of a control group (46 patients) every 12 months using several cognitive function tests, including VVLT, there was no statistically significant difference between the two groups. The results of these last two studies are contrary to the present results.
Significant correlations exist between the measures of cognitive performance and speech recognition in noise, both with and without hearing aids (2, 10). In a previous study by the author, positive correlation was found between all VVLT results and SDS in noise, and between the Mini-Mental Status Examination result and SDS in noise (17). These results demonstrated that cognitive function was well reflected by the WIN test. It has been shown that in bilateral, hearing-impaired subjects using a long-term single hearing aid, the normally aided ear performed better for speech identification in the presence of background noise than did the unaided ear at high sound pressure level (>75 dB) (18). In another study, the same author reported that improvement of speech identification in the presence of background noise appeared in the normally aided ear after 6 weeks of use, with the benefit increasing over time for the following 12 weeks (19). In the present study, however, we observed no significant improvement in the normally aided ear in the WIN test, possibly reflecting the differences in the tests used in the various studies. Additional time might be needed before significant improvement is seen in speech identification in the presence of background noise under the conditions of our WIN test.
In comparing the pure tone average, the control group had better hearing than did the study group. The control group would ideally have been matched for hearing level as well as age, but it was unrealistic that we would be able to find subjects with similar levels of hearing loss as the control group who would agree to postpone being fitted with hearing aids, and who were willing to participate in the study for 6 months. Therefore, the control group was set as patients with mild hearing loss (average 40.7±19.0 dB, 44.4±20.8 dB) who would postpone being fitted with hearing aids. Although there were some discrepancies in hearing level between the two groups (better ear, 9.6 dB; worse ear, 20.0 dB) in the initial VVLT, all three subset scores showed no difference between the two groups.
Two hypotheses have been proposed to explain the strong correlations between hearing ability and cognitive capacity in old age. The "cascade hypothesis" proposes that a decrease in hearing ability over an extended period affects cognitive functioning because of sensory underload, which explains the improvement of cognitive function following restoration of sensory input by hearing aid use (20). The "common cause hypothesis" argues that decreases in central cognitive processing simultaneously affect sensory and cognitive functioning (21). According to the common cause hypothesis, hearing aids should not lead to improved cognitive functioning because the underlying central aging mechanism is unaffected by acoustic amplification. The results of the present study support the cascade hypothesis.
We could not estimate the exact time interval required for rehabilitation of the central auditory system by hearing aid use because of variations among individuals in terms of age, hearing level, duration of sensory deficit, and original ability for cognition. However, we were aware that prolonged understimulation of the cognitive system could lead to irreversible change, in which case aural rehabilitation would produce no effect on cognitive functioning. It is clear that early rehabilitation is an important factor in restoring cognitive function for speech perception.
The results of the computerized Korean VVLT before and after wearing hearing aids showed an improvement in speech-related cognitive function within a short time, particularly with regard to working memory and learning ability. This finding indicates that hearing aids not only compensate for sound attenuation caused by cochlear lesions but may also induce acclimatization of the regions of the central auditory system associated with speech perception.
ACKNOWLEDGEMENT
The computerized Korean visual verbal learning test was provided by Maxmedica Inc. (Seoul, Korea).
References
1. Humes LE, Burk MH, Coughlin MP, Busey TA, Strauser LE. Auditory speech recognition and visual text recognition in younger and older adults: similarities and differences between modalities and the effects of presentation rate. J Speech Lang Hear Res. 2007; 4. 50(2):283–303. PMID: 17463230.

2. Lunner T. Cognitive function in relation to hearing aid use. Int J Audiol. 2003; 7. 42(Suppl 1):S49–S58. PMID: 12918610.

3. Anstey KJ, Luszcz MA, Sanchez L. A reevaluation of the common factor theory of shared variance among age, sensory function, and cognitive function in older adults. J Gerontol B Psychol Sci Soc Sci. 2001; 1. 56(1):P3–P11. PMID: 11192335.

4. Syka J. Plastic changes in the central auditory system after hearing loss, restoration of function, and during learning. Physiol Rev. 2002; 7. 82(3):601–636. PMID: 12087130.

5. Rauschecker JP. Auditory cortical plasticity: a comparison with other sensory systems. Trends Neurosci. 1999; 2. 22(2):74–80. PMID: 10092047.

6. Ponton CW, Vasama JP, Tremblay K, Khosla D, Kwong B, Don M. Plasticity in the adult human central auditory system: evidence from late-onset profound unilateral deafness. Hear Res. 2001; 4. 154(1-2):32–44. PMID: 11423213.

7. Mulrow CD, Aguilar C, Endicott JE, Tuley MR, Velez R, Charlip WS, et al. Quality-of-life changes and hearing impairment: A randomized trial. Ann Intern Med. 1990; 8. 01. 113(3):188–194. PMID: 2197909.
8. Tesch-Romer C. Psychological effects of hearing aid use in older adults. J Gerontol B Psychol Sci Soc Sci. 1997; 5. 52(3):P127–P138. PMID: 9158564.

9. van Hooren SA, Anteunis LJ, Valentijn SA, Bosma H, Ponds RW, Jolles J, et al. Does cognitive function in older adults with hearing impairment improve by hearing aid use? Int J Audiol. 2005; 5. 44(5):265–271. PMID: 16028789.

10. Carhart R, Tillman TW. Interaction of competing speech signals with hearing losses. Arch Otolaryngol. 1970; 3. 91(3):273–279. PMID: 5414080.

11. Kwon JS, Lyoo IK, Hong KS, Yeon BK, Ha KS. Development and standardization of the computerized memory assessment for Korean adults. J Korean Neuropsychiatr Assoc. 2002; 3. 41(2):347–362.
12. Chang YL, Bondi MW, Fennema-Notestine C, McEvoy LK, Hagler DJ Jr, Jacobson MW, et al. Brain substrates of learning and retention in mild cognitive impairment diagnosis and progression to Alzheimer's disease. Neuropsychologia. 2010; 4. 48(5):1237–1247. PMID: 20034503.

13. Wolk DA, Dickerson BC. Alzheimer's Disease Neuroimaging Initiative. Fractionating verbal episodic memory in Alzheimer's disease. Neuroimage. 2011; 1. 54(2):1530–1539. PMID: 20832485.

14. Braden JP. Intellectual assessment of deaf and hard-of-hearing people: a quantitative and qualitative research synthesis. Sch Psychol Rev. 1992; 21(1):82–94.

15. Schneider BA, Daneman M, Pichora-Fuller MK. Listening in aging adults: from discourse comprehension to psychoacoustics. Can J Exp Psychol. 2002; 9. 56(3):139–152. PMID: 12271745.

16. Henrichsen J, Noring E, Lindemann L, Christensen B, Parving A. The use and benefit of in-the-ear hearing aids: A four-year follow-up examination. Scand Audiol. 1991; 20(1):55–59. PMID: 1842270.
17. Song SJ, Shim HJ, Park CH, Lee SH, Yoon SW. Analysis of correlation between cognitive function and speech recognition in noise. Korean J Otorhinolaryngol-Head Neck Surg. 010; 4. 53(4):215–220.

18. Gatehouse S. Apparent auditory deprivation effects of late onset: the role of presentation level. J Acoust Soc Am. 1989; 12. 86(6):2103–2106. PMID: 2600300.

19. Gatehouse S. The time course and magnitude of perceptual acclimatization to frequency responses: evidence from monaural fitting of hearing aids. J Acoust Soc Am. 1992; 9. 92(3):1258–1268. PMID: 1401514.

21. Lindenberger U, Baltes PB. Sensory functioning and intelligence in old age: a strong connection. Psychol Aging. 1994; 9. 9(3):339–355. PMID: 7999320.

Fig. 1
Comparison of total scores between the study and control groups. After 6 months, the study group showed significant improvement in total score, from 32.7±8.3 to 38.5±11.8 (P<0.05), whereas the total score of the control group was unchanged.

Fig. 2
Comparison of recognition scores between the study and control groups. After 6 months, the study group showed significant improvement in recognition score, from 11.7±1.9 to 15.3±2.3 (P<0.05), whereas the recognition score of the control group was unchanged.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download