INTRODUCTION
Incomplete glottal closure resulting from unilateral vocal fold paralysis can cause impairment of most of the laryngeal functions, including airway protection, breathing and stabilization of the body core during physical activity and phonation. However, dysphonia and vocal efficiency are generally the main concerns of the patient and the treatment team (
1). The decision for surgical or behavioral intervention for patients with vocal fold paralysis is driven by the patient's perception of a vocal handicap and the expectation on the part of the surgeon, the voice therapist and the patient that treatment will address the patient's primary concerns (
2).
Voice disability resulting from unilateral vocal fold paralysis is most commonly managed by voice therapy. If voice therapy fails to restore a sufficient voice and the swallowing function, then phonosurgical intervention is recommended and particularly in cases with a wide glottal gap (
3). Vocal fold augmentation, laryngeal framework surgery and laryngeal reinnervation techniques have been proposed and applied for correction of glottal insufficiency (
2). Since Isshiki et al. (
4) introduced the basic technique of thyroplasty, laryngeal framework surgery has been frequently used as a procedure for the management of incomplete glottal closure. Several modifications of Isshiki thyroplasty type I have subsequently been presented with the aim of optimizing the intra-operative surgical time, the positioning of the implant and the implant material itself such as Silasticie (
5), hydroxilapatite (
6,
7), Vitalium [miniplates] (
8,
9), expanded polytetrafluoroethylene (Gore-Tex) (
10,
11), and titanium implants (
3,
12). The goal of the current study is to demonstrate the functional voice outcomes following external medialization thyroplasty using autologous cartilage from the nasal septum with the patient under local anesthesia.
Go to :

MATERIALS AND METHODS
Patients
This study has been reviewed and approved by the Ethical Committee, Al-Menoufiya University College of Medicine. The study included 15 patients who presented to the Phoniatrics and Otolaryngology clinics at Al-Menoufiya University Hospital during the period from January 2008 to March 2009 and who were diagnosed with unilateral vocal fold paralysis. All the patients who participated in this study gave us written informed consent and they were well informed about the surgical procedures, the expected outcomes and the possible complications.
There were 6 females and 9 males included in the study and their average age was 45.5 year. Seven patients had left vocal fold paralysis while 8 patients had right vocal fold paralysis. The etiological classification of the cases included in the study is shown in
Table 1.
Table 1
Etiological classification of the patients with unilateral vocal fold paralysis


Most of the patients were diagnosed with idiopathic vocal fold paralysis (10 patients), while there were 4 patients in a post-thyroidectomy state and only one patient had recently undergone cardiac surgery. The patients had unilateral vocal fold paralysis for an average duration of 9 months (the duration ranged from 7 to 13 month). All the patients complained of a change of voice, yet choking was not a consistent complaint for many of them. Twelve patients received pre-operative voice therapy (about 20 to 25 sessions per patient) while the remaining three refused the voice therapy and they preferred the surgical option from the start.
The patients underwent comprehensive assessment that included history taking, voice recording, auditory perceptual assessment, videolaryngostroposcopy and acoustic voice analysis. The patients were evaluated pre-operatively and at 1 week and 6 months post-operatively. All the patients showed up at the first follow-up visit (1 week, yet only 12 patients showed up at the second follow-up visit (after 6 months).
Auditory perceptual assessment
The patients were instructed to count from 1-10, read a standardized passage and sustain the vowels /a/, /i/, and /u/ at a comfortable pitch and loudness in an acoustically treated room. These voice samples were recorded using a Sony DAT 60ES tape recorder. The recorded samples were evaluated by three phoniatricians according to the GRBAS scale in which the following parameters were rated on a scale from 0 (normal) to 4 (severe): the overall grade (G) of dysphonia, roughness (R), breathiness (B), and straining (S). The average rating of the three raters was included in the statistical analysis.
Videolaryngostroboscopic examination
Each patient underwent rigid telescopic videolaryngostroboscopy (VLS) before surgery and again after surgery at each follow-up visit (at 1 week and 6 months post surgery). VLS was performed using an Explorent 90° rigid telescope connected to a charge-coupled device camera (model 2687, Explorent, Germany) and a light source.
Acoustic voice analysis
The patients underwent acoustic voice analysis in a soundproof room using a standardized protocol. A constant mouth-to-microphone distance of 15 cm was maintained. The patients were instructed to sustain the vowel /i/ at a comfortable pitch and loudness. A 6 second data sample was used for analysis by using Computer Speech Laboratory Software (Dr. Speech, ver. 4, Tiger DRS Inc., Seattle, WA, USA). From the sustained vowel /i/, the fundamental frequency, jitter, shimmer and harmonic-to-noise ratio (HNR) values were obtained. The maximum phonation time was measured using a computer cursor over a waveform display of the airflow and acoustic signals.
Surgical procedure
Septal cartilage harvest procedure
Anesthesia
Infiltration anesthesia was done using 1.5 mL of anesthetic solution (1% or 2% lidocaine with 1:100,000 epinephrine). Injection was done in the following sites bilaterally: intercartilaginous injection of the nasal dorsum from the region of the rhinion to the supratip region, and at the base of the columella and the nasal tip and this injection was extended into the floor of the nose.
Surgical technique
The graft was obtained through a hemi-transfixion incision. Mucoperichondrial flaps were raised bilaterally to expose the quadrangular cartilage. Mucoperiosteal flaps were also raised over the vomer and the maxillary crest to provide maximum exposure. A vertical incision was made roughly 1.5 cm posterior to the caudal border of the quadrangular cartilage. A second cartilaginous incision was then made parallel to the dorsum about 1.5 cm below the nasal dorsum. The septal cartilage was harvested by disarticulating it from the maxillary crest, the vomer and the perpendicular plate of the ethmoid bone. To prevent damage to the nasal bridge and the development of a saddle nose, it was essential to be sure that at least 1 cm of cartilage remained both dorsally and below. The incision was sutured with silk. A nasal pack was applied as an internal splint to adapt the mucoeperichondrium to the nasoseptal cartilage and prevent formation of a hematoma.
Medialization thyroplasty procedure
Anesthesia
Infiltration anesthesia was done through injecting 2 mL of anesthetic solution (1% or 2% lidocaine with 1:100,000 epinephrine) postero-laterally to the depth of the midpoint of the posterior border of the sternomastoid muscle (at the level of the cricoids cartilage). An additional 2 mL were injected superiorly and inferiorly to the point of the primary injection. The same procedure was repeated on the opposite side.
Surgical technique
All the thyroplasties were performed by the same surgeon (Author #2). The technique used for medialization of the vocal fold has been previously reported by Isshiki et al. (
4). The thyroplasty was applied in 8 patients on the right side and in 7 patients on the left side. A horizontal paramedian cervical incision was made over the middle of the thyroid cartilage. Dissection was carried out in a subplatysmal plane, the strap muscles were retracted and the thyroid lamina was exposed. A perichondrial rectangle (window) was made at the level of the vocal folds (6 mm from the midline) and it measured 5 mm (height)×12 mm (length). The cartilage window is subsequently cut (
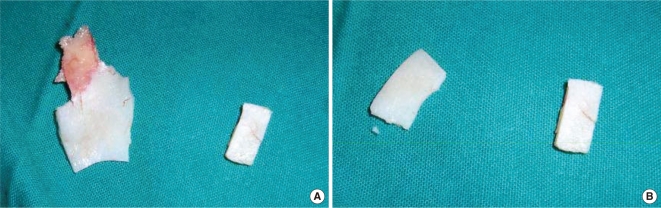
Fig. 1). With using a relatively blunt instrument, the inner perichondrium was circumferentially elevated in a careful way to avoid injuring it. A piece of the septal cartilage was cut and shaped into a rectangular graft with larger measurements than the window that was created in the thyroid lamina (
Fig. 2). The cartilage graft was then carefully tucked into the window superficially to the inner perichondrium. To assess the best implant position intraoperatively, a perceptual evaluation of the patient's voices was done and further layers of the graft were inserted if needed to achieve the best voice quality the patient can produce. Intra-operative perceptual evaluation was carried out by asking the patient to count from 1-10 and rehearse a standardized passage that was memorized by all the patients. The patient's voice quality was judged by consensus agreement between the surgeon (YAK) and a phoniatrician (TAM), who attended the surgical procedures. All the patients received wound drainage for approximately 2 days and they were observed in the hospital after surgery for an average of 3 days. The patients were evaluated at 1 week after surgery and then at the 6 months follow-up.
 | Fig. 1The cartilage window in the thyroid cartilage. 
|
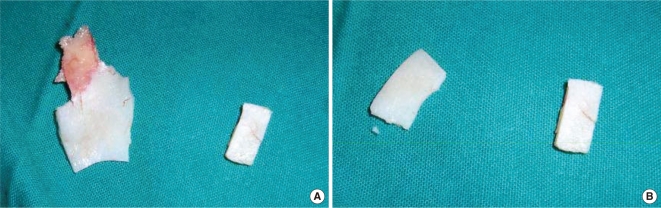 | Fig. 2The nasal septal cartilage after being removed. (A) The nasal septal cartilage as a whole and the rectangular shaped part of the cartilage to be placed in the window. (B) Two chips of the nasal septal cartilage that are used in medialization. 
|
Statistical analysis
The data is presented as means and standard deviations. Comparisons of the acoustic and perceptual data of the patients pre- and post-operatively were performed using paired sample student t-tests. The significance level was set to 0.05 throughout the analysis. The SPSS ver. 11 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis.
Go to :

RESULTS
The study included 15 patients (6 females and 9 males, age range: 30 to 57 years) who were diagnosed with unilateral vocal fold paralysis. Medialization thyroplasty type I was performed for all the patients using autologous nasal septal cartilage with the patients under local anesthesia. Pre-operatively, the laryngoscopic examination revealed incomplete glottic closure with a total glottal gap during phonation (
Fig. 3). On the post-operative evaluation, complete glottis closure was achieved in 11 patients (
Fig. 4), while 3 patients had a small post-operative posterior gap (
Fig. 5), and one patient had a residual glottal gap post-operatively.
 | Fig. 3Pre-operative laryngoscopic assessment of a patient with right vocal fold paralysis and a total glottis gap. 
|
 | Fig. 4Post-operative laryngoscopic assessment of a patient with right vocal fold paralysis and almost complete glottis closure. 
|
 | Fig. 5Post-operative laryngoscopic assessment of a patient with right vocal fold paralysis and a posterior glottis gap. 
|
Pre-operatively, stroboscopic assessment of all the patients demonstrated obvious asymmetry in the movement of the mucosal wave between the paralyzed vocal fold and the healthy one. On the post-operative assessment, although there was a complete glottis closure in most of the patients, no evident mucosal waves were observed on the paralyzed vocal folds at the 1 week follow-up visit or the 6 months follow-up visit.
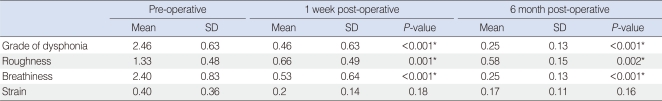
The perceptual and acoustic voice evaluations of the patients, including the pre-operative assessment and the 1 week- and 6 month post-operative assessment, are shown in
Tables 2 and
3. On comparing the pre-operative perceptual voice assessment with that at 1 week after the operation, most of the included perceptual parameters showed significant improvement (
P<0.001) (
Table 2). This significant improvement continued to be shown between the pre-operative perceptual assessment and that of the 6 months follow-up evaluation (
P<0.001) (
Table 2).
Table 2
Comparison between the pre-operative perceptual voice evaluation of the patients and that at 1 week and 6 months post-operatively
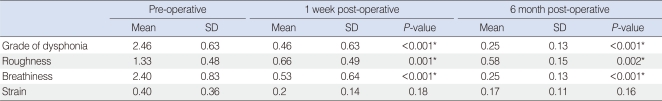

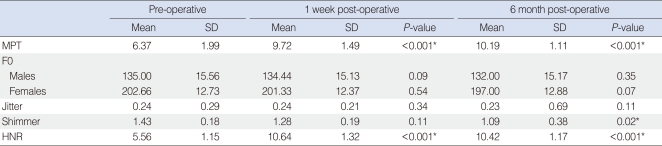
Table 3
Comparison between the pre-operative acoustic voice evaluation of the patients and that at 1 week and 6 months post-operatively
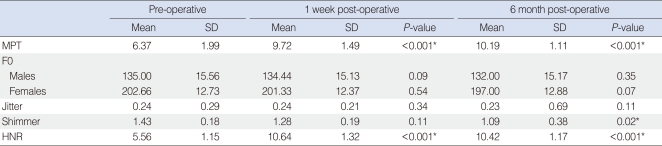

On the other hand, the objective voice evaluation significantly improved post-operatively. Pre-operatively, the average maximum phonation time (MPT) was 6.37 seconds. One week after surgery, the MPT significantly improved to 9.72 seconds (
P<0.05) and to 10.19 seconds after 6 months (
P<0.001) (
Table 3). Similarly, significant improvement was noticed between the pre-operative evaluation and the 1 week and 6 months post-operative evaluation of the HNR (
P<0.001) while shimmer showed significant improvement only at the 6 month follow-up (
P=0.02) (
Table 3). No significant improvement was reported for jitter and F0 in both the male and female patients at the 1 week follow-up visit or the 6 months follow-up visit (
Table 3).
Go to :

DISCUSSION
Different surgical procedures are used for the management of glottal insufficiency resulting from unilateral vocal fold paralysis. These procedures include vocal fold injection, arytenoid adduction and external medialization thyroplasty. However, medialization thyroplasty is considered the most widely used laryngeal framework procedure for achieving adequate glottal closure and particularly for wide glottal gaps (
13). It has been reported that the endoscopic augmentation techniques induce vocal fold stiffness with loss of the mucosal waves (
14). Moreover, there are some advantages of external medialization thyroplasty over other techniques such as the former can be conducted under local anesthesia, and the implant is placed lateral to the inner perichondrium of the thyroid cartilage lamina so the structural integrity of the vocal fold is preserved (
15).
There is a controversy regarding the proper timing for external medialization thyroplasty because of the relative difficulty in determining the type of recurrent laryngeal nerve injury (
16). Therefore, it is recommended in such cases to examine the nerve conduction by performing electromyography to exclude complete nerve degeneration (
17). Partial recovery can be expected in some cases in which the nerve is not completely damaged. However, the extent and the duration of this recovery may vary according to the degree of damage. It is generally advisable to wait for at least 6 months from the onset of the problem before offering medialization surgery (
15). No electromyography was done for the patients in this current study. However, all the patients had the diagnosis of unilateral vocal fold paralysis for an average duration of 9 months. Therefore, there were minimal chances for spontaneous recovery to take place.
Functional voice therapy can successfully restore better voice quality in many patients with unilateral vocal fold paralysis and especially if the glottal gap is not so wide. Medialization thyroplasty is mainly indicated for patients with a large glottal gap and after failure of voice therapy to achieve sufficient glottal closure. Most of the patients included in this current study underwent medialization thyroplasty after receiving voice therapy (20-25 sessions) with no detectable improvement of the voice quality.
Medialization thyroplasty was carried out using autologous cartilage from the nasal septum as an implant. Because of its better tissue tolerability, an autologous cartilage implant is less likely to be rejected or extruded. It can be easily cut and shaped with the scalpel to be easily adjusted into the thyroid cartilage window. The cartilage implant does not need any external fixation as it simply fits and is easily introduced under the edges of the thyroid lamina window. Multiple layers of the cartilage can be inserted according to the required degree of medialization as guided by the intra-operative voice quality. Apart from slight endolaryngeal hematoma that is frequently observed after surgery and this resolves spontaneously with time, there were no major complications in our patients.
Arytenoid adduction is sometimes done by surgeons along with medialization thyroplasty to improve the posterior glottic closure (
18). However, many studies have suggested the importance of arytenoid adduction in improving the objective or subjective outcomes of thyroplasty surgical procedures (
19). Moreover, a recent study has reported no significant difference in the post-operative glottis closure for the patients who underwent only thyroplasty and those who underwent throplasty with arytenoid adduction (
2). In this current study, there was no need for supplementary arytenoid adduction as most of our patients achieved complete glottal closure post-operatively and they were satisfied with their voices. This indicates the minor role of the respiratory glottis in affecting the voice quality of patients following thyroplasty procedures.
On comparing the pre- and post-operative perceptual assessment of the patients' voice quality, there was significant improvement of most of the perceptual parameters, including the overall grade of dysphonia, breathiness and roughness. This improvement was significantly detected at both the 1 week and the 6 months follow-up visits. This indicates that better glottal closure is achieved following medialization thyroplasty and this is reflected by the perceived voice quality.
At the same time, significant improvement was demonstrated between the pre- and post-operative objective assessments of the patients' voices using acoustic analysis. In the current study, MPT showed significant improvement at both the 1 week and the 6 months follow-up evaluations. This could be also explained by the improvement in the glottal closure, less air escaping and better control of the phonatory airflow that the patients achieved post-operatively. Similarly, HNR and shimmer showed significant improvement post-operatively. This indicates a better mechanism for true vocal fold vibration with proper utilization of the aerodynamic forces at the level of the vocal folds, and this is significantly reflected by the acoustic signal of the voice. Moreover, proper vocal folds closure with no glottis gap improved the perceived loudness of the voice (intensity), and so there were lesser values of the amplitude perturbation (shimmer). The improvement in HNR could be mainly explained by the reduction of turbulence noise post-operatively as a result of improved transformation of the aerodynamic energy into acoustic energy after correcting the glottal gap. Comparable perceptual and acoustic results were reported in other related studies (
9,
12,
20,
21).
On the other hand, F0 and jitter did not show significant differences between the pre-operative assessment and the 1 week or the 6 months follow-up visits post-operatively. These findings match those of Lu et al. (
22), and Storck et al. (
7) who found similar acoustic analysis results for their patients who underwent external thyroplasty. This could be explained by the fact that medialization thyroplasty works on adjusting the paralyzed vocal fold position rather than having a direct effect on the length or the tone of the vocal fold.
Although most of the patients in this study reported continuous improvement of the perceptual and acoustic parameters throughout the whole follow-up period, one of the potential limitations of this study is the lack of long-term follow-up for more than 6 months. However, previous animal studies (
23,
24) that used autologous cartilage grafts demonstrated the good tolerability and efficacy of the implanted cartilaginous materials for long term volumetric augmentation of glottis insufficiency and this could extend for up to 3 years.
In conclusion, external medialization thyroplasty using an autologous nasal septal cartilage graft is considered a safe and efficient phonosurgical procedure. It can be used to correct glottal insufficiency in cases of unilateral vocal fold paralysis while preserving the structural integrity of the vocal folds. This technique provides proper positional adjustment of the paralyzed vocal fold with significant improvement in the subjective and objective functional voice outcomes.
Go to :






 PDF
PDF Citation
Citation Print
Print






 XML Download
XML Download