Abstract
Tracheoesophageal fistula (TEF) after prolonged intubation could present as chronic aspiration and could be mistaken as unilateral or bilateral vocal fold palsy, especially when there was combined posterior glottic synechia. We present a case of post-intubation TEF which was successfully treated with tracheal resection and anastomosis with primary esophageal closure. The accompanying posterior glottic web was treated by endoscopic technique of web lysis, with topical application of mitomycin C solution.
Long-term intubation is the cause of the majority of acquired, nonmalignant tracheoesophageal fistulae (TEF). Post-intubation TEF could present as chronic aspiration after intubation, and could therefore be mistaken as unilateral or bilateral vocal fold palsy, especially when there was combined posterior glottic synechia.
Surgical closure of TEF is necessary because spontaneous closure is extremely rare. Due to the variety of surgical options to repair a TEF, including direct closure of the tracheal and esophageal defects with or without pedicled muscle flaps, tracheal closure with an esophageal patch, segmental tracheal resection, and anastomosis with esophageal closure and esophageal diversion, the timing and type of repair are still being debated.
We present a case of post-intubation TEF which was successfully treated with tracheal resection and anastomosis, using primary esophageal closure and endoscopic lysis for the accompanying posterior glottic web. Approval for this case report was granted by the Institutional Review Board of the author's hospital (No. 20090428/06-2009-54/83).
A forty four-year-old woman was referred from a local general hospital for dyspnea and aspiration on eating. She had history of drug intoxication from a suicidal attempt 2 months prior. At that time she had been intubated and had a gastric lavage, after which she had a nasogastric feeding tube. A tracheotomy was necessary because of prolonged intubation (longer than 20 days). During the hospital stay her T-cannula was recurrently obstructed by crust and secretion and her symptoms seemed to be relieved after T-cannula change. On endoscopic examination, performed by an ENT resident, it was apparent that the right side of her vocal fold seemed to be paralyzed, and injection laryngoplasty was initially planned to solve her aspiration problem.
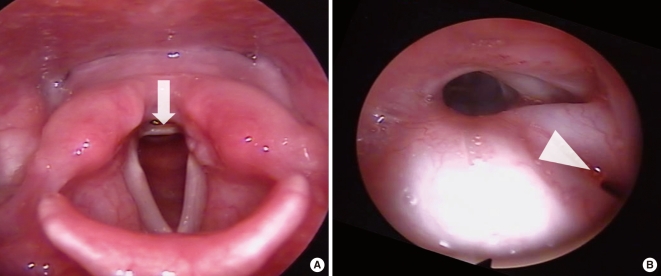
On detailed examination of her airway, however, a glottic scar band was found at the posterior glottis, which seemed to be the cause of the limited mobility of her right vocal fold (Fig. 1A). Moreover, there was a TEF on the left posterior wall of the trachea, 1 cm above the level of tracheostoma (Fig. 1B). We confirmed that it was a TEF by verifying leakage through the fistula on oral intake of water. Surgical intervention was planned for her problems.
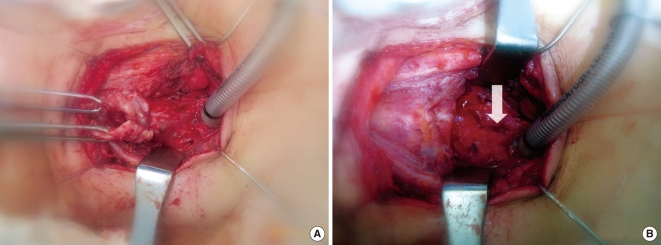
Through an anterior cervical horizontal incision, the skin, subcutaneous fat, and platysma were elevated as one layer and the flap was raised to the level of the suprahyoid region. The sternohyoid muscles were divided in the midline and the thyroid isthmus was divided and ligated to expose the anterior surface of the trachea. The trachea was freed circumferentially only above and below the site of the fistula, and care was taken to maintain the dissection as close as possible to the outer tracheal surface, thereby avoiding injury to the recurrent laryngeal nerves and to preserve the lateral blood supply to the unresected trachea. The tracheal resection was done from the 2nd to the 4th tracheal rings (2.5 cm in length), and the esophageal fistula was found to be a slit-like shape, 1 cm in length (Fig. 2). It is of paramount importance to assure that the tracheal cut end has a normal diameter and mucosal appearance. The opening of the airway gave complete exposure to the esophageal defect. The edges of the esophageal defect were debrided and a two-layer closure was was made over a nasogastric tube.
After closure of the esophageal defect, the trachea was reconstructed via interrupted 4-0 Vicryl sutures with 4 mm interval between stitches. Before completion of the anastomosis, the distal ventilation system was removed and a new endotracheal tube advanced beyond the anastomosis line. Excessive anastomotic tension was avoided by performing laryngeal and tracheal release. The wound was then filled with sterile saline solution to test the anastomosis. The cervical incision was closed by covering the anastomotic line with the thyroid isthmus and by approaching the linea alba cervicalis. Two soft multi-holed drain catheters were placed. Soon after, the larynx was evaluated with suspension laryngoscopy. Under microscopic magnification the scar band causing posterior glottic synechia was resected with micro surgical instruments. Topical 0.04% mitomycin C solution was applied with 3 mm-sized cotton balls around the interarytenoid area, to prevent synechia or scarring.
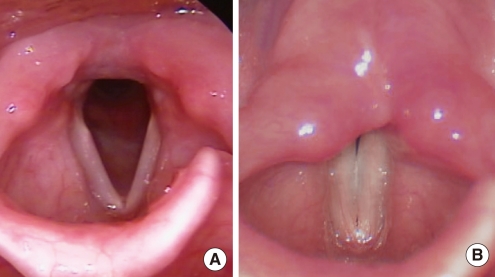
The patient was moved to ward via recovery room with her intubation tube in situ. Extubation was done early the following morning. There was no sign of airway obstruction or aspiration. She recovered both her voice and oral diet. On post-1 year follow-up visit, she had no dyspnea or aspiration and both vocal folds were freely mobile (Fig. 3).
Surgical repair for TEF can be accomplished by simple division and closure of the fistula (1). The lateral approach used for the simple division and repair is limited in that it gives a limited and unilateral exposure of the fistulous tract, and requires identification of the recurrent laryngeal nerve (1, 2). Identification of the fistulous tract may not be simple and usually requires a more extensive dissection than expected. Moreover, the separation of the tracheal and esophageal lines requires esophageal rotation and thus esophageal devascularization, which can result in late tracheal stenosis at the level of the repair or muscle interposition. In addition, there could be a combined tracheostoma, which should be closed by secondary healing, if it were not resected with TEF closure simultaneously (1). Therefore, tracheal resection and anastomosis with primary esophageal closure has some advantages over simple division and closure of the fistula: 1) it is a one-stage procedure, 2) easy visualization and division of the esophageal fistula site, 3) reliable result despite the risk of anastomosis site problems (1-3). In this case, we could manage the patient successfully by tracheal resection and end-to-end anastomosis with primary esophageal closure 1) in one stage, 2) without identification of recurrent laryngeal nerve, and 3) with early rehabilitation. Except for the possible morbidity related to tracheal resection and anastomosis, including disruption of anastomosis, emphysema or pneumomediastinum caused by air leakage, this procedure could be one of the best options for acquired TEF after prolonged intubation (1).
Prolonged intubation caused various problems such as glottic or subglottic stenosis, TEF, vocal fold paralysis, hypertrophic scar, and so on (4-6). Because these complications could be brought-on at the same time, clinicians should be alert to find all the problems in the aerodigestive tract comprehensively (4). Therefore, thorough endoscopic and imaging work-up should precede the initial surgical intervention. In this case, initial the misdiagnosis was idiopathic unilateral vocal fold paralysis, which was based on vocal fold immobility on endoscopic examination and chronic aspiration on medical history.
Posterior glottic stenosis is, for clinicians, a troublesome and hard to solve complication after prolonged intubation (6-8). Nd-YAG laser and mitomycin C shows good result for posterior glottic stenosis after prolonged intubation (9, 10). The posterior glottic scar band in this case was easily resolved by endoscopic resection and topical mitomycin C application.
Tracheal resection and anastomosis with primary esophageal closure was successfully used to treate TEF occurring after prolonged intubation, with, and endoscopic technique of web lysis for the accompanying posterior glottic web. Careful evaluation for combined complications from prolonged intubation is mandatory and should be settled simultaneously.
References
1. Macchiarini P, Verhoye JP, Chapelier A, Fadel E, Dartevelle P. Evaluation and outcome of different surgical techniques for postintubation tracheoesophageal fistulas. J Thorac Cardiovasc Surg. 2000; 2. 119(2):268–276. PMID: 10649202.

2. Chappell VL, Heck HA Jr. Repair of large, iatrogenic, tracheo-esophageal fistulae. Ann Thorac Surg. 2007; 2. 83(2):705–706. PMID: 17258028.

3. Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am. 2003; 5. 13(2):271–289. PMID: 12755313.

4. Anand VK, Alemar G, Warren ET. Surgical considerations in tracheal stenosis. Laryngoscope. 1992; 3. 102(3):237–243. PMID: 1545649.

5. Grillo HC, Donahue DM, Mathisen DJ, Wain JC, Wright CD. Postintubation tracheal stenosis: treatment and results. J Thorac Cardiovasc Surg. 1995; 3. 109(3):486–492. PMID: 7877309.
6. Hoasjoe DK, Franklin SW, Aarstad RF, Day TA, Stucker FJ. Posterior glottis stenosis mechanism and surgical management. Laryngoscope. 1997; 5. 107(5):675–679. PMID: 9149173.
7. Rovo L, Jori J, Brzozka M, Czigner J. Minimally invasive surgery for posterior glottic stenosis. Otolaryngol Head Neck Surg. 1999; 7. 121(1):153–156. PMID: 10388899.

8. Yeh CM, Chou CM. Early repair of acquired tracheoesophageal fistula. Asian Cardiovasc Thorac Ann. 2008; 8. 16(4):318–320. PMID: 18670027.

9. Roh JL, Yoon YH. Prevention of anterior glottic stenosis after transoral microresection of glottic lesions involving the anterior commissure with mitomycin C. Laryngoscope. 2005; 6. 115(6):1055–1059. PMID: 15933520.

10. Gallivan GJ. Bilateral vocal fold posterior glottic/subglottic stenotic web resected with contact tip Nd-YAG laser. J Voice. 2002; 9. 16(3):415–421. PMID: 12395994.

Fig. 1
Telescopic findings. (A) Posterior glottic web is found between the arytenoids (arrow). (B) Tracheoesophageal fistula is seen on the left posterior wall of the trachea, 1 cm above the level of tracheostoma (arrowhead).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download