Abstract
Objectives
To evaluate that the cross-sectional area of the air space in the Eustachian tube (ET) on computed tomography (CT) images could be useful for predicting the postoperative aeration of the middle ear.
Methods
The patient group consisted of 80 patients (80 ears) with chronic otitis media and who underwent middle ear surgery from 2006-2007 and who were followed up for more than 1 yr. The control group consisted of 100 ears of 50 individuals with normal tympanic membranes and who underwent CT for other causes (such as tinnitus or hearing loss). The largest cross-sectional areas of the aerated ET were measured on the coronal images of the temporal bone CT by a single otologist using the computer-based "Region of Interest" picture archiving and communications system. The patient group was divided into two subgroups, 1) those with good postoperative aeration and 2) those with poor postoperative aeration. The largest cross-sectional areas of the aerated ETs were compared between the patients and the controls, and between the patients with good aeration and the patients with poor aeration.
Results
The mean cross-sectional areas significantly differed between the patient group and the control group, and between the good and poor aeration subgroups (P<0.05 each). The mean area of the poor aeration subgroup was smaller than that of the control group (P<0.05), but the mean area of the good aeration subgroup did not significantly differ from that of the controls.
The Eustachian tube (ET) is of great importance in chronic otitis media (COM), both pathogenetically and surgically, in that dysfunction of the ET is an important cause of middle ear disease (1). Among the methods commonly used to measure the ET's ventilatory function are tympanometry, the Valsalva test, the Toynbee test and the nine-step test, but these methods have limited utility in patients with perforated tympanic membranes (TM). If the TM is not intact, then the preoperative ET function can be evaluated using the inflation-deflation manometric test, but this is an assessment of tubal patency only and not function, and failure to inflate the middle ear does not necessarily indicate a lack of patency of the ET (2). Furthermore, the small pressure shifts that are characteristic of inflation-deflation manometric tests, coupled with the potential for instrument error, severely limit the use of these tests in obtaining reliable indices of the tubal function (3).
Slow motion video endoscopy may be useful in detecting pathologic changes in the ET mucosa, regardless of the condition of the TM (4). If the TM is perforated, then transtympanic endoscopy can be used to evaluate the tympanic orifice of the ET. Yet these methods require trained and skilled technicians, as well as special equipment. Moreover, endoscopy has been found unsuitable for assessments around the isthmus owing to its poor resolution and the relatively large diameter of the endoscope.
Radiologic evaluation, and especially computed tomography (CT), is essential when preoperatively evaluating the middle ear and mastoid. The recently developed multiplanar reconstruction technique has made it possible to obtain images parallel or perpendicular to the long axis of the ET (5). This technique is useful for better understanding the ET and ET-related diseases such as a patulous ET (6). A horizontal CT system, in which patients are in the sitting position, and not the recumbent position, can be used for more physiologically relevant imaging (7, 8). Nevertheless, axial and coronal temporal bone CT (TBCT) imaging is currently the most commonly used tool for preoperative anatomic evaluation, including evaluation of the ET, in patients with COM. But there were few studies that have assessed ET patency on conventional axial and coronal CT images and its correlation with the postoperative results. Because conventional TBCT can visualize only the bony portion of the ET, while opening failures usually occur in the cartilaginous portion, the value of preoperative ET evaluation using TBCT is unclear. So, we assessed whether the cross-sectional area of the ET, as measured on CT images, can be useful for predicting postoperative middle ear aeration.
The patient group consisted of 80 patients (80 ears) with COM, but they were without any otologic anomaly or temporal bone trauma history, and they underwent middle ear surgeries from 2006-2007 in a tertiary referral hospital and they were followed up for more than 1 yr. The 80 patients consisted of 37 males and 43 females with a mean age of 46.7±12.4 yr. The control group consisted of 100 ears of 50 individuals (44 males and 56 females; mean age, 41.8±13.8 yr) with normal TMs and they underwent CT for other causes (such as tinnitus or hearing loss).
For the evaluation of postoperative middle ear aeration, the COM group was divided into two subgroups based on the results of otoscopy and tympanometry 1 yr after surgery: a good aeration subgroup that consisted of patients with normal TMs seen on otoscopic examination and the A type on tympanometry, and a poor aeration group that consisted of patients with adhesive TMs on otoscopic examination or the B/C type on tympanometry.
The axial view TBCT was performed with the patients in the supine position, and the coronal view TBCT was performed with the patients in the prone position with full extension of the neck. Contiguous axial and coronal images at 1.25-mm thickness were obtained using a Lightspeed plus multidetector axial CT system (GE, Milwaukee, WI, USA). The axial CT examinations were performed at 120 kV and 240 mAs, the field of view was 18 cm with an imaging matrix of 512×512 pixels and the slice increment was the same as the slice thickness.
Among a few slices of the coronal images, the one showing the largest air space area of the ET was chosen and the area was measured. All the area measurements were taken by a single otologist using the computer-based "Region of Interest" picture archiving and communications system, and the measurements were done on a 512×512 pixel image magnified 7 times under a window level of 350 housefield unit (HF) and a window width of 3,000 HF. For each patient, the largest air space area was determined as the mean of two measurements (Fig. 1).
The largest cross-sectional areas of the air space in the ET lumen were compared between the patients and the controls and between the good and poor aeration subgroups by oneway ANOVA. Using logistic regression analysis, we analyzed the correlation between the cross-sectional area and postoperative middle ear aeration. The optimal cut-off value predicting good postoperative middle ear aeration was estimated by a receiver operating characteristic curve analysis.
The mean largest cross-sectional area of the aerated ET of the COM patients was 6.02±4.34 mm2 (range, 0 to 16.56 mm2) and that of the controls was 9.16±2.65 mm2 (range, 3.21 to 15.94 mm2), with the former being significantly smaller than the latter (P<0.05). Among the 80 patients, 47 showed good postoperative middle ear aeration (a normal TM and A type on tympanometry), whereas 33 showed poor postoperative middle ear aeration (an adhesive TM or B/C type on tympanometry). The mean largest cross-sectional area of the aerated TM was significantly lower in the patients with poor postoperative aeration (3.73±4.05 mm2) than that in the patients with good postoperative aeration (7.62±3.81 mm2) and the controls (9.16±2.65 mm2) (P<0.05 each), but the mean largest cross-sectional area of the aerated TM of the good aeration subgroup did not significantly differ from that of the controls (P>0.05) (Fig. 2).
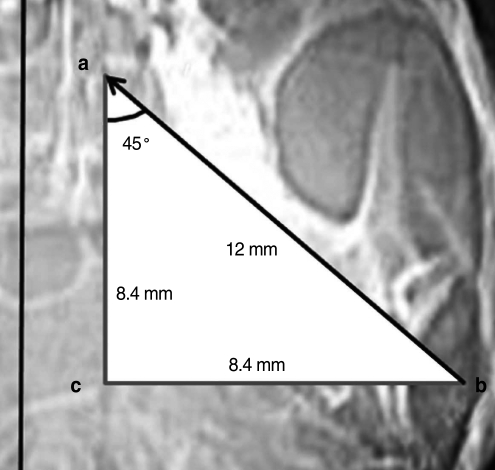
By the logistic regression analysis, the largest cross-sectional area of the aerated ET of the COM patients was positively correlated with postoperative middle ear aeration (odds ratio, 0.77; P<0.05) (Fig. 3). The optimal cut-off value for predicting good postoperative middle ear aeration was estimated to be 5.53 mm2 by the receiver operating characteristic curve analysis. The sensitivity and specificity of this cut-off value were 78.7% and 70.6%, respectively (Fig. 4, Table 1).
These analyses indicate that the cross-sectional area of the ET on the preoperative coronal images may be useful for predicting the postoperative condition of the tympanic cavity. We cannot know the patency of the cartilaginous portion and the functional problems related to the opening and closing mechanism of the ET. However, the largest cross-sectional area of the ET measured in the present study reflects the narrowing caused by middle ear pathology, such as cholesteatoma and granulation tissue, or inflammatory mucosal swelling, although this area is also influenced by the original size of the bony frame.
Of the 33 patients in the poor aeration group, 10 had areas exceeding the cut-off value (5.53 mm2), with 3 having areas larger than the mean of the controls. This may be due to cartilaginous opening failure of the ET, despite the relatively wide lumen of the bony portion. In contrast, of the 47 patients in the good aeration group, 10 had areas smaller than the cut-off value. This may be due to the properly working gas exchange function in the mastoid or in the tympanic cavity, although the patency of the ET was poor. The ventilation and pressure of the middle ear are regulated not only by the ET, but also by gas exchange through the middle-ear or the mastoid mucosa. The findings in these 10 patients may also be related to their surgery, which resulted in removal of pathology from the tubal orifice and improvement of the inflammation of the middle ear and the tubal mucosa.
In most patients, COM arises from secretory otitis media, with ET dysfunction playing a major role in the pathogenesis of the secretory otitis media. The suggested succession of events starts with long-term poor ET function and secretory otitis, and this is followed by atrophy of the TM with or without retraction, perforation of the atrophic TM due to acute otitis media (AOM) or trauma, poor healing of the atrophy and permanent perforation, and possibly with secondary infection leading to active infection of the middle ear mucosa with deterioration of the tubal function (1). ET dysfunction can be caused by an opening failure or an obstructive mechanism. The most frequent cause of ET dysfunction is the inability, and especially of the cartilaginous portion, to open during swallowing, although this type of dysfunction does not necessarily correlate with the prognosis of middle ear disease (9, 10). Indeed, in the subjects with unilateral middle ear disease, there were no differences in the abilities of their healthy and diseased ears to equalize pressure (11). In addition, no correlation was observed between each of the three middle-ear pressure-regulation functions, including positive and negative pressure-equalization (via the inflation-deflation test) and mastoid aeration, and the outcome of type-I tympanoplasty. However, when all three parameters were poor, which indicated a complete mechanical obstruction of the ET and this included its transmucosal gas exchange dysfunction, the probability of a poor outcome was significantly higher (9). Mechanical obstruction of the ET blocks not only its ventilation function, but also its clearance function, resulting in the retention of fluid or bacterial infection of the middle ear mucosa (1, 9). Because the absence of the clearance function of the ET is critical, obstruction has a more serious effect on patients with COM or secretory otitis media (9, 12). ET obstruction can occur at both ends, whereas in most patients with COM it occurs around the tympanic orifice, and this is possibly due to middle ear pathology or edema of the tubal mucosa.
In the present study, we chose the pretympanic portion as the measured target among the 6 segments of the ET: the pharyngeal portion, the midportion, the near of the isthmus portion, the isthmus portion, the post-isthmus portion and the pretympanic portion (13). We did this because we considered that the pretympanic portion is not only the largest one in the entire ET, but it is also the area most affected by middle ear pathology. Therefore, we measured the cross-sectional area on the coronal section showing the largest air-space for reducing technical errors. Because the pretympanic portion is affected by mucosal swelling in patients with middle ear disease, our measurements of the cross-sectional area excluded the mucosal layer. Indeed, a histopathologic study reported that the percentage of the luminal circumference occupied by the inflammatory reaction in each segment increased from the pharyngeal portion (42%) to the pretympanic portion (62%), and the maximal augmentation of the mean mucosal thickness increased from the pharyngeal portion (78%) to the pretympanic portion (259%) (14). Mucosal swelling of the pretympanic portion is a major factor for differentiating patients with OM from normal subjects.
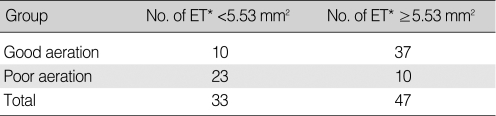
On the coronal view, it was easy to find the lumen of the pretympanic segment, where it connects with the bulging of the tensor tympani muscle on its roof and it is located in the lateral side of the internal carotid artery and cochlea. However, a slice showing an air-space above the level of the tensor tympani muscle was regarded as being part of the tympanic cavity rather than the pretympanic portion of the ET. The average anteroposterior distance of the bony ET in normal adults was estimated to be 8.4 mm; the average length of the bony ET was estimated to be 12 mm and the angle of the long axis of the ET to the sagittal plane was estimated to be about 45° (Fig. 5) (15). Considering that the contiguous coronal images were 1.25-mm thick, we theoretically should be able to visualize the bony portion of the ET in seven slices. Using the sum of the measurements of all seven cross-sectional areas, it may be possible to estimate the entire volume of the bony ET. Practically, however, this would be difficult because the number of slices showing the ET can vary from five to seven. Moreover, the post-isthmus portion of the ET, which occupies a very small air space, increases the risk of measurement error. These measurements failed to show a significant difference of the air space between the control ears and the stenotic ears, suggesting that measurements from CT images may be unreliable (5). We were unable to utilize the axial views because the tympanic orifice of the ET is continuously connected to the tympanic cavity, and this makes it difficult to determine the lateral border of the ET facing the tympanic cavity.
While using the computer-based "Region of Interest" tool, we attempted to keep the HF within 2 standard deviations from the mean value obtained in a pilot study of the control group (-772.4±39.6). We thought that this would be helpful in measuring the precise area of the pure air space without soft tissue. If the HF was too high, then the cross-sectional aeration area might be overestimated because the measured portion could contain a small part of the mucosa.
We found that the mean cross-sectional area of the aerated ET in the COM patients (6.02±4.34 mm2) was smaller than that of the normal individuals (9.16±2.65 mm2), and this is in agreement with the findings of a histopathologic study using the temporal bone from children under 2 yr old (13). In that study, the mean cross-sectional area of the ET lumens of the inflamed temporal bone was significantly smaller than that of the noninflamed bones only in the pretympanic portion, whereas the differences were of borderline significance in the other bony portions and the differences were not significant in all the cartilaginous portions (13). In that study, the minimal size of the pretympanic portion was about 2 mm2, whereas 15 of our patients (12 in the poor aeration subgroup and 3 in the good aeration subgroups, but none of the controls) had a minimal size of 0 mm2. These differences may be due to the differences of the disease states (AOM vs. COM), age (infants vs. adults) and the measured objects (temporal bone slides vs. CT images). Another histological study that used 200 temporal bones of adults found that the mean height and width of the tympanic opening of the ET were 5.20 mm and 3.95 mm, respectively (16). Assuming that this orifice is rectangular, the mean area was calculated to be 20.54 mm2. One reason for the discrepancy with our measured area may be that we measured the air space with excluding the mucosal thickness, whereas the earlier study measured the bony frame of the ET with including the mucosal layer. Moreover, because the tympanic portion is not exactly rectangular in shape, the calculated area (20.54 mm2) may have been overestimated. Furthermore, the measured cross-sectional area in our study may not have been the exact orifice occupying the largest area due to the 1.25-mm thickness interval between the slices.
The limitation of this study was the non-inclusion of the postoperative hearing results. This study enrolled patients with various types of COM (such as cholesteatoma or simple TM perforation) and who underwent various types of surgical procedures (such as type I-tympanoplasty or tympanization). Therefore, we measured middle ear aeration as the factor that represents the postoperative results. To utilize a strict standard of middle ear aeration, we defined good aeration as only when the TM configuration and tympanometry results were both positive, otherwise the aeration was regarded as poor. In the present study, we did not consider factors that can influence the mucosal thickness, the severity of the preoperative inflammation, the duration of antibiotic therapy and treatment with combinations of medicine, although these variables should all be considered when making precise comparisons of the cross-sectional areas of aerated ETs.
We evaluated whether the measurement of the cross-sectional area of the ET on the coronal CT images could predict postoperative middle ear aeration. This cross-sectional area of the air space in the pretympanic portion of the ET was chosen as the parameter that reflects the mucosal swelling of the bony ET in patients with COM. We observed a positive correlation of this area with postoperative middle ear aeration. Our findings indicate that the evaluation of the ET on the preoperative TBCT in patients with COM may predict the postoperative results.
References
1. Tos M. Importance of eustachian tube function in middle ear surgery. Ear Nose Throat J. 1998; 9. 77(9):744–747. PMID: 9787517.

2. Bluestone CD. Cummings CW, Flint PW, Harker LA, Haughey BH, Richardson MA, Robbins BW, editors. Anantomy and physiology of the Eustachian tube. Cummings otolaryngology: head and neck surgery. 1998. 3rd ed. Philadelphia: Elsevier Mosby Inc;p. 3003–3025.
3. Riedel CL, Wiley TL, Block MG. Tympanometric measures of eustachian tube function. J Speech Hear Res. 1987; 6. 30(2):207–214. PMID: 3599952.

4. Poe DS, Abou-Halawa A, Abdel-Razek O. Analysis of the dysfunctional eustachian tube by video endoscopy. Otol Neurotol. 2001; 9. 22(5):590–595. PMID: 11568663.

5. Yoshida H, Takahashi H, Morikawa M, Kobayashi T. Anatomy of the bony portion of the eustachian tube in tubal stenosis: multiplanar reconstruction approach. Ann Otol Rhinol Laryngol. 2007; 9. 116(9):681–686. PMID: 17926591.

6. Yoshida H, Kobayashi T, Takasaki K, Takahashi H, Ishimaru H, Morikawa M, et al. Imaging of the patulous Eustachian tube: high-resolution CT evaluation with multiplanar reconstruction technique. Acta Otolaryngol. 2004; 10. 124(8):918–923. PMID: 15513527.

7. Yoshida H, Kobayashi T, Morikawa M, Hayashi K, Tsujii H, Sasaki Y. CT imaging of the patulous eustachian tube: comparison between sitting and recumbent positions. Auris Nasus Larynx. 2003; 5. 30(2):135–140. PMID: 12753983.
8. Kikuchi T, Oshima T, Ogura M, Hori Y, Kawase T, Kobayashi T. Three-dimensional computed tomography imaging in the sitting position for the diagnosis of patulous eustachian tube. Otol Neurotol. 2007; 2. 28(2):199–203. PMID: 17255887.

9. Takahashi H, Sato H, Nakamura H, Naito Y, Umeki H. Correlation between middle-ear pressure-regulation functions and outcome of type-I tympanoplasty. Auris Nasus Larynx. 2007; 6. 34(2):173–176. PMID: 17055205.

10. Bluestone CD, Hebda PA, Alper CM, Sando I, Buchman CA, Stangerup SE, et al. Recent advances in otitis media: 2. Eustachian tube, middle ear, and mastoid anatomy; physiology, pathophysiology, and pathogenesis. Ann Otol Rhinol Laryngol Suppl. 2005; 1. 194:16–30. PMID: 15700932.
11. Magnuson B. Tubal opening and closing ability in unilateral middle ear disease. Am J Otolaryngol. 1981; 8. 2(3):199–209. PMID: 7283063.

12. Bluestone CD. Studies in otitis media: Children's Hospital of Pittsburgh-University of Pittsburgh progress report-2004. Laryngoscope. 2004; 11. 114(11 Pt 3 Suppl 105):1–26. PMID: 15514559.

13. Sade J, Luntz M. Eustachian tube lumen: comparison between normal and inflamed specimens. Ann Otol Rhinol Laryngol. 1989; 8. 98(8 Pt 1):630–634. PMID: 2764447.

14. Sade J, Luntz M, Berger G. The eustachian tube profile in children: a quantitative histopathological study of the ET lumen and mucosal lining involvement in acute and secretory otitis media. Adv Otorhinolaryngol. 1988; 39:18–36. PMID: 3394566.
15. Prades JM, Dumollard JM, Calloc'h F, Merzougui N, Veyret C, Martin C. Descriptive anatomy of the human auditory tube. Surg Radiol Anat. 1998; 20(5):335–340. PMID: 9894313.

16. Djeric D, Savic D. Anatomical variations and relations of the bony portion of the eustachian tube. Acta Otolaryngol. 1985; May–Jun. 99(5-6):543–550. PMID: 4024903.
Fig. 1
The coronal computed tomography image captured during measurement of the largest cross-sectional areas of the aerated Eustachian tube using the "Region of Interest" picture archiving and communications system. The "area" circumscribed by the black-colored curved line was determined by automatic calculation, whereas the "mean" was the average number of Housefield unit of the corresponding region and "SD" was the standard deviation in Housefield unit.
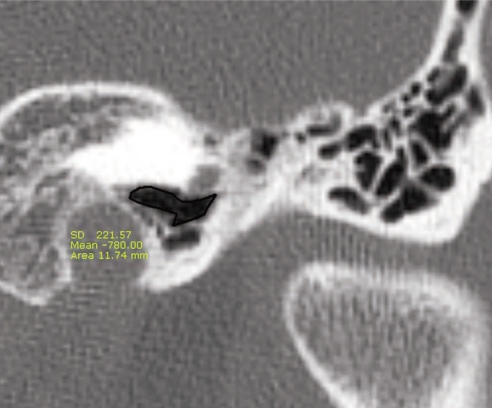
Fig. 2
Measurements of the largest cross-sectional areas of the aerated Eustachian tube (ET). We observed significant differences between the poor aeration subgroup and the good aeration subgroup (*P<0.05) and between the poor aeration subgroup and the control group; by contrast, the areas of the good aeration subgroup and the control group did not significantly differ. †Good aeration group: the patients showing normal tympanic membranes and A type on tympanometry after surgery; ‡Poor aeration group: the patients showing adhesive tympanic membranes or B/C on tympanometry after surgery. The error bar means SD.
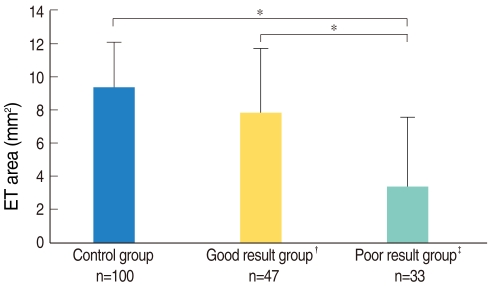
Fig. 3
The correlation between the largest cross-sectional areas of the aerated Eustachian tube (ET) and the postoperative middle ear aeration (A), and the logit transformation of the postoperative middle ear aeration (B). It means that the largest cross-sectional areas of the aerated Eustachian tube are related with the postoperative middle ear aeration. The odds ratio was 0.772 (P=0.000).
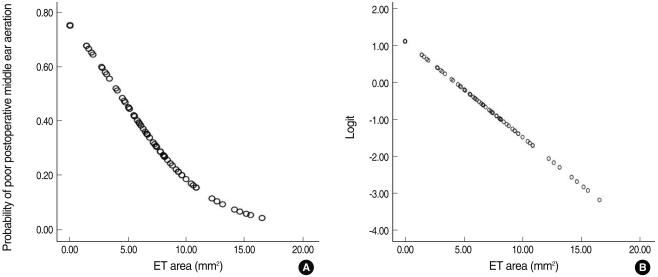
Fig. 4
Receiver operating characteristic (ROC) curve for the largest cross-sectional area of the aerated Eustachian tube for predicting good postoperative middle ear aeration. The cut-off value for differentiating good aeration from poor aeration was estimated to be 5.53 mm2 (circle).
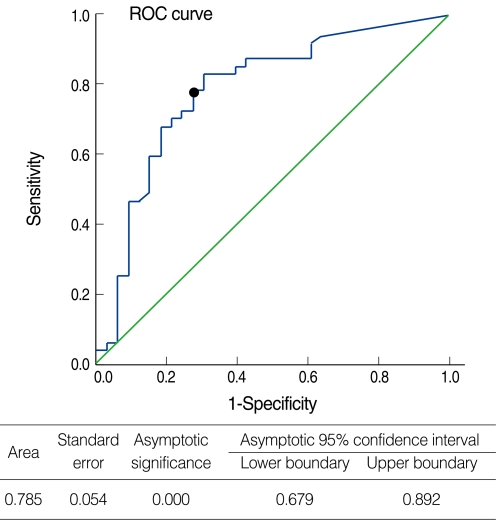
Fig. 5
Eustachian tube (ET) measurements on the coronal view of temporal bone CT. The anteroposterior distance (a-c) of the bony ET was calculated to be 8.4 mm from the average length of the bony ET (a-b) in a normal adult (12 mm), and the angle of a-b to the sagittal plane was about 45°. a: midpoint of the medial border of the bony ET; b: midpoint of the lateral border of the bony ET; c: imaginary point of intersection where the two lines from a and b.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download