This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
These days, the main injection laryngoplasty technique is cricothyroid (CT) approach. However, patients who have previously undergone other neck treatments, such as thyroidectomy or neck dissection have distorted anatomical landmark makes this approach more difficult. The aim of this study is to determined the efficiency of transcartilaginous (TC) approah as compared with CT approach for unilateral vocal fold paralysis patients, especially for previously neck treated patients.
Methods
From March 2005 to February 2008, 137 consecutive injection laryngoplasties were performed in patients with unilateral glottic insufficiency. Percutaneous injection was performed under local anesthesia into the vocalis muscle, using disposable 25 G 4 cm long needles through the cricothyroid membrane or directly through the thyroid cartilage. Of the 137 patients, 124 completed acoustic, perceptual, stroboscopic, and subjective evaluations prior to the injection and at 3 months after the injection.
Results
In the 124 patients, the CT and TC approaches were used in 94 and 30 patients, respectively. Acoustic and perceptual parameters (GRBAS, MPT, jitter, shimmer), voice handicap index, and grades of mucosal waves and glottic closure were significantly improved after the injection in both the CT and TC groups (P<0.05). Only two patients (6.6%) had penetration difficulties, because of ossification of the thyroid cartilage. The overall success rates of the CT and TC approaches were 86.2%, 93.3%, respectively. However, the success rate of the TC approach in patients who had previously undergone neck treatments was significantly higher than that of the CT approach (100% vs. 65% P<0.05).
Conclusion
Based on the preliminary results of this trial, injection laryngoplasty using a TC approach was an effective alternative to the CT approach, especially in patients who had previously undergone neck surgeries.
Go to :

Keywords: Injection laryngoplasty, Thyroid cartilage, Vocal cord paralysis
INTRODUCTION
In recent years, injection laryngoplasty techniques have regained popularity as a means to manage unilateral vocal cord paralysis (
1), because they are easier and less invasive than conventional medialization thyroplasty and may provide equally durable and effective results (
2). There are several routes to reach the vocal fold, such as the transoral, transnasal, and transcutaneous routes (
3,
4). For the transcutaneous route, there are various alternatives, such as through the cricothyroid membrane, thyrohyoid membrane, and directly through the thyroid cartilage. In Korea, the cricothyroid membrane (CT) approach is the most common (
5), because it makes less dead space and there is no leakage from the needle puncture site. However, the direction of the needle is not parallel but is oblique to the vocal fold, making it technically difficult to control the exact depth and location during the injection even for a skilled surgeon (
6). Additionally, in patients with obesity, a short neck, or previous neck treatment, such as neck dissection or thyroidectomy, the external laryngeal landmark may be obscured by fibrotic wound healing, making the CT approach injection procedure more difficult. In contrast to the CT approach, the transcartilaginous (TC) approach is an easier method for controlling the depth and location of the targeted vocal fold, because the direction of the needle is parallel to the vocal fold (
7) (
Fig. 1). We believe that this approach can be a useful alternative to the CT approach for unilateral vocal cord paralysis patients, especially for patients who have previously undergone other neck treatments. This report describes a prospective study to determine the utility of the TC approach injection laryngoplasty technique, compared with the CT approach.
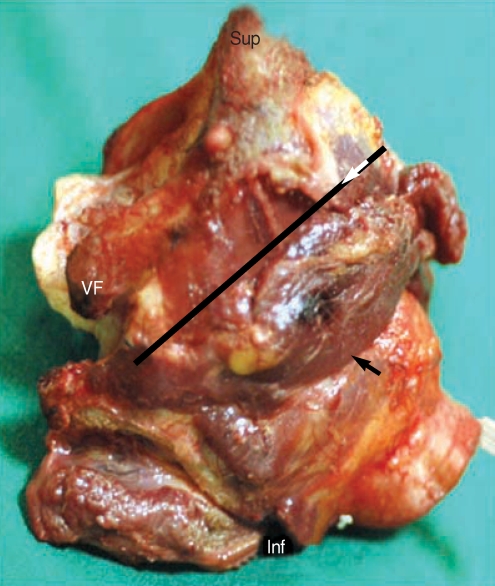
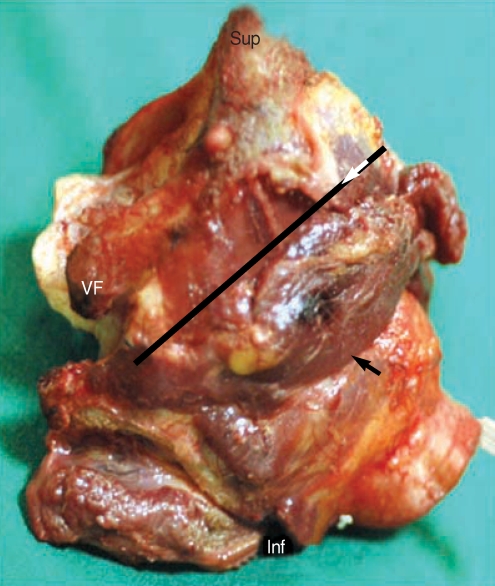 | Fig. 1Demostration of approach direction of cricothyroid (CT) and transcartilaginous (TC) approach in a human cadaveric larynx. Note that direction of needle is parallel to the vocal fold in TC approach but is oblique in CT approach. Long black arrow means an approach direction of CT method. Short white arrow means an approach direction of TC method. VF: vocal fold; Sup: superior; Inf: inferior. 
|
Go to :

MATERIALS AND METHODS
Patients
Of 137 consecutive patients with unilateral vocal cord paralysis, 124 patients were enrolled. They received injection laryngoplasty between March 2005 and February 2008 at the Department of Otolaryngology - Head and Neck Surgery, Soonchunhyang University Bucheon Hospital. Of the patients, 10 were excluded for incomplete follow-up data (9 CT approach, 1 TC approach), and three for an inadequate observation period (3 TC approach).
We selected the approach of injection laryngoplasty according to the time period. From March 2005 to January 2007, we used the CT approach as a primary injection laryngoplasty approach. After that time, we used the TC approach as a primary approach instead of CT approach.
Our institutue apply several biocompatible filler as a injection laryngoplasty material, we used the polyacrylamide hydrogel (Aquamid®, Ferrosan AS, Copenhagen, Denmark) for a permanent purpose, while hyaluronic acid derivatives (Rofilan®, Rofil medical international, Breda, Netherland) for a temporary purpose.
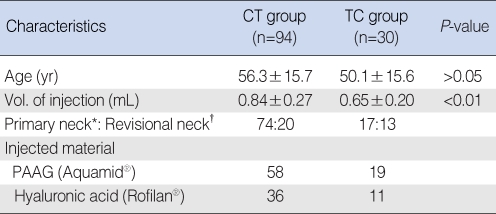
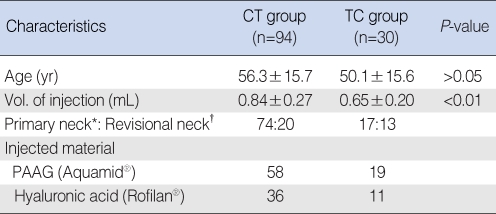
Finally, the study group included 94 CT approach patients (CT group) and 30 TC approach patients (TC group), with 91 being primary neck patients and 33 having undergone previous neck treatments. The mean age was 55.9±15.9 yr (range, 15 to 88 yr). Demographic information and patient characteristics are shown in
Table 1. The study design was approved by the Institutional Review Board.
Table 1
Patients' demographics of CT and TC group (N=124)

Objective voice evaluation
Acoustic and aerodynamic analyses were conducted prospectively, prior to injection, and at three months after the injection by single speech language pathologist. For the acoustic analyses, each patient sat in a quiet room wearing a microphone (AKG C410, AKG Acoustics, Vienna, Austria) at a constant 3-cm distance from the mouth. Sustained 3-s /a /-like phonations were recorded, and jitter and shimmer were analyzed using the Dr. Speech ver. 4.0 (Tiger DRS Inc., Seattle, WA, USA). For aerodynamic analyses, the maximal phonation time was calculated. Each patient sustained /a/ vowel phonations for as long as possible over three trials.
Subjective voice evaluation
Perceptual voice evaluations were conducted using the GRBAS rating scale. Professional speech language pathologists evaluated voice quality, using the GRBAS scale (overall grade of hoarseness, roughness, breathiness, asthenia and strain), focusing, in particular, on overall grade of dysphonia (G) and breathiness (B) (0=normal; 1=slight disturbance; 2=moderate disturbance; and 3=severe disturbance). A 10-point visual analog scale (VAS) was used by the patients, who self-rated their voice function and the degree of aspiration independently (0=normal voice/no aspiration problems; 10=worst voice/maximal aspiration problems), to evaluate subjective voice improvement and aspiration status. For stroboscopic evaluation (Rhinolaryngeal stroboscope 9100, kayPENTAX, Lincoln Park, NJ, USA), mucosal waves and glottic closure were analyzed. For practical purposes, we rated the mucosal wave of vocal fold vibration and the glottic closure independently using a fourpoint grading (0=no wave, severe posterior glottic gap exceeding 3 mm during phonation; 1=marked decreased mucosal wave, moderate posterior glottic gap between 2 and 3 mm during phonation; 2=slightly decreased mucosal wave, mild posterior glottic gap within 2 mm during phonation; and 3=full wave, complete closure). At each follow-up visit, the patients also completed the voice handicap index (VHI) (
8), a patient-based survey divided into three subscales that measure the functional, physical, and emotional aspects of the handicap caused by voice impairment. Subscale scores can range from 0 to 40, and total scores can range from 0 to 120; a higher score indicates a greater degree of handicap.
Injection procedures
All injection laryngoplasties were performed percutaneously under local anesthesia by the same junior surgeon. Before procedure, each patient inhaled a 4% lidocaine nebulizer for 10 min. An extra nozzle was used to spray an additional 4% lidocaine onto the pharynx, larynx, and nose. The CT approach was performed through the cricothyroid membrane, directly into the vocalis muscle, using a disposable 25 G 4 cm long needle under transnasal flexible fiberscopic (Olympus laryngobronchoscope type T3) monitoring. For the TC approach, direct puncture was performed through the thyroid cartilage, just inferior to the halfway point of the cartilage (
7), 0.5-1 cm lateral to the midline Appropriate needle location was confirmed through the flexible fibersocope before injection. The tip of the needle could be seen submucosally, and was then withdrawn slightly for injections. Injection was started slowly to the vocalis muscle in front of the vocal process and continued until a slight overcorrection was achieved.
Definition of failures
We deemed the following to be injection failures:
Injection in an inaccurate location, such as a false vocal cord, subglottis, or superficial area of the vocal fold.
Insufficient vocal fold augmentation.
Leakage of injected material, due to puncture of the vocal fold mucosa.
If a booster injection was necessary within one month following the first injection.
We defined a success rate as a number that excludes the numbers of injection failures. We evaluated the overall success rate of the CT approach for primary neck patients and revisional neck patients, compared with the TC approach.
Statistical analyses
Statistical analyses were performed using the paired t-test, Wilcoxon's signed-rank test, and chi square test (SPSS ver. 12.0 SPSS Inc., Chicago, IL, USA). P-values less than 0.05 were deemed to be statistically significant.
Go to :

RESULTS
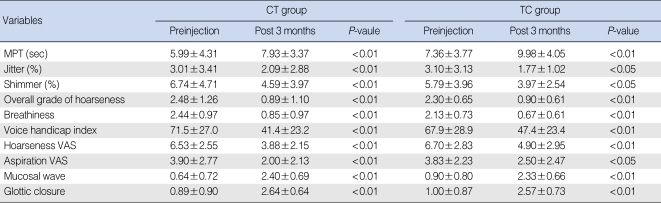
Objective parameters
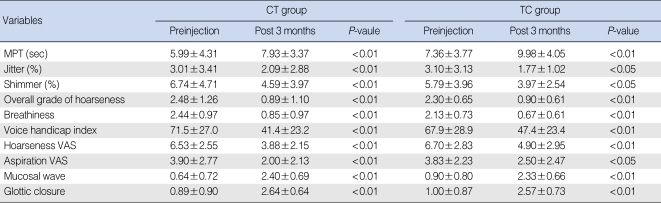
Of the patients, 124 completed the acoustic and aerodynamic analyses. Statistically significant increases were observed in maximal phonation time, and statistical decreases were observed in jitter and shimmer during the postoperative 3-month follow-up for both the CT and TC approaches. For the CT approach, the average maximal phonation time increased significantly, from 5.99±4.31 sec to 7.93±3.37 sec at 3 months (P<0.01). The average percentage of jitter and shimmer decreased from 3.01±3.41% to 2.09±2.88% and from 6.74±4.71% to 4.59±3.97% at 3 months, respectively (P<0.01). For the TC approach, the average maximal phonation time increased significantly, from 7.36±3.77 sec to 9.98±4.05 sec at 3 months (P<0.01). The average percentage of jitter and shimmer decreased from 3.10±3.13% to 1.77±1.02% and from 5.79±3.96% to 3.97±2.54% at 3 months, respectively (P<0.01).
Subjective parameters
The patients' overall ratings of their symptomatic voice, VHI, GRB AS scale, and stroboscopic analyses revealed significant improvements over their baseline evaluations for both the CT and TC approaches.
For the CT approach, the average of scores for hoarseness and aspiration on the VAS scale improved from 6.53±2.55 to 3.88±2.15 and from 3.90±2.77 to 2.00±2.13 at 3 months, respectively (
P<0.01). The patients' VHI values improved significantly, from 71.5±27.0 to 41.4±23.2 at 3 months (
P<0.01). Stroboscopic analyses also revealed that the average grade of mucosal wave and glottal closure improved significantly, from 0.64±0.72 to 2.40±0.69 and from 0.89±0.90 to 2.64±0.64 at 3 months, respectively (
P<0.01). The GRBAS scores also revealed improved overall grades of dysphonia (G) and breathiness (B) at 3 months post-operation (
P<0.01). For the TC approach, the average scores for hoarseness and aspiration on the VAS scale improved, from 6.70±2.83 to 4.90±2.95 and from 3.83±2.23 to 2.50±2.47 at 3 months, respectively (
P<0.05). The patients' VHI values improved significantly, from 67.9±28.9 to 47.4±23.4 at 3 months (
P<0.01). Stroboscopic analyses also revealed that the average grade of mucosal wave and glottal closure improved significantly from 0.90±0.80 to 2.33±0.66 and from 1.00±0.87 to 2.57±0.73 at 3 months, respectively (
P<0.01). The GR BAS scale scores also revealed improved overall grades of dysphonia (G) and breathiness (B) at 3 months postoperation (
P<0.01).
Table 2 summarized the results of objective and subjective parameters for each approach.
Table 2
Objective and subjective analysis of CT & TC approach

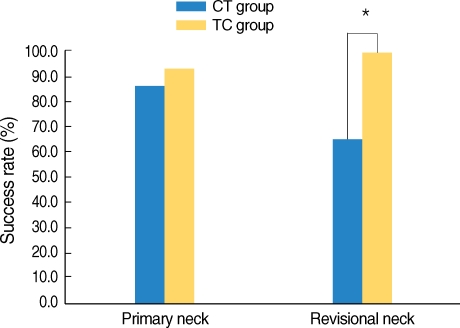
Success rates of the injection procedures
The overall success rates of the CT and TC approached were 86.2% (81 successful injections/94 injections) and 93.3% (28/30), respectively. These rates were not significantly different (
P>0.05). However, the success rate of the TC approach (100%, 13/13) was significantly higher than that of the CT approach (65%, 13/20) for previously treated neck patients (
P<0.05) (
Fig. 2).
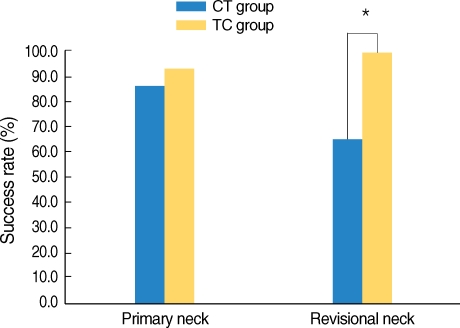 | Fig. 2
The success rate of transcartilaginous (TC) approach was significantly higher than cricothyroid (CT) approach (100% vs. 65%) for revisional neck group. Primary neck means the groups of patients who didn't received the neck operation before. Revisional neck means the groups of patients who received the neck operation before.
*significant differences between CT and TC approach group.

|
Postoperative complications
No serious adverse effect, such as airway obstruction, material migration, or granuloma formation, was observed in any patient during the follow-up period. Two patients suffered vocal fold mucosal punctures during the injection procedure. Another complication was penetration difficulty of the thyroid cartilage in the TC approach, due to ossification. We experienced two cases of penetration difficulty, one is an 82-yr-old man and the other is who had received radiotherapy to the neck. We resolved this problem by converting the injection technique from the TC to the CT approach. Another problem in the TC approach was obstruction of the needle lumen with cartilage matrix. If the appropriate location of the needle in the vocal fold cannot be determined at first, we had to change the needle for a new one.
Go to :

DISCUSSION
Injection laryngoplasty for the treatment of unilateral vocal fold paralysis has been subject to dramatic changes in recent years. Advancements in both injection techniques and biocompatible materials have advanced the field of laryngology to a new level (
9). Various approaches have been introduced to perform injection laryngoplasty under local anesthesia. Among these methods, percutaneous injection through the cricothyroid membrane is the most preferable and convenient method (
6,
10). However, it involves some technical difficulties in controlling the depth and location of the needle during the injection procedure, leading to a long learning curve. This is primarily because the direction of the CT approach is not parallel, but oblique, to the vocal fold. The average angle in the medial direction at the surface is 10-15°, and in the superior direction it is 40-50° (
6). Thus, when a patient's external anatomical landmark is indistinct, especially in patients who are obese, have short necks, or have previously undergone other neck treatments, such as thyroidectomy or neck dissection (
11), the CT approach injection procedure is more difficult. In that circumstances, the TC approach is an effective alternative to the CT approach. Berke et al. (
7) first described the CT and TC approach as one of the percutaneous injection laryngoplasty techniques to treatment of parkinsonism related dysphonia. They used the TC approach for young patients with uncalcified thyroid cartilage, and the CT approach for older patients (
12). However, there were no descriptions for both approaches, such as characteristics, advantages and disadvantages.
Our data showed that the TC and CT approaches both provided statistically significant voice improvement in subjective and objective evaluations. The overall success rate of the TC approach was comparable to the CT approach (93.3% vs. 86.2%). However, the success rate of the TC approach was significantly higher than the CT approach in patients who had previously undergone neck treatments. The volume of injected materials was significantly reduced in the TC approach versus the CT approach (0.65 mL vs. 0.84 mL). We believe this to be the result of the shorter working distance and reduced dead space in the TC approach.
The advantages of the TC approach are:
Shorter working distance, because the puncture is directly through the thyroid cartilage (11).
Injection level is vocal fold level and approach direction is parallel, not oblique, to the vocal fold level.
Easy to control the depth and location of the targeted area.
Useful for patients with problematic anatomical landmarks such as previous neck treated patients and cricothyroid space narrowed patient from congenital and postoperative cause.
Provide a alternative technique when CT approach is not possible.
The disadvantages are:
In some patients, it is not possible to use the TC approach, because ossification of the thyroid cartilage can prevent passage of the needle through the thyroid cartilage and, thus, a CT approach may be required (12).
If the appropriate location of the needle in the vocal fold cannot be determined at first, the cartilage matrix may plug the needle lumen, requiring considerable force on the syringe, or having to change the needle to expel the injection material
Based on the preliminary results of this trial, injection laryngoplasty using a TC approach was an effective alternative to the CT approach. It is especially useful technique in unilateral vocal fold paralysis patients who have previously undergone other neck operations.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download