Abstract
Objectives
This study investigated the outcomes of uvula-preserving palatopharyngoplasty (UPPPP) in patients with obstructive sleep apnea syndrome (OSAS).
Methods
Twenty men with obstructive sleep apnea syndrome received the UPPPP operation at our institution. We measured symptom changes after UPPPP using a visual analog scale (VAS), and all patients were examined with polysomnography pre- and post-operatively. 'Surgical success' was defined as reduction in apnea-hypopnea index (AHI) to below 20 events per hour and more than 50% post-operative reduction.
Results
Snoring decreased significantly (6.7±2.3 to 3.7±2.9 on VAS, P=0.002) but the postoperative globus sense did not differ from that preoperatively (2.0±2.4 to 2.1±2.7 on VAS, P=0.79). Apnea and apnea-hypopnea indices were significantly reduced after UPPPP (34.7±20 to 24.2±17.2 events/hour, P=0.029). The surgical success rate was 40% regardless of Friedman stage. There was significant reduction in the AHI on supine sleep in both surgically successful and unsuccessful patient groups.
Obstructive sleep apnea syndrome (OSAS) disturbs night sleep and causes daytime sleepiness and cardiovascular problems, such as hypertension and cerebral stroke (1). Weight reduction, change in sleeping position, use of oral appliances, and continuous positive airway pressure (CPAP) are the non-surgical treatment modalities for OSAS. Diverse surgical methods addressing OSAS-causing airway obstruction in the nasal cavity, oropharynx, and tongue base have been employed. Clinicians need to consider the clinical findings, patient compliance and preference when selecting an appropriate treatment modality. A definite set of selection criteria remain to be established (2).
Uvulopalatopharyngoplasty (UPPP), as introduced by Fujita et al. (3) in 1981, is the standard oropharynx surgical method. This operation creates smooth airflow by removing redundant oropharyngeal soft tissues and widening the anteroposterior airway. However, in 1983 Rapoport et al. (4) showed that CPAP, currently the most effective treatment modality for OSA, caused mainly lateral oropharyngeal airway expansion. This raised fundamental questions about the UPPP concept. Many patients have been dissatisfied with the treatment outcomes and frequent side effects are noted.
Globus sense - a foreign body sensation - is the most common side-effect following UPPP. It is reported in 22-31% after one year (5, 6) and up to 60% of patients after 3 years (7). Some patients complain of intractable discomfort on long-term follow-up (8). This may be related to the removal of uvula seromucous glands. Thus, surgical methods that preserve the uvula are needed (7, 9). For example, Han et al. (10) introduced 'Han's UPPP' which preserved the uvula, the tensor palati and the levator palate. These authors reported successful surgical outcomes associated with few side-effects, such as postoperative velopharyngeal insufficiency (VPI). However, to the best of our knowledge, no study has been conducted to compare globus or foreign body sense between the pre- and post-UPPP periods.
Gastaut et al. (11) were the first to report that the supine sleep position aggravated sleep apnea. This observation was followed by considerable research on the effects of sleep position on sleep apnea. Cartwright et al. (12) defined 'positional dependency' in OSAS patients and introduced positional therapy. They were strongly of the view that polysomnography (PSG), conducted in patients in various sleep positions, was essential for the diagnosis and treatment of OSAS, and that the respiratory distress index (RDI) should be evaluated for proper analysis of treatment outcomes. However, there are few reports on the impact of oropharyngeal surgery on apneal positional dependency in OSAS patients.
We devised a surgical technique to improve treatment outcomes and to minimize postoperative side effects, with uvula preservation. We also analyzed the effects of sleep position on treatment outcomes. The aim of this study was thus to determine the effect of uvula-preserving palatopharyngoplasty (UPPPP) on globus sense and positional dependency of OSAS patients.
This study was approved by the Asan Medical Center Institutional Review Board.
We reviewed the medical records of 208 patients who had been diagnosed with OSAS and had received UPPPP at the Asan Medical Center, Seoul, South Korea, from January 2003 to June 2006. For patients with severe OSA, CPAP was recommended as first line treatment. However, UPPPP was performed in patients with severe OSA who had refused CPAP treatment, or in patients with mild to moderate OSA who elected to undergo surgery. Treatment modalities including CPAP, mandibular advancement device, and surgery were explained to all patients in conjunction with the potential risks and benefits. Physical examinations, including preoperative Friedman staging and Muller gradin, were performed. For precise evaluation of treatment outcomes, we excluded patients with severe anatomic abnormalities in the nasal cavity (e.g., septal deviation, hypertrophic turbinates) and in the mandible (e.g., hypognathia, retrognathia). We analyzed post-operative symptom changes (including snoring, globus sense, and headache) using a visual analog scale (VAS) running from 0 (no symptom) to 10 (maximal symptom expression). PSG was performed using a Grass-Telefactor system, Grass-Telefactor Twin recording and analysis software (Astro-Med Inc., West Warwick, RI, USA). A type 1 (standard, in-laboratory, technician-attended, overnight) protocol was employed. Apnea index (AI, events/hour), apnea-hypopnea index (AHI, events/hour), body-mass index (BMI, kg/m2), minimal O2 saturation (SaO2min,%), and sleep position, were analyzed by PSG. An AI (AHI) is the total number of apneas (apneas and hypopneas) that occur during sleep divided by the total duration of sleep in hours. In adults, the episodes of disordered breathing must last 10 seconds or more before being considered apnea or hypopnea. The position detector was composed of small beads and was rotated by gravity change according to patient position. The detector defined a supine or non-supine sleep position. All patients received preoperative PSG and were recommended to attend for follow-up PSG about 6 months after the operation. However, most patients refused follow-up PSG for various reasons, including the expensive test fee, ineffective surgical outcome, unwillingness to visit clinic because of improvement in symptoms. Only 20 subjects received follow-up PSG.
'Surgical success' or 'responsiveness' was defined as postoperative AHI below 20 and reduction of more than 50%, compared to the preoperative value. If a positive outcome was observed, but did not meet the above criteria, the outcome was deemed 'improved'. If the postoperative AHI change was less than 5 events per hour, the outcome was deemed 'the same'. A 'worse' outcome was defined as increased AHI after surgery. 'Positional dependency' was identified when AHI decreased by more than 50% with positional change from supine to non-supine.
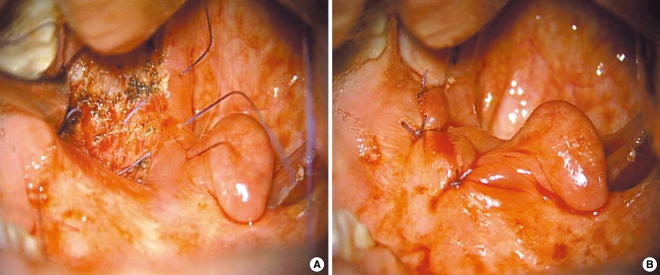
In this study, the tonsillectomy procedure was similar to that of classic UPPP. However, we preserved the uvula to minimize the incidence of postoperative globus sense and VPI. We attempted to expand the anterosuperior and lateral aspects of the airway by traction of oropharyngeal soft tissues with a suturing technique, and to prevent rupture of surgical wounds caused by dead space formation by plicating the tonsillar fossa. The preserved uvula moved upward after lateral traction of the soft palate. The surgical procedure is illustrated in Figs. 1 and 2.
Wilcoxon's signed rank test was used to compare pre- and post-operative symptom scores and PSG data. The Mann-Whitney U-test was applied to compare changes between the responsive and non-responsive groups. Statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Results are expressed as mean±SD. A P-value less than 0.05 was considered statistically significant.
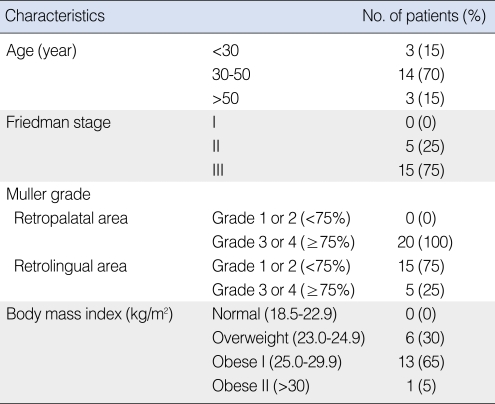
All patients were men. The mean age 40.0±9.4 years (22 to 55 years), and the mean follow-up duration was 25.8±7.0 months. Five (25%) patients were of Friedman stage II and 15 (75%) were of stage III. The preoperative Muller grades for the retropalatal area were 3 or 4 in all patients. In the retrolingual area, the number of patients of Muller grades 1 or 2 was 15 (75%), and that of grades 3 or 4 was 5 (25%). The preoperative mean BMI was 27.2±2.5 kg/m2. The patient characteristics are summarized in Table 1.
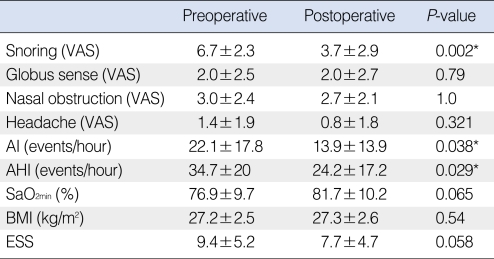
After the operation, snoring was subjectively decreased in 16 (80%) patients and remained unchanged in 4 (20%). The mean VAS score significantly decreased from 6.7±2.3 to 3.7±2.9 (P=0.002). There was no wound rupture or postoperative VPI. The mean VAS score of globus sense had not changed (preoperative VAS, 2.0±2.4 vs. postoperative VAS, 2.1±2.7; P=0.79) (Table 2).
Pre- and post-operative changes in parameters, including polysomnographic data, are summarized in Table 2. AI (from 22.1±17.8 events/hour to 13.9±13.9, P=0.038) and AHI (from 34.7±20 events/hour to 24.2±17.2, P=0.029) significantly reduced post-operatively. SaO2min increased from 76.9±9.7% to 81.7±10.2% (P=0.065) and the Epworth Sleepiness Scale (ESS) score decreased from 9.4±5.2 to 7.7±4.7 (P=0.058), with marginal statistical significance. In addition, patients with preoperative ESS scores over 10, which signify severe sleep deprivation, achieved meaningful postoperative results (mean ESS falling from 14.3±3.2 to 9.3±5.0, P=0.034). However, BMI - the most important confounding factor in the treatment analysis of OSAS patients - did not undergo post-operative change (from 27.2±2.5 kg/m2 to 27.3±2.6 kg/m2, P=0.54).
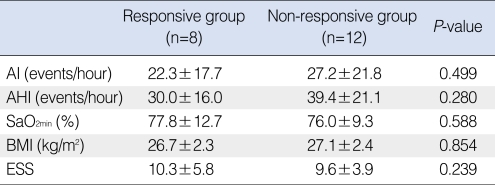
Eight (40%) patients achieved 'successful' results, 5 (25%) 'improved,' 3 (15%) remained 'the same' and 4 (20%) were 'worse.' Surgical success rates according to Friedman staging were 40% in both stage II and III groups. Patients with 'successful' results were defined as 'responsive' and others as 'non-responsive.' Preoperative AI, AHI, SaO2min, BMI, and ESS scores were analyzed between these groups but no statistically meaningful differences were seen (Table 3).
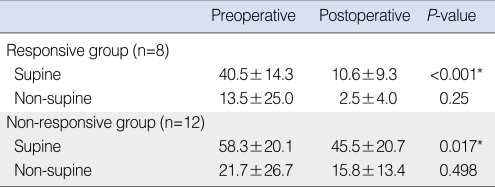
The mean preoperative AHI in the supine sleep position was 40.5±14.3 events/hour in the responsive group, and 58.3±20.1 in the non-responsive group (P=0.219). In the non-supine sleep position, the values were 13.5±25.0 and 21.7±26.7 (P=0.624), respectively. Postoperative AHI changes were significant in the supine sleep position in both the responsive (from 40.5±14.3 to 10.6±9.3, P<0.001) and the non-responsive (from 58.3±20.1 to 45.5±20.7, P=0.017) group, but statistical significance was not seen when the non-supine sleep positions were used by both groups (Table 4).
The number of patients with 'positional dependency' preoperatively was 17 of 20 (85.0%); 7 of 8 (87.5%) in the responsive group, and 10 of 12 (83.3%) in the non-responsive group. Post-operation, patients with positional dependency decreased from 7 to 5 in the responsive group, but there was no change in the non-responsive group. There was no post-operative wound rupture.
The success rate after UPPP in sleep apnea patients is about 40%, and snoring improvement rates of about 80% have been reported (13-15). However, these data have been controversial, as the success criteria were supposedly ambiguous, and statistical problems associated with the reported analyzes have been described (16). In our study, snoring subjectively decreased in 80% of patients and VAS scores fell significantly. The success rate was 40%, which thus appears comparable to that of UPPP. However, if patients with 'improved' results were included, the figure would rise to 65%. The success rates by Friedman staging were 40% in both stage II and III patients. This is noteworthy because, in a published report, patients of Friedman stage III achieved only 10% success rate if treated by UPPP alone (17).
The wound rupture rate after classic UPPP has not been reported officially, but appears to be not infrequent, according to anecdotal experience in our clinic. Because the classical suture method of UPPP includes only the anterior and posterior pillars, and not the tonsillar fossa, which facilitates dead space formation. For this reason, we sutured and plicated the tonsil bed (Figs. 1 and 2). Thus, we did not encounter postoperative wound rupture.
Finkelstein and colleagues showed that the uvula produced large quantities of thin saliva and then suddenly secreted the liquid (18). They were of the view that the uvula is a highly organized lubricating organ. The uvula consists of complex seromucous glands intermixed with a network of muscle fiber bundles, and is rich in voluminous secretory ducts, which store saliva that can be secreted after muscle contraction. The rest of the soft palate has mucous glands that produce only viscous saliva. The seromucous glands in the uvula are capable of producing much more fluid than the soft palate. Back et al. (9) claimed that the uvula played a major role in lubrication of the oral cavity and oropharynx, and that pharyngeal dryness - a sense of foreign body presence- and difficulties in phonation and swallowing, occur if the uvula is removed. Kezirian et al. (19) reported that a foreign body sensation in the pharynx was the most common complication after UPPP. In a long-term (about 20 years) follow-up study in patients who underwent UPPP, a 42.8% incidence of dry throat and foreign body sense was reported (8). In our study, however, there were no significant change in the preoperative globus sense following the operation. This is noteworthy, and presumably due to preservation of the uvula to produce thin saliva for pharyngeal lubrication.
Another potential advantage of uvula preservation is that it does not compromise CPAP compliance after surgery. A previous report showed that patients who underwent classic UPPP showed significantly lower CPAP compliance, compared to patients not treated with UPPP (20). This is because resection of the soft palate and uvula may increase air leakage through the mouth, and thus reduce the maximal tolerable CPAP pressure. Patients who received uvula-preserving modified UPPP could tolerate CPAP without mouth leakage, when compared to patients who received classic UPPP (21). Our procedure did not include resection of the soft palate or uvula, and thus may maintain patient CPAP compliance. Further evaluation on the impact of uvula-preservation on CPAP compliance is needed.
Our study showed that postoperative AHI changes were significant in the supine sleep position in both the responsive and non-responsive groups. Thus, oropharyngeal surgery in patients showing positional dependency may have a role to play, if positional therapy is unsuccessful, or if patients prefer the supine sleep position, perhaps due to musculoskeletal pain experienced in the non-supine position. The number of preoperative positionally dependent patients was 17 out of 20 (85%). As such, the number of patients without positional dependency was too small to permit comparative analysis. However, when large number of patients with positional dependency is taken into consideration, the combined efficacy of our surgical methodology and positional therapy should be expected to yield optimal results.
The limitations of this study are as follows. First, there was no control group in our study. Because of its retrospective nature, we did not compare between classic UPPP and our UPPPP method and a prospective randomized controlled trial is needed in future to valid the outcomes. Second, there was no long-term follow-up data to enable evaluation of delayed postoperative complications, and symptom changes are available. Third, the number of enrolled patients was too small to confer strong statistical reliability. This study excluded patients who had refused follow-up sleep investigations. Many patients did not want to perform follow-up polysomnography, mainly due to cost concerns. In South Korea, sleep studies are not supported by the national health insurance system. As such, the status of patients who refused to be followed-up with sleep studies remains unknown.
The value of this study rests with the fact that it is the first to compare the effects of oropharyngeal surgery on pre- and post-operative globus sense in OSAS patients.
UPPPP can minimize postoperative globus sense and other complications in OSAS patients with a success rate comparable to that of surgical methods previously reported. Furthermore, oropharyngeal surgery may reduce AHI in the supine sleep position in patients with positional dependency.
References
1. Moon HS. Influence of sleep-related breathing disorders in changes of cardiovascular function. Sleep Med Psychophysiol. 1997; 12. 4(2):129–139.
2. Lee SH, Wang SG, Koo SK, Koo HE, Yun JH, Roh HJ, et al. Long-term polysomnographic findings and subjective results in sleep apnea patients treated with laser assisted uvulopalatoplasty. Korean J Otolaryngol-Head Neck Surg. 2002; 2. 45(2):144–148.
3. Fujita S, Conway W, Zorick F, Roth T. Surgical correction of anatomic azbnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg. 1981; Nov–Dec. 89(6):923–934. PMID: 6801592.
4. Rapoport DM, Garay SM, Goldring RM. Nasal CPAP in obstructive sleep apnea: mechanisms of action. Bull Eur Physiopathol Respir. 1983; Nov–Dec. 19(6):616–620. PMID: 6360256.
5. Croft CB, Golding-Wood DG. Uses and complications of uvulopalatopharyngoplasty. J Laryngol Otol. 1990; 11. 104(11):871–875. PMID: 2266310.

6. Haavisto L, Suonpaa J. Complications of uvulopalatopharyngoplasty. Clin Otolaryngol Allied Sci. 1994; 6. 19(3):243–247. PMID: 7923849.

7. Hagert B, Wikblad K, Odkvist L, Wahren LK. Side effects after surgical treatment of snoring. ORL J Otorhinolaryngol Relat Spec. 2000; Mar–Apr. 62(2):76–80. PMID: 10729796.

8. Goh YH, Mark I, Fee WE Jr. Quality of life 17 to 20 years after uvulopalatopharyngoplasty. Laryngoscope. 2007; 3. 117(3):503–506. PMID: 17334312.

9. Back GW, Nadig S, Uppal S, Coatesworth AP. Why do we have a uvula?: literature review and a new theory. Clin Otolaryngol Allied Sci. 2004; 12. 29(6):689–693. PMID: 15533161.

10. Han D, Ye J, Lin Z, Wang J, Zhang Y. Revised uvulopalatopharyngoplasty with uvula preservation and its clinical study. ORL J Otorhinolaryngol Relat Spec. 2005; 67(4):213–219. PMID: 16103738.

11. Gastaut H, Tassinari CA, Duron B. Polygraphic study of the episodic diurnal and nocturnal (hypnic and respiratory) manifestations of the Pickwick syndrome. Brain Res. 1966; 2. 1(2):167–186. PMID: 5923125.

12. Cartwright R, Ristanovic R, Diaz F, Caldarelli D, Alder G. A comparative study of treatments for positional sleep apnea. Sleep. 1991; 12. 14(6):546–552. PMID: 1798889.

13. Fujita S, Conway WA, Zorick FJ, Sicklesteel JM, Roehrs TA, Wittig RM, et al. Evaluation of the effectiveness of uvulopalatopharyngoplasty. Laryngoscope. 1985; 1. 95(1):70–74. PMID: 3965833.

14. Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996; 2. 19(2):156–177. PMID: 8855039.

15. Janson C, Gislason T, Bengtsson H, Eriksson G, Lindberg E, Lindholm CE, et al. Long-term follow-up of patients with obstructive sleep apnea treated with uvulopalatopharyngoplasty. Arch Otolaryngol Head Neck Surg. 1997; 3. 123(3):257–262. PMID: 9076230.

16. Schechtman KB, Sher AE, Piccirillo JF. Methodological and statistical problems in sleep apnea research: the literature on uvulopalatopharyngoplasty. Sleep. 1995; 10. 18(8):659–666. PMID: 8560132.

17. Friedman M, Ibrahim H, Joseph NJ. Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope. 2004; 3. 114(3):454–459. PMID: 15091218.

18. Finkelstein Y, Meshorer A, Talmi YP, Zohar Y, Brenner J, Gal R. The riddle of the uvula. Otolaryngol Head Neck Surg. 1992; 9. 107(3):444–450. PMID: 1408233.

19. Kezirian EJ, Weaver EM, Yueh B, Deyo RA, Khuri SF, Daley J, et al. Incidence of serious complications after uvulopalatopharyngoplasty. Laryngoscope. 2004; 3. 114(3):450–453. PMID: 15091217.

20. Mortimore IL, Bradley PA, Murray JA, Douglas NJ. Uvulopalatopharyngoplasty may compromise nasal CPAP therapy in sleep apnea syndrome. Am J Respir Crit Care Med. 1996; 12. 154(6 Pt 1):1759–1762. PMID: 8970367.

21. Han F, Song W, Li J, Zhang L, Dong X, He Q. Influence of UPPP surgery on tolerance to subsequent continuous positive airway pressure in patients with OSAHS. Sleep Breath. 2006; 3. 10(1):37–42. PMID: 16432757.

Fig. 1
Illustration of uvula-preserving palatopharyngoplasty. (A, B) Axial view of the operation field. (A) The classical suture method of uvulopalatopharyngoplasty is associated with a higher rupture risk because of deadspace formation. (B) In our study, the tonsil bed is sutured together and plicated for prevention of deadspace formation. (C) Coronal view of the operation field. Soft tissues are retracted not only anteroposteriorly but also laterally by the tensile force developed in the suture technique.
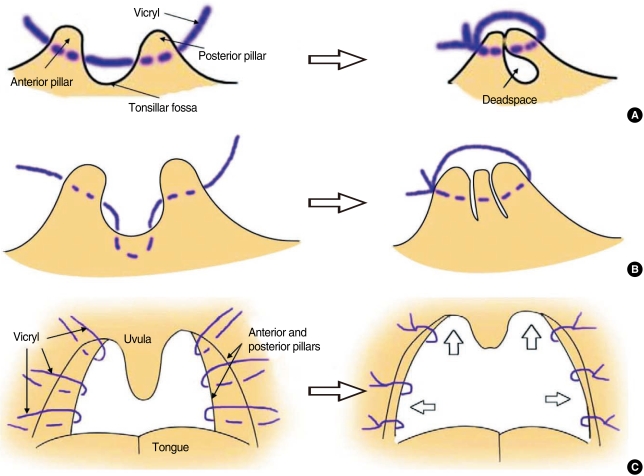
Fig. 2
Photographs of uvula-preserving palatopharyngoplasty. (A) Suturing of the anterior pillar, the tonsil fossa, and the posterior pillar with Vicryl (colored purple) is performed after tonsillectomy. The tonsil fossa is sutured for prevention of rupture caused by deadspace formation. (B) Soft tissues are retracted not only anteroposteriorly but also laterally by the tensile force developed in the suture technique. The preserved uvula will become smaller by contraction of scar tissue on both sides of the musculus palatouvularis and at the lower margin of the tensor palati.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download