Abstract
Objectives
Jugular foramen paraganglioma is a locally invasive, benign tumor, which grow slowly and causes various symptoms such as pulsatile tinnitus and low cranial nerve palsy. Complete surgical resection is regarded as the ideal management of these tumors. The goal of this study is to identify the clinical characteristics and most effective surgical approach for jugular foramen paraganglioma.
Methods
Retrospective analysis of 9 jugular foramen paraganglioma patients who underwent surgical resection between 1986 and 2005 was performed. Clinical records were reviewed for analysis of initial clinical symptoms and signs, audiological examinations, neurological deficits, radiological features, surgical approaches, extent of resection, treatment outcomes and complications.
Results
Most common initial symptom was hoarseness, followed by pulsatile tinnitus. Seven out of 9 patients had at least one low cranial nerve palsy. Seven patients were classified as Fisch Type C tumor and remaining 2 as Fisch Type D tumor on radiologic examination. Total of 11 operations took place in 9 patients. Total resection was achieved in 6 cases, when partial resection was done in 3 cases. Two patients with partial resection received gamma knife radiosurgery (GKS), when remaining 1 case received both GKS and two times of revision operation. No mortality was encountered and there were few postoperative complications.
Conclusion
Neurologic examination of low cranial nerve palsy is crucial since most patients had at least one low cranial nerve palsy. All tumors were detected in advanced stage due to slow growing nature and lack of symptom. Angiography with embolization is crucial for successful tumor removal without massive bleeding. Infratemporal fossa approach can be considered as a safe, satisfactory approach for removal of jugular foramen paragangliomas. In tumors with intracranial extension, combined approach is recommended in that it provides better surgical view and can maintain the compliance of the patients.
Jugular foramen paragangliomas are rare, slow-growing, encapsulated, hypervascular tumors that arise from jugular foramen of temporal bone (1). Jugular foramen paraganglioma are known to occur predominantly in the age of 50 to 60, and female to male ratio is reported to be 5:1 (1, 2). Incidence of multiple lesion is reported to be between 25 to 50% in familial cases, compared with less than 10% in sporadic cases (1).
Jugular foramen paragangliomas are locally invasive, expanding within the temporal bone via pathways of least resistance, such as air cells, vascular lumens, skull base foramina, and eustachian tube (3, 4). Significant intracranial and extracranial extension may occur, as well as extension within the sigmoid sinus and inferior petrosal sinuses (3-5).
Clinical course of jugular foramen paragangliomas reflects their slow growth and paucity of symptoms, which often results in a significant delay in diagnosis (1, 3, 6). The most common presenting symptom is known to be pulsatile tinnitus, followed by hearing loss (2, 7).
Complete surgical resection is the ideal management of most jugular foramen paragangliomas (2, 5, 7-9). Radiation therapy can be utilized as an alternative treatment modality for certain candidates including elderly and medically inoperable patients, and is also indicated in recurred tumor after surgical resection and in residual tumors when gross total removal of extensive tumor could not be carried out (10). Control of jugular foramen paraganglioma ranged from 85 to 100% (10). Gamma knife surgery is recently introduced and can be used as a primary tool in cases without significant cervical extension or in patients with recurrent tumors in intracranial area (10).
To identify the clinical characteristics and most effective surgical approach, the authors have made a retrospective analysis of the patterns of clinical presentation, surgical approaches and treatment outcomes in 9 patients with jugular foramen paraganglioma who underwent surgical treatment.
This study included 9 patients with jugular foramen paraganglioma confirmed by permanent pathologic reports. The patient group consisted of 4 men and 5 women who underwent surgery by a single surgeon between 1986 and 2005. Mean age at the time of diagnosis was 40.8 yr, ranging from 26 to 60 yr. Follow up period was 29 month to 264 months, with mean follow up period of 93 months. Five cases occurred on the right side and remaining 4 cases on the left, and there was one case where bilateral lesion was detected.
Review of clinical records was performed, analyzing initial clinical symptoms and signs, audiological examinations and neurological deficits, radiological features, surgical approaches, extent of resection, treatment outcomes and postoperative complications.
The extent of jugular foramen paraganglioma was classified according to Fisch classification, based on radiological findings. The extent of removal was determined according to intraoperative findings and postoperative imaging study.
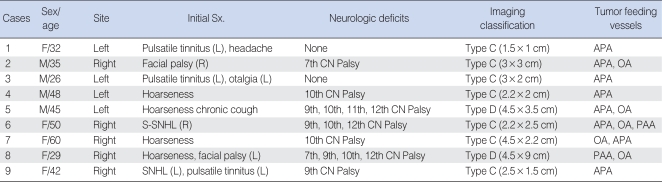
Most common initial symptom at the time of first outpatient visit was hoarseness which was observed in 4 patients, followed by pulsatile tinnitus which was noted in 3 cases (Table 1). Sudden sensorineuronal hearing loss in 2 patients, facial palsy in 2 patients and neck mass in 1 patient were also reported. All patients except for 2 cases had at least one low cranial nerve palsy on evaluation. Most common neurologic deficit on presentation was 10th nerve palsy, followed by 9th nerve, 12th nerve, and 7th nerve in order.
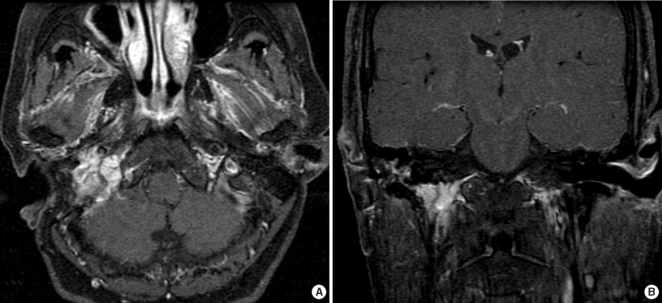
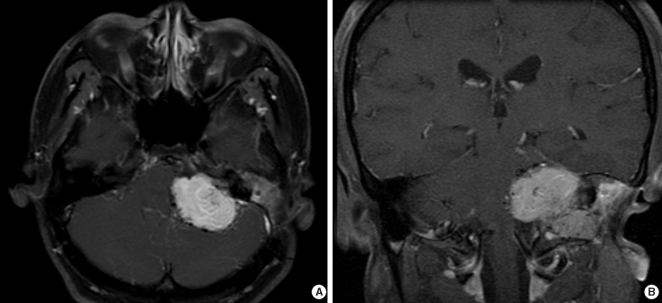
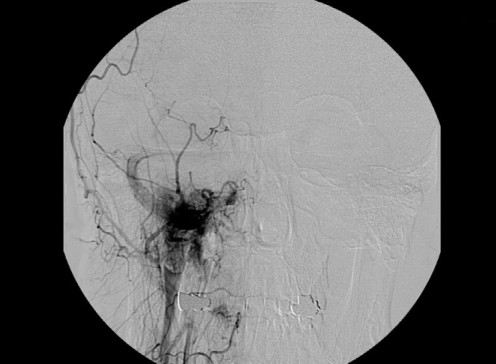
Magnetic resonance imaging (MRI) and angiography were performed in all cases. The extent of jugular foramen paragangliomas were classified according to Fisch classification with radiologic findings of MRI. Seven patients were classified as Type C (Fig. 1) and remainnig 2 patients were Type D (Fig. 2). Size of the tumor varied from as small as 1.5×1 cm to as large as 4.5×9 cm. On angiography, all tumors had at least one main feeding vessel. Ascending pharyngeal artery was the most common feeding vessel, and successful embolization of the feeding vessel was achieved in all cases (Fig. 3).
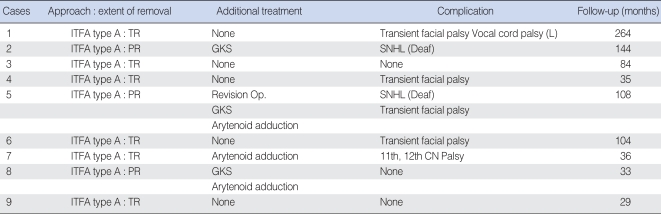
Nine patients underwent a total of 11 operations (Table 2). Type A infratemporal approach alone was used in all cases. Complete resection was achieved in 6 patients, and all of them is under regular outpatient follow-up without any sign of recurrence. All type D tumors resulted in partial resection and 1 out of 7 Type C tumors was partially resected. The residual tumor in the 2 cases of Type D jugular foramen gangliomas was the portion of intracranial extension. In one type D tumor case (case 5), 1 cm sized residual tumor was suspected in postoperative MRI after first operation in 1999. The patient received gamma knife radiosurgery (GKS) on the remnant tumor and was continuously observed with MRI at the outpatient. However, the patient had to undergo revision operation in cooperation with neurosurgery department in 2006 because the tumor mass grew as large as 4 cm. Tumor still remained after the second operation and revision operation by neurosurgery department was performed in 2007, still resulting in small portion of residual tumor. The remaining tumor is under observation currently. In the remaining two partial resection cases, staged operation was planned initially. However, the patients refused to undergo the burden of major surgery twice after the first operation (infratemporal approach), and gamma knife surgery had to be performed as an alternative to planned staged operation by neurosurgery department. Tumor was completely shrunken in one case, and tumor was stabilized without growing in the other case.
No mortality was encountered during the follow-up period, ranging from 17 to 275 months (mean, 71 months). Most common postoperative complication was transient facial palsy which occurred in 4 cases. In all 4 cases, patient showed H-B Grade IV palsy which returned to H-B Grade II palsy in a few months. Since Infratemporal fossa approach inevitably encounters facial palsy due to transposition of facial nerve, facial palsy of grade better than H-B Grade II was excluded from the criteria of complications. In 2 cases, audiologic function was lost postoperatively. In one patient, 11th and 12th nerve palsy were newly developed post-operatively. Three patients received arytenoid adduction, 2 cases due to unilateral vocal cord palsy, and one case due to decreased vocal cord mobility. In other case, left vocal cord palsy developed, but the patient did not undergo arytenoid adduction since symptom due to vocal cord palsy was not prominent.
Our collected data showed some differences from the previous reports on jugular foramen paraganglioma. In previous reports, jugular foramen paraganglioma is known to occur predominantly in the age of 50 to 60, and female to male ratio is reported to be 5:1 (1, 2). However, the female to male ratio was 5:4, and tumors were detected at the mean age of 40.8 yr in our data, even though the age of detection was distributed widely, not being focused to certain age group. Our data showed no significant preference to certain sex, age and site, in terms of incidence.
Most common initial presenting symptom at the time of first visit to the outpatient was hoarseness, whereas the most common presenting symptom is known to be pulsatile tinnitus, followed by hearing loss in the previous reports (2, 7). Lower cranial nerve dysfunction is relatively common with glomus jugulare tumors and includes dysphagia, hoarseness, aspiration, tongue paralysis, shoulder drop, and voice weakness (3, 5, 7). Our result was consistent with that, and 7 out of 9 patients showed at least one low cranial nerve palsy, emphasizing the importance of neurologic evaluation of low cranial palsy at the time of first visit. Emphasis should also be given on the fact that patients without pulsatile tinnitus should not be excluded from the suspicion of jugular foramen paraganglioma. Facial nerve paralysis is known to occur less commonly, but it signals advanced disease and is related with poor facial nerve prognosis outcome (3, 5, 7). Our data was consistent with the reports. Facial palsy was present in 2 cases in our data and both cases were advanced jugular foramen paragangliomas. Facial nerve function was not restored from the initial facial nerve palsy after the operation in both cases.
On imaging evaluation with MRI, 7 patients were Type C tumors and remaining 2 cases were Type D tumors. It correlates with the fact that jugular foramen paragangliomas are slow growing and lack symptoms which results in the late diagnosis of the tumor (1, 3, 6). Successful embolization and surgical removal of tumor without massive bleeding were achieved in all cases. Ascending pharyngeal artery was the most common feeding vessel, as reported previously (11). Since the tumor is hypervascular in nature, angiography is crucial to identify main feeding vessels and embolize them prior to surgery which decreases the chance of massive bleeding intraoperatively (11).
Complete surgical resection is the ideal management of most jugular foramen paragangliomas (2, 5, 7-9). In our cases, all of the cases were approached with Type A infratemporal fossa approach alone. 6 out of 7 Type C tumors were resected completely and are under observation without any sign of recurrence. All Type D tumors resulted in partial resection and 1 out of 7 Type C tumors was partially resected. GKS after partial resection of the tumor was reported to be effective (10), but recurrence was observed in 1 out of 3 cases in our data. We recommend that combined approach in cooperation with the neurosurgery department should be implemented in the first place in cases of jugular foramen ganglioma with intracranial extension, rather than planning a staged operation. Jackson et al. showed that a single-stage resection and reconstruction offered the greatest likelihood of complete tumor removal while preserving local tissue for use in reconstruction (12). Combined approach can include infratemporal fossa, suboccipital, middle fossa, anterior craniofacial, translabrynthine approach, and more. These approaches can be combined depending on the location of the tumor (12, 13). Combined approach can expose the tumor better than single approach since better operative view of the tumor can be obtained from two different angles, which should result in better chance of complete removal of the tumor (13). The widened view also prevents excessive effort to remove unvisualized portion of the tumor, which might cause injuries to the nerves. There is a problem to seal a larger defect in combined approach compared with a single approach, but advances in reconstruction technique of the defect has decreased concerns to this problem (12, 13). Combined approach is also much better to maintain compliance of the patient for the treatment. In our cases, all patients in whom staged operation was planned refused to undergo the secondary operation due to decreased compliance after the first operation.
In our cases, infratemporal approach was sufficient in complete resection of the tumor in most cases when intracranial extension was not present, with the aid of embolization. No mortality was encountered and permanent postoperative complications occurred in few cases, as observed in the results. With skilled surgical technique, infratemporal fossa approach can be considered as a safe and effective approach for removal of jugular foramen paraganglioma without intracranial extension.
Glomus jugulare tumors can be presented in various manners. In our result, low cranial involvement was present in most of the cases, suggesting that neurologic examination of the low cranial nerve is crucial.
In the surgical aspect, it can be concluded that infratemporal fossa approach provides safe, satisfactory way to remove jugular foramen paraganglioma, but combined approaches is strongly recommended instead of staged operation when treating jugular foramen paraganglioma with intracranial extension.
References
1. Heth J. The basic science of glomus jugulare tumors. Neurosurg Focus. 2004; 8. 15. 17(2):E2. PMID: 15329017.

2. Ramina R, Maniglia JJ, Fernandes YB, Paschoal JR, Pfeilsticker LN, Neto MC, et al. Jugular foramen tumors: diagnosis and treatment. Neurosurg Focus. 2004; 8. 15. 17(2):E5. PMID: 15329020.

3. Al-Mefty O, Teixeira A. Complex tumors of the glomus jugulare: criteria, treatment, and outcome. J Neurosurg. 2002; 12. 97(6):1356–1366. PMID: 12507134.

4. Prabhu SS, DeMonte F. Complete resection of a complex glomus jugulare tumor with extensive venous involvement: case report. Neurosurg Focus. 2004; 8. 15. 17(2):E12. PMID: 15329027.
5. Patel SJ, Sekhar LN, Cass SP, Hirsch BE. Combined approaches for resection of extensive glomus jugulare tumors. A review of 12 cases. J Neurosurg. 1994; 6. 80(6):1026–1038. PMID: 8189258.
6. Coles MC. Glomus jugulare tumor presentation and management: a case study. J Neurosci Nurs. 2004; 8. 36(4):221–223. PMID: 15366548.

7. Watkins LD, Mendoza N, Cheesman AD, Symon L. Glomus jugulare tumours: a review of 61 cases. Acta Neurochir (Wien). 1994; 130(1-4):66–70. PMID: 7725944.

8. Michael LM 2nd, Robertson JH. Glomus jugulare tumors: historical overview of the management of this disease. Neurosurg Focus. 2004; 8. 15. 17(2):E1. PMID: 15329016.

9. Woods CI, Strasnick B, Jackson CG. Surgery for glomus tumors: the Otology Group experience. Laryngoscope. 1993; 11. 103(11 pt 2 suppl 60):65–70. PMID: 8231595.
10. Mascarenhas F, Ferreira AG, Carvalho H, Almeida A, Santos M, Cattoni MB, et al. Kondziolka D, McDermott M, Régis J, Smee R, Flickinger JC, editors. Stereostatic radiosurgery in the management of glomus jugulare tumors. Radiosurgery. 2006. Basel: Karger;p. 108–117.
11. Valavanis A. Preoperative embolization of the head and neck: indications, patient selection, goals, and precautions. AJNR Am J Neuroradiol. 1986; Sep–Oct. 7(5):943–952. PMID: 3096120.
12. Jackson CG, Netterville JL, Glasscock ME 3rd, Hampf CR, Carrasco VN, Haynes DS, et al. Defect reconstruction and cerebrospinal fluid management in neurotologic skull base tumors with intracranial extension. Laryngoscope. 1992; 11. 102(11):1205–1214. PMID: 1405979.

13. Jackson CG, Kaylie DM, Coppit G, Gardner EK. Glomus jugulare tumors with intracranial extension. Neurosurg Focus. 2004; 8. 15. 17(2):E7. PMID: 15329022.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download