Abstract
Objectives
Although it is well recognized that a small meatus after canal wall down (CWD) tympanomastoidectomy can cause a lifetime problem, unsatisfactory results are frequently encountered. We herein introduce a novel technique, perichondrial posterior fixation (PPF), to maintain a wide external auditory canal (EAC), to minimize postoperative wound infection due to the smaller dead space and to improve the posterior auricular cosmetic outcome.
Methods
A total of 73 patients who underwent CWD tympanomastoidectomy were included. Interventions are CWD tympanomastoidectomy with the PPF technique. Review of the medical records and evaluation of the postoperative size of the meatus and the extent of the cavum conchal cartilage buried within the mastoid cavity by taking digital photographs.
Results
Thirty males and 43 females were included and the mean age was 44.1 yr (range, 6 to 66 yr). The mean follow-up duration was 26 months (range, 12 to 56 months). All ears maintained a clean and large external meatus. The posterior auricular cavum conchal cartilage was successfully prevented from being buried into the mastoid cavity in all ears. The extent of cartilage buried into the mastoid cavity was much reduced compared to the conventional technique.
Meatoplasty is routinely performed as an integral part of a canal wall down (CWD) mastoidectomy. It is typically performed at the end of the mastoidectomy to assist in ventilation and to provide easy access for cleaning of the cavity postoperatively.
Numerous methods for modified meatoplasty have been introduced and used since the first description by Stacke (1). However, conventional meatoplasty in CWD mastoidectomy results in sliding of the cavum conchal portion from the posterior wall (Fig. 1). Therefore, the opening of the external auditory canal (EAC) becomes slightly stenotic and auricular deformity may occur. Deformities of the EAC are especially more severe in children than in adults due to the thinner, more elastic and less rigid nature of their cartilage.
Hence, we introduced a novel technique, perichondrial posterior fixation (PPF), to maintain a wide EAC, to minimize postoperative wound infection due to the smaller dead space, and to improve the posterior auricular cosmetic outcome.
Medical records of 88 patients diagnosed with chronic otitis media with/without cholesteatoma and who underwent CWD tympanomastoidectomy with the PPF technique from January 2003 to December 2006 were reviewed. Fifteen cases followed up for less than 12 months were excluded. The postoperative size of the meatus and the extent of the cavum conchal cartilage buried within the mastoid cavity were evaluated on a regular basis. This technique was approved by institutional review board (IRB No: 0905-030-281).
Meatoplasty was performed as the final surgical procedure of CWD tympanomastoidectomy just before the closure of the subcutaneous tissue and skin.
To expose the conchal cartilage, soft tissue over the cartilage was elevated just above the perichondrial layer posterolaterally (Fig. 2). The excessive conchal cartilage was excised as in conventional meatoplasty. Then 2 stitches were used to pull the perichondrium of the cavum conchal cartilage posteriorly to the remnant periostium of the mastoid bone with absorbable 3-0 vicryl thereafter (Fig. 3). After the subcutaneous suture was completed, the meatus was packed with nylon strips and antibiotics-soaked cotton wicks.
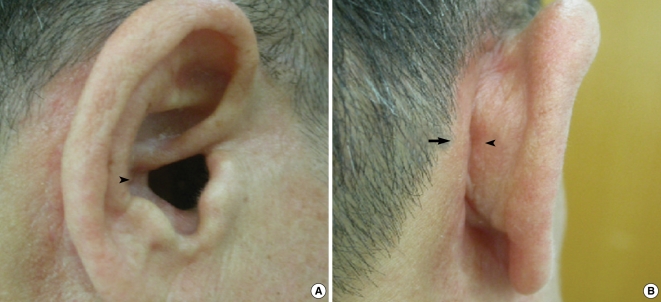
Sixty-five adults and 8 children underwent meatoplasty using the PPF technique. Thirty patients were male and 43 were female. The mean age of the patients at surgery was 44±14.1 yr old (range, 6 to 66 yr). The mean follow-up duration was 26±13.2 months (range, 12 to 56 months). All ears maintained a clean and large external meatus. Using our novel PPF technique, we could successfully prevent the posterior auricular cavum conchal cartilage from being buried in the mastoid cavity in all ears that were operated on. The extent of the cartilage buried within the mastoid cavity was significantly reduced, resulting in an improved outcome compared to the conventional technique (Fig. 4). Five of 73 patients (6.8%) had postoperative infection of the retroauricular area, and of those five, infections of four were easily controlled by topical antibiotics. Only one patient suffered from severe infection, and was admitted and treated with intravenous antibiotics.
Meatoplasty is one of the key procedures in modified radical mastoidectomy. A large external auditory meatus allows ventilation of the mastoid cavity as well as easy access for examination and debridement of the entire cavity. Removal of the soft tissue and cartilage of the EAC and concha could enlarge the meatus, but the meatoplasty procedures can be complicated by stenosis, infection, and auricular deformity. Stenosis of the meatus has the potential to cause a number of problems including accumulation of cerumen, chronic otitis externa, hearing impairment, and difficulty in examining the ear (2). Numerous surgical techniques to prevent and correct meatal stenosis of the ear canal have been described (3-6). Techniques of meatoplasty have included a combination of transposed skin flaps, removal of the conchal cartilage, removal of the cartilage from the tragus or floor of the ear canal, and use of conchomastoid sutures or meatal packing to maintain a large meatal diameter (7-9). The disadvantages of these techniques are that they are either excessively complicated or they fail to meet the need of removing both the excess cartilage and bone to achieve a proper meatus. Also, in patients who underwent conventional meatoplasty, stenoses of the external ear canal opening were observed as the cavum conchal cartilage gradually collapsed into the posterior wall. This also resulted in adverse cosmetic outcomes. Eventually, stenosis of the meatus causes ventilation dysfunction, resulting in a wet cavity and thereby accumulation of cerumen. In particular, pediatric patients' conchal cartilages are less elastic, and thinner than those of adult patients. Hence pediatric patients' conchal cartilages are easily pulled and displaced by the tension of the facial muscle. Consequently, the cartilaginous portion of the EAC in pediatric patients tends to be more stenotic and tortuous than that of adult patients after conventional meatoplasty.
An ideal meatoplasty for preventing stenosis of the EAC after CWD should be simple to perform, reliable, and cosmetically acceptable. Since 2003, we have designed and adopted a new method in which the perichondrium of the cavum conchal cartilage is anchored posteriorly to the periostium of the mastoid bone. There was no stenosis seen in our series and cosmetically successful outcomes were achieved in all cases. This technique allowed direct fixation of the cartilage to the posterior wall and resulted in a decrease in postoperative infection by reducing the dead space in the operation field. Perichondritis secondary to cartilage excision, although theoretically possible, has not been observed in our cases. A previous study reported a 12 to 20% rate of revision meatoplasty in a series of patients who had undergone CWD mastoidectomy (10). In contrast, none of the patients required revision meatoplasty after performing our novel technique. In addition, the rate of postoperative infection was not significantly different from the rate for conventional meatoplasty (1.9 to 6.5%) found in a previous report (11). Furthermore, in cases in which revision canaloplasty or CWD were required for stenosis of the EAC, or in cases of recurrent infection after conventional meatoplasty, correction of the stenosis and a good cosmetic outcome were obtained by applying our PPF technique. However, cosmetic outcomes could not be improved when the cartilage or soft tissue had been removed excessively during previous procedures.
The PPF technique, which is a novel method of meatoplasty in CWD tympanomastoidectomy, can be an effective treatment modality in maintaining a large EAC and in improving the cosmetic outcome with minimal risk of complications.
References
1. Roulleau P. Development of the surgery of chronic otitis. Rev Laryngol Otol Rhinol (Bord). 1993; 114(2):87–91. PMID: 8284561.
2. Fisch U, Chang P, Linder T. Meatoplasty for lateral stenosis of the external auditory canal. Laryngoscope. 2002; 7. 112(7 Pt 1):1310–1314. PMID: 12169919.

3. Paparella MM, Kurkjian JM. Surgical treatment for chronic stenosing external otitis (Including finding of unusual canal tumor). Laryngoscope. 1966; 2. 76(2):232–245. PMID: 5324121.
4. Soliman T, Fatt-Hi A, Abdel Kadir M. A simplified technique for the management of acquired stenosis of the external auditory canal. J Laryngol Otol. 1980; 5. 94(5):549–552. PMID: 7400681.

5. Hunsaker DH. Conchomeatoplasty for chronic otitis externa. Arch Otolaryngol Head Neck Surg. 1988; 4. 114(4):395–398. PMID: 3348895.

6. Mirck PG. The M-meatoplasty of the external auditory canal. Laryngoscope. 1996; 3. 106(3 Pt 1):367–369. PMID: 8614206.

7. Eisenman DJ, Parisier SC. Meatoplasty: the cartilage of the floor of the ear canal. Laryngoscope. 1999; 5. 109(5):840–842. PMID: 10334243.

8. Suskind DL, Bigelow CD, Knox GW. Y modification of the Fisch meatoplasty. Otolaryngol Head Neck Surg. 1999; 7. 121(1):126–127. PMID: 10388893.

9. Raut W, Rutka JA. The Toronto meatoplasty: enhancing one's results in canal wall down procedures. Laryngoscope. 2002; 11. 112(11):2093–2095. PMID: 12439187.

10. Garap JP, Dubey SP. Canal-down mastoidectomy: experience in 81 cases. Otol Neurotol. 2001; 7. 22(4):451–456. PMID: 11449098.

11. Kos MI, Castrillon R, Montandon P, Guyot JP. Anatomic and functional long-term results of canal wall-down mastoidectomy. Ann Otol Rhinol Laryngol. 2004; 11. 113(11):872–876. PMID: 15562896.

Fig. 1
A surgical outcome by conventional meatoplasty. (A) Lateral view. Narrowing of the external auditory canal due to sliding of the conchal cartilage (arrowhead) from the posterior wall. (B) Posterior view. The cavum conchal cartilage (arrowhead) is buried in the mastoid cavity (arrow).
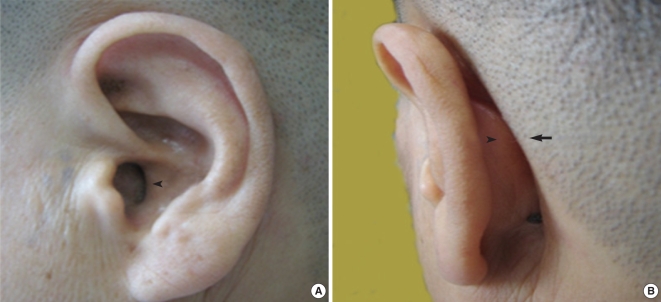
Fig. 2
The surgical technique of a novel meatoplasty in canal wall down tympanomastoidectomy using perichondrial posterior fixation. (A) Partial excision of the cavum cochal cartilage. (B) A wedge incision is made in the Ko_rner flap. (C) Suturing the anterior edge (arrowhead) of the conchal cartilage to the periosteum of the mastoid bone (arrow) with 3-0 vicryl. (D) Final result after finishing our novel meatoplasty.
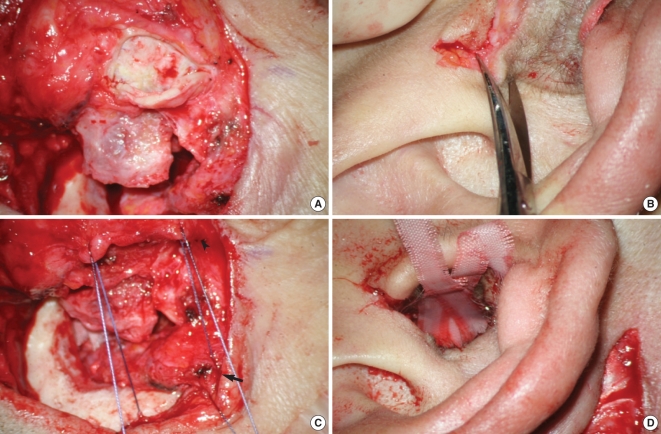
Fig. 3
Axial cross-section diagram at the level of the external auditory canal (EAC) of the right ear. (A) Narrowed EAC opening (a) by conventional meatoplasty and reduced height of the external auricle by boring into the mastoid cavity (B) Cutting the excessive anterior edge (b) of the conchal cartilage. (C) Suturing the anterior margin of the conchal cartilage posteriorly to the periosteum of the mastoid bone (c), widened EAC opening (d) by prevention of conchal cartilage sliding.

Fig. 4
A surgical outcome by perichondrial posterior fixation. (A) Lateral view. Widening of the external auditory canal (arrowhead) by fixation of the conchal cartilage to the posterior wall. (B) Posterior view. Elevation of the cavum conchal cartilage (arrowhead) on the posterior mastoid wall (arrow).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download