INTRODUCTION
Radiotherapy has been shown to be effective in controlling carcinoma of the larynx, and the combination of radiotherapy and an organ-sparing protocol has been used frequently to treat patients with advanced-staged laryngeal carcinoma. Nevertheless, irradiation of laryngeal tissue may cause hypoxic, hypovascular, and hypocellular changes that impair normal collagen synthesis and cell production, leading to tissue breakdown and the formation of chronic non-healing wounds (
1). The main complications of radiation therapy for laryngeal carcinoma are laryngeal edema, skin damage, perichondritis, and cartilage necrosis (
2). Patients with these complications have various clinical manifestations, including skin erythema, pain, dysphagia, hoarseness, dyspnea, and weight loss. In addition, some patients experience laryngeal edema, ulceration, and cartilage exposure (
3).
Chondroradionecrosis (CRN) of the larynx is one of the most serious complications of radiation therapy. It may progress or become fatal despite aggressive treatment measures. Hyperbaric oxygen therapy (HBO) has been used to treat radiation necrosis of the head and neck (
4-
7). HBO is thought to repair vascular beds within the irradiated tissue, enhancing neovascularization and wound healing. The efficacy of HBO in the treatment of laryngeal CRN has been described in only a few case reports and series (
6-
8). The purpose of this study was to determine the optimal diagnostic methodology and management in six patients with laryngeal CRN.
MATERIALS AND METHODS
Patients who presented with CRN of the larynx between 2002 and 2007 at a tertiary care hospital were enrolled in this retrospective study. Patients were diagnosed on the basis of endoscopy, computed tomography (CT), positron emission tomography (PET), and pathologic examination. All patients were treated with radiotherapy combined with surgery or chemotherapy for squamous cell carcinoma arising in the larynx, and were followed regularly thereafter. Following suspicion of CRN, all patients underwent CT, PET, or combined PET/CT, and biopsy. All necrotic tissues were removed with microforceps under suspension laryngoscopy and sent for culture and pathologic examination to exclude recurrent cancer. Patients with recurrent tumors were excluded from this study. The degree of CRN was categorized according to the previously described grading system for laryngeal radiation changes (
3).
Each patient was treated with parenteral broad-spectrum antibiotics, humidity, and oral washing. HBO consisted of 2 hr of 2.5 atm 100% oxygen, once or twice daily, for 6 days each week. If symptoms and signs became aggravated despite aggressive therapy and were associated with other serious impending complications, the patient underwent total laryngectomy. We reviewed the diagnosis, treatment, and clinical course and outcome of each patient.
RESULTS
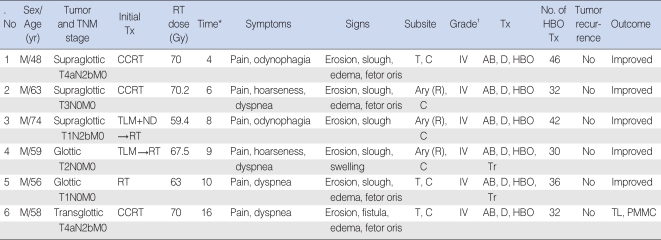
Six patients (all men; mean age, 60 yr) were included in this study; their clinical and treatment profiles are summarized in
Table 1. All patients previously had laryngeal cancer and were treated with external beam radiotherapy (n=4) or intensity-modulated radiotherapy (n=2), with a mean total radiation dose to the larynx of 66.7±4.5 Gy. Three patients underwent concurrent chemoradiotherapy. Two patients initially underwent transoral laser microresection of laryngeal cancer and postoperative radiotherapy for microscopic positive resection margins or extensive nodal stage. The mean time between completion of radiotherapy and CRN diagnosis was 8.8±4.1 months (range, 4 to 16 months). All patients complained of pain in the anterior neck or odynophagia, and four patients had progressive dyspnea. All patients had a history of smoking (mean of 40±8 pack-years; range, 29 to 50 pack-years), and two patients were smokers at the time of CRN diagnosis. Two patients had chronic obstructive pulmonary disease, two had diabetes mellitus, and two had hypertension. One patient underwent a laryngoscopic biopsy 1.5 months before diagnosis of CRN. All patients had Chandler grade IV CRN.
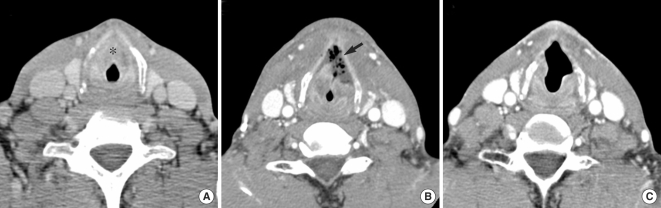
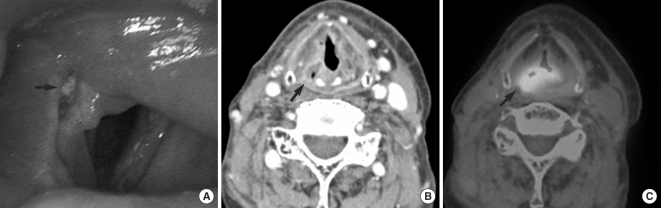
CT revealed air bubbles, cartilage erosion or fragmentation, fistula formation, or absence of the unilateral arytenoid cartilage (
Figs. 1,
2). All patients underwent PET or combined PET/CT prior to suspension laryngoscopy and HBO. PET showed that one patient had local tumor recurrence (false positive), and five patients were free of tumors (true negatives). On suspension laryngoscopy, all patients showed laryngeal mucosal erosion, as well as fragmentation or sloughing of the exposed laryngeal cartilage: three in the anterior larynx (
Fig. 1) and three in the posterior larynx (unilateral arytenoid and cricoid cartilages) (
Fig. 2). All patients underwent removal of necrotic tissue with microforceps. Pathologic examination of the tissue samples confirmed there was no tumor recurrence.
All six patients were treated with antibiotics and HBO. Bacterial culture showed positive results in four patients, with infection by Streptococcus viridans, Enterobacter cloacae, Pseudomonas aeruginosa, or Acinetobacter baumannii. Antibiotic therapy was dependent on the results of culture sensitivity tests. HBO consisted of a mean of 36±6 dives (range, 32 to 46 dives). Although respiratory distress improved in most patients after the start of HBO, two patients received temporary tracheostomies to resolve upper airway obstruction. Despite aggressive treatment, one patient had aggravation of laryngeal CRN and infection of the deep cervical space from a fistula. This patient underwent a total laryngectomy and received coverage with transposition of a pectoralis major myocutaneous flap. The other five patients showed improvement of CRN on follow-up CT and endoscopy. Pathologic examination of biopsy and laryngectomy specimens showed no evidence of tumor recurrence in any of these patients. Local recurrence of tumors or CRN was not observed during a mean follow-up period of 24 months (range, 12 to 62 months). One patient, however, died of regional recurrence and distant metastasis.
DISCUSSION
Laryngeal CRN is a very rare but serious complication of radiotherapy for laryngeal carcinoma, with an expected incidence of less than 1% (
8). Organ-preserving protocols have become more popular in the treatment of patients with advanced laryngeal carcinomas. Combination radiotherapy and chemotherapy is increasingly utilized; this may increase the incidence of complications following radiotherapy. For example, of 341 patients with laryngeal or hypopharyngeal carcinomas treated with radiotherapy alone or with chemoradiotherapy, 4 (1.2%) had CRN, and 8 (2.3%) had both CRN and tumor recurrence (
9). The incidence of CRN is directly related to the total dose, field size, and duration of therapy. The incidence increases at total doses of 70 Gy or more (
3). For example, of 18 patients with laryngeal CRN, 8 (44%) had been treated with total radiotherapy doses of 70 Gy or more (
7). Although the clinical presentation of CRN usually occurs within one year after radiotherapy, it has been observed more than 10 yr after radiotherapy (
10,
11). Our study agrees with these findings. In addition, our study is the first to report two patients with CRN after they underwent the organ-preserving strategy of laser microsurgery plus radiotherapy. This suggests that laryngeal subsites previously injured by laser surgery may be more vulnerable to irradiation injury, resulting in cartilage exposure and necrosis.
Symptoms and signs of laryngeal complications from irradiation vary from slight hoarseness, dryness, and edema to severe pain, respiratory distress, fetor oris, and fistula formation (
3). Chandler grade (
3) I or II laryngeal CRN is expected to occur in patients after they have undergone irradiation; such cases generally do not require treatment. Chandler grade III and IV patients have serious complications and may progress despite aggressive treatment measures. The symptoms and signs are similar to those seen in recurrent laryngeal carcinoma, presenting a major diagnostic dilemma for clinicians (
9,
12,
13). The CT appearance of laryngeal CRN is nonspecific and indistinguishable from that of tumor recurrence. CRN, however, may be identifiable on CT through sloughing of the arytenoid cartilage, fragmentation and collapse of the thyroid cartilage, and/or the presence of gas bubbles around the cartilage (
14). Although PET may distinguish benign and malignant changes in the irradiated larynx (
15), repeated laryngoscopy and biopsy are essential to help resolve this diagnostic problem. Even then, the answer may not be clear because submucosal tumor recurrence may be detected on whole organ sections despite multiple biopsies (
9,
12). To differentiate CRN from tumor recurrence, a diagnostic algorithm may be used, in which PET is initially performed in patients with grade III or IV laryngeal complications, with biopsy subsequently performed in PET-positive patients (
13). The follow-up PET may also help to differentiate tumor recurrence and CRN occurrence by showing no change or a decrease in the standardized uptake values of the focal uptakes (
15). In the present study, one of the six patients had false-positive PET results, and none had local recurrence on pathologic examination or during follow-up. Therefore, patients presenting with CRN after radiotherapy should be under high suspicion for tumor recurrence.
Conservative measures have been recommended to treat patients with Chandler grade I or II CRN, including humidification, steroids, and antibiotics for up to six weeks, Patients with grade III or IV CRN are more difficult to treat, both medically and surgically (
8). The efficacy of HBO for laryngeal CRN was evaluated retrospectively in 18 patients; 13 (72%) showed functional and symptomatic improvement, 4 failed to respond to treatment, and 1 developed recurrence (
7). The combination of HBO and surgery led to improvement in 20 of 26 patients (77%) with mandibular osteoradionecrosis (
5). In contrast, a recent randomized controlled study showed that HBO did not benefit 68 patients with overt mandibular osteoradionecrosis (
16). Although the rarity of CRN has precluded the use of randomized controlled studies of HBO in the treatment of this condition, our findings and the findings of others suggest that HBO may be effective in treating CRN (
6,
7). In addition, HBO may eliminate the need for surgery and may enable patients who have had tracheostomies to be decannulated (
17). The present findings also suggest that the early removal of necrotic tissue under suspension laryngoscopy may be helpful in the treatment of CRN, in combination with HBO. Radical surgery, such as total laryngectomy, may sometimes be required to treat patients with progressive CRN, nonfunctional larynges, and a high suspicion of tumor recurrence.
CRN of the larynx is a rare but fatal complication of radiotherapy that may be detected early by endoscopic and imaging methods. Nevertheless, pathologic confirmation may be necessary to exclude the possibility of tumor recurrence. Early removal of necrotic tissue and HBO may help improve CRN and thereby save the functional larynx.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download