This article has been
cited by other articles in ScienceCentral.
Abstract
Concha bullosa is a common anatomic variation of the middle turbinate; however, sinusitis secondary to the concha bullosa is rare. A 52-yr-old woman presented with nasal obstruction and posterior nasal drip. Computed tomography and examination of the nasal cavity revealed septal deviation on the left side, and a massive concha bullosa and maxillary sinusitis on the right side. The lateral lamella of the affected turbinate was removed and the inspissated material was drained. Histopathologic examination of the excised lesion in the concha bullosa revealed bacterial colonies in the mucus plug. We report here on a massive concha bullosa with secondary maxillary sinusitis.
Go to :

Keywords: Massive concha bullosa, Sinusitis
INTRODUCTION
Concha bullosa is a cystic distension of the middle nasal concha. This variation of the middle turbinate is very common and various studies have reporting the frequency of this as 14-53%. However, polyps, mucocele formation, and infection in the concha bullosa are rare. There have been few reported cases since Bektas et al. (
1) first noted an instance of an infected concha bullosa with orbital extention. There have been no reports about a massive concha bullosa with definite secondary maxillary sinusitis in the current literature. Here we describe a patient who has nasal obstruction and symptoms of post nasal drip due to a massive concha bullosa and the related sinusitis.
Go to :

CASE REPORT
A 52-yr-old woman was admitted to our clinic with complaints of nasal obstruction and posterior nasal drip. She had suffered with these symptoms for several months. On nasal examination, we noted the hypertrophic right middle turbinate and left septal deviation. The patient was allergic to aspirin and penicillin, and she was a hepatitis B-viral carrier. She was otherwise healthy and the routine laboratory results were all normal.
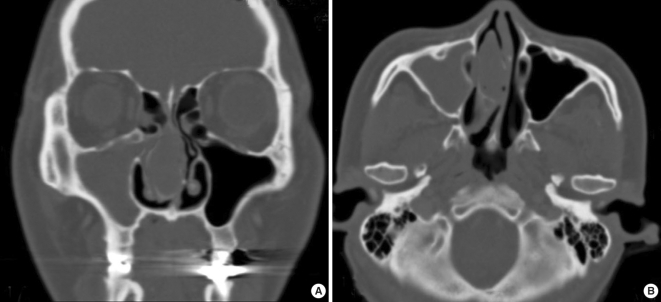
Computed tomography (CT) of the paranasal sinuses showed a massive concha bullosa that bulged into the lateral nasal wall, with almost total obstruction of the maxillary sinus ostium (
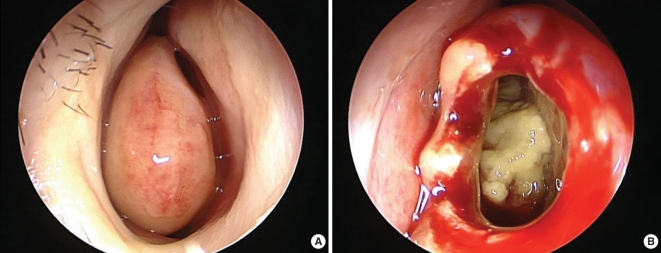
Fig. 1). In addition, right maxillary sinusitis was also observed. On the endoscopic examination, the concha bullosa was pale and it could be mistaken as the inferior turbinate because it protruded anterior to an inferior turbinate (
Fig. 2A). On the operation, the lateral and medial lamellae of the concha bullosa were separated and the lateral lamella was then cut out. There was some yellowish, inspissated material, and a polypoid lesion in the concha bullosa (
Fig. 2B). The yellowish, concentrated material was aspirated out and the polypoid lesion was sent to the Pathology Department for further examination. Next, a middle meatal antrostomy was performed and a discharge of pus was observed through the antrostomy site. A bacterial culture was performed with negative results. Histopathological examination of the excised lesion from the concha bullosa revealed bacterial colonies in the mucus plug and lymphocytic infiltration, which were both consistent with chronic inflammation. The patient's symptoms quickly diminished postoperatively. The endoscopic examination that was done two weeks after the operation showed a clear cavity.
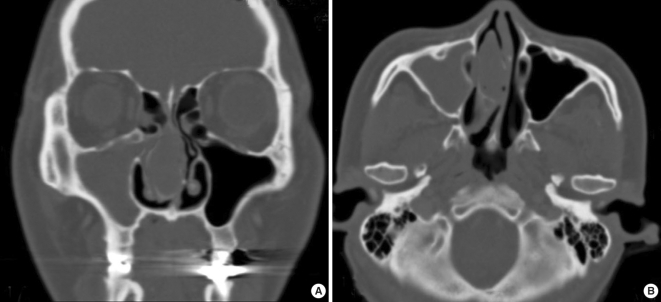 | Fig. 1Coronal & Axial CT of the paranasal sinus shows the right huge concha bullosa and maxillary sinusitis. 
|
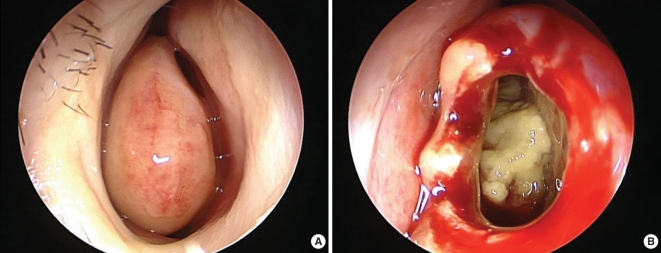 | Fig. 2Preoperative finding: telescopic view (0°, 4 mm) of the right nasal cavity shows the huge concha bullosa of the middle turbinate. Intraoperative finding: after resection of lateral lamella of the concha bullosa, telescopic view (0°, 4 mm) shows that it is filled with yellowish, inspissated material. 
|
Go to :

DISCUSSION
A concha bullosa is an aerated middle turbinate. Pneumatization of the middle turbinate may originate from the frontal recess, the anterior ethmoids or directly from the middle meatus. In one reported case, ventilation of the air cells within a concha bullosa came from the area from which the pneumatization arose (
2).
A concha bullosa can be infected, and cases of massive concha bullosa pyocele have been reported. The patient in our report complained of no acute symptoms, but acute orbital symptoms can be a sign of orbital extension (
1).
There is conflicting data on whether or not concha bullosa is a cause of sinusitis. Several studies have shown there is no relationship between concha bullosa and sinusitis (
3,
4). However, in this case, there was a massive concha bullosa obstructing the middle meatus, and this caused the right maxillary sinusitis.
Of interest is the relationship between the concha bullosa and septal deviation. A study reported that septal deviation does not result in concha bullosa, but it does augment the pneumatization of the middle turbinate depending on the degree of the angle of deviation (
5). Consistent with this previous report, we think that in this case, the septal deviation on the left side encouraged the development of a right concha bullosa.
In conclusion, we suggest that if a patient has an infected concha bullosa with secondary maxillary sinusitis, resection of the lateral wall of the concha bullosa and endoscopic sinus surgery will be needed to properly treat this condition.
Go to :





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download