Pneumothorax is a rare complication associated with pulmonary alveolar proteinosis (PAP) [
123]. Pneumothorax can be detected during diagnosis of PAP [
1] or can manifest as a complication after whole-lung lavage (WLL) [
2]. There have been several case reports regarding anesthetic management of WLL in patients with PAP [
456]. However, there are few reports about WLL in patients whose PAP is complicated with pneumothorax [
3]. We treated a case of WLL complicated with pneumothorax, which we suspect occurred after a previous lavage. We successfully managed the patient's complications with chest-tube insertion. We describe the case, herein, with a review of the relevant literature.
Case Report
A 30-year-old male who was 161 cm tall and weighed 91 kg (morbid obesity, body mass index 35.0 kg/m
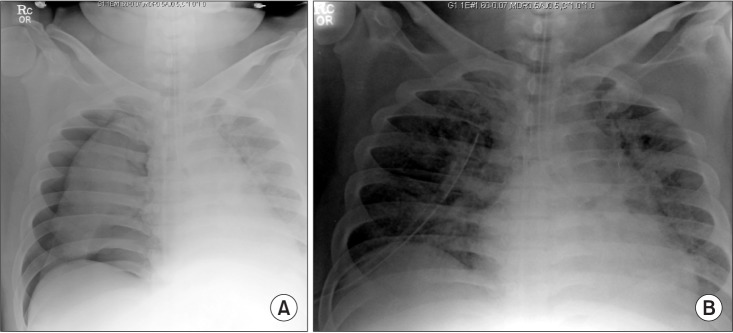
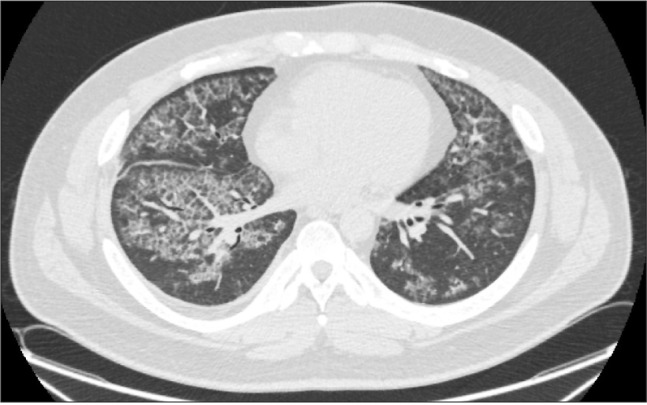
2) underwent WLL as treatment for PAP (
Fig. 1). The patient had been suffering dyspnea on exertion for three years. His vital signs were blood pressure (BP) 130–150/70–80 mmHg, heart rate (HR) 80–100 beats/min, respiratory rate (RR) 18–22 rates/min, and body temperature 36.2℃. The patient's oxygen saturation by pulse oximeter (SpO
2) while receiving air was 75–89%, which was partially corrected to 91–98% while receiving 2 L/min of oxygen via nasal prong (VNP). Arterial blood gas analysis (ABGA) under oxygen administration revealed the following: pH 7.39, arterial CO
2 partial pressure (PaCO
2) 44.6 mmHg, arterial O
2 partial pressure(PaO
2) 65.3 mmHg, and bicarbonate (HCO
3–) 26.1 mEq/L.
 | Fig. 1Chest computed tomography-performed 9 days before admission. CT images demonstrate characteristics of ground-glass opacities with a crazy-paving appearance in both lungs, suggesting pulmonary alveolar proteinosis.
|
During induction, both mask ventilation and intubation were difficult (laryngeal view: Cormack-Lehane grade IV). Intubation trials with a 37-Fr. left-sided double lumen tube (DLT) (Mallinckrodt™, Covidien, Dublin, Ireland) and laryngoscopy, followed by a videostylet (Optiscope®, Pacific Medical, Seoul, Korea) failed. Hence, a flexible fiberoptic bronchoscope (FOB) was used to intubate a single lumen tube (SLT) (ID 8.0), and then the SLT was changed to a DLT using a tube exchanger.
Left one-lung ventilation (OLV) was maintained with an SpO
2 of 86–90% at an inspired oxygen fraction (FIO
2) of 1.0 during right-lung lavage. We performed external percussion physiotherapy with an automatic mechanical percussion device (The Vest™ Model 205 [Airway Clearance System], frequency 10 Hz, duration 3 minutes, Hill-Rom, Charleston, SC, USA) rather than manual chest percussion. After right-lung lavage, we resumed two-lung ventilation (TLV) with intermittent suction for 20 minutes (FIO
2 1.0). For left-lung lavage, right OLV was started with an FIO
2 of 1.0, but it was impossible to maintain SpO
2 > 80% (
Table 1). Therefore, we decided to postpone left-lung lavage until conditions in the right lung improved (
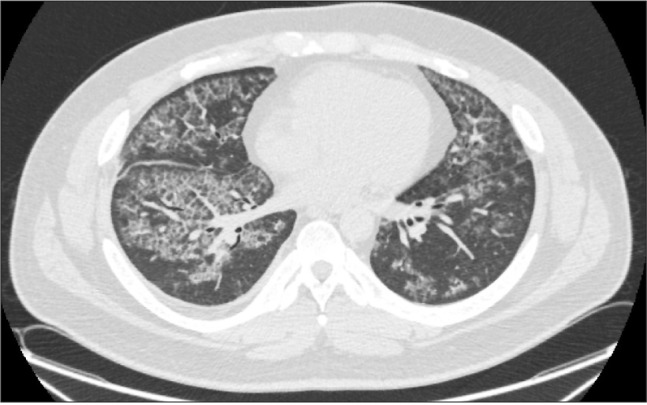
Fig. 2). A chest X-ray taken after intensive care unit (ICU) transfer showed no specific findings, including pneumothorax. One day after the lavage, while in the ICU, the patient was weaned from mechanical ventilation, extubated, and transferred to the general ward.
 | Fig. 2Chest X-ray taken one day before the second lavage. There are no specific findings except for increased diffuse parenchymal opacity in both lungs.
|
Table 1
Arterial Blood Gas Analysis
|
|
pH |
PaCO2 (mmHg) |
PaO2 (mmHg) |
HCO3–(mEq/L) |
FIO2
|
|
1st day |
TLV |
7.4 |
38.2 |
0100.1 |
22.9 |
1.0 |
|
Left OLV |
7.36 |
40.3 |
61.6 |
22.1 |
1.0 |
|
TLV |
7.4 |
34.5 |
82.3 |
20.8 |
1.0 |
|
Right OLV |
7.36 |
44.4 |
49.6 |
24.4 |
1.0 |
|
2nd day |
TLV |
7.38 |
43.0 |
56.9 |
24.6 |
1.0 |
|
TLV (C-tube) |
7.36 |
41.2 |
93.2 |
22.9 |
1.0 |
|
Right OLV |
7.34 |
44.6 |
60.3 |
23.4 |
1.0 |

Three days later, the patient was returned to the operating room for left-lung lavage. The patient's SpO2 was 91–96% with O2 3 L/min VNP. We intubated the trachea with a SLT via Glide-Scope (Verathon Medical, British Columbia, Canada) and then changed the SLT to a DLT with a tube exchanger because the previous intubation was difficult. We confirmed breath sounds from both lungs, and right and left lung ventilation during separation through auscultation. The proper tube location was confirmed using an FOB.
TLV was performed in volume-controlled mode: FIO
2 1.0, tidal volume of 400 ml, RR of 15 rates/min, peak inspiratory pressure (PIP) of 31 cmH
2O, and positive end-expiratory pressure (PEEP) of 5 cmH
2O. PaO
2 was 57 mmHg (SpO
2 86%) on ABGA examination. Fifty minutes after induction, we started right OLV in pressure-controlled mode: FIO
2 1.0, inspiratory pressure of 25 cmH
2O above PEEP 5 cmH
2O, tidal volume of 200 ml, and RR of 20 /min. Within a few minutes of starting right OLV, the patient's SpO
2 plunged below 80%, so we rapidly resumed TLV and re-confirmed the proper position of the DLT using an FOB. We did not observe any bronchial secretion or obstruction. Right OLV was tried again, but the patient's SpO
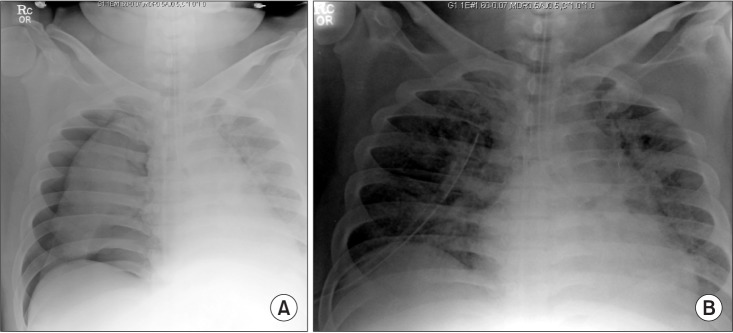
2 rapidly decreased to < 80% within a few minutes. After resuming TLV, 2.5 mg of salbutamol was nebulized to relieve any bronchial constriction, and 100 mg of hydrocortisone was injected intravenously to improve symptoms. During manual ventilation, we detected very poor lung compliance. In auscultation, the patient's breath sounds from the right lung were very distant and nearly inaudible. Therefore, we suspected he had a right-side pneumothorax, which was confirmed on chest X-ray (
Fig. 3A). A chest tube was inserted by a thoracic surgeon, and a follow-up chest X-ray showed that the pneumothorax had decreased (
Fig. 3B). Two hours after induction, lung compliance and arterial oxygenation improved: FIO
2 1.0, tidal volume of 450 ml, RR of 18/min, PIP of 24 cmH
2O, and PEEP of 5 cmH
2O. PaO
2 improved to 93 mmHg on the following ABGA examination (
Table 1).
 | Fig. 3(A) Chest X-ray taken during the second lavage procedure shows a newly developed right-side pneumothorax. (B) Chest X-ray taken after chest-tube insertion shows that the right-side pneumothorax had decreased.
|
We re-tried right OLV and were finally able to maintain SpO2 > 90%: FIO2 1.0, inspiratory pressure of 23 cmH2O above PEEP 5 cmH2O, tidal volume of 320 ml, and RR of 20 /min, without any severe air leakage or tidal-volume loss. The left-lung lavage was started along with right OLV with the chest tube inserted state. During the remaining lavage period, we maintained SpO2 > 85% without further deterioration.
After lavage, the patient was transferred to the ICU and received mechanical ventilation. On postoperative day (POD) 1, the patient developed a high fever (38.8℃) and was diagnosed as having pneumonia with parapneumonic effusion in the right lower lobe, so antibiotics were administered. The chest tube was removed on POD 3, and extubation was performed on POD 4. The patient was transferred to the general ward on POD 7 and discharged on POD 19. Follow-up chest computed tomography was performed 40 days after the left-lung lavage; it showed interval decreases in the extent of PAP in both lungs, resolved parenchymal consolidation in the right lung, and decreased right pleural effusion (
Fig. 4).
 | Fig. 4Follow-up chest computed tomography taken 40 days after the bilateral whole lung lavage. The findings included interval decreases in the extent of pulmonary alveolar proteinosis in both lungs, a resolved state of parenchymal consolidation in the right lung, and decreased right pleural effusion.
|
Go to :

Discussion
The few published reports of PAP cases described complications with spontaneous or post-procedural pneumothorax [
123]. In Stoica et al. [
1]'s report, a spontaneous pneumothorax was detected while diagnosing PAP and was not successfully controlled with chest tube insertion. After two months of unsuccessful pleural drainage, the patient received a thoracotomy for a surgical suture of the lung apical blebs. One month after the surgical repair, he underwent sequential lavages of both lungs. Spontaneous pneumothorax is a rare complication of PAP and represents an absolute contraindication for WLL until resolved. Full lung expansion is mandatory for WLL, but chest drainage is often unsuccessful because of the precarious condition of the pulmonary tissue. In Yang et al. [
2]'s case, a post-procedural pneumothorax occurred during multiple bronchoalveolar lavages in a patient with acute progressive PAP. The pneumothorax was thought to be a complication of the third WLL and mechanical ventilation, and was absorbed prior to the fourth WLL. Another case report related a pneumothorax that developed during placement of a balloon catheter using a wire guide in a child who needed a WLL. In this case, airway perforation for catheter positioning via the Seldinger technique caused the pneumothorax, not the lavage procedure itself [
3]. The physician detected the pneumothorax because of severe respiratory instability requiring high ventilation pressure. The post-procedural pneumothorax was immediately drained, and WLL was resumed, as in our case.
In our case, we assumed that positive pressure ventilation during anesthesia induction and OLV while attempting the second WLL could have led to pneumothorax through rupture of the friable alveolar structure of the right lavaged lung and aggravated it. The pneumothorax was detected after decreased lung compliance and loss of breath sound, and was managed via chest-tube insertion, which enabled subsequent WLL resumption. Because there was no sign of a pneumothorax on the chest X-ray taken after the right lavage, the hypoxemia that had occurred previously during the right OLV for the left lung lavage on the first procedure day might have been caused by poor lung condition, and not by the pneumothorax, which is what happened on the subsequent lavage procedure day.
The golden standard for PAP therapy is WLL [
45]. This procedure is contraindicated in patients with a co-existing respiratory disease, such as respiratory infections or pneumothorax [
1]. If we had detected the right-side pneumothorax prior to performing the second lavage, we would have inserted a chest tube in advance or considered delaying the left lavage. However, we did not detect any signs of a pneumothorax on the daily chest X-rays, which were performed until the day prior to the second lavage procedure (
Fig. 2). Moreover, decreased lung compliance and hypoxemia are features that commonly accompany OLV. Therefore, there was a delay in our ability to suspect a possible right-side pneumothorax in the event of hypoxemia during right OLV. When a patient with PAP has refractory hypoxemia prior to lavage, extracorporeal membrane oxygenation should be considered to avoid severe hypoxemia with fatal consequences during lavage [
6]. Firat et al. [
7] reported combined lavage techniques to manage PAP. Multiple segmental lavages (MSL or prewash) were recommended for hypoxemic patients prior to WLL to improve oxygenation. These two techniques (MSL and WLL) can be used consecutively in PAP patients who are initially unable to undergo general anesthesia.
Campo et al. [
8] performed a global survey to obtain information about current practices and the procedures of WLL. They found that WLLs were generally performed under general anesthesia with a DLT in two consecutive sessions at 1–2 week intervals. They also found that use of warm saline, drainage of lavage fluid by gravity, and indications for WLL therapy for PAP were homogenous across the study centers. There was also high variation in the choice of which lung to be lavaged first, position choice, contraindications, follow-up methods and timing, use of chest percussion, extubation timing, lung isolation and lavage methods for small children, and the amount of fluid used for WLL. We selected the first lung to be lavaged based on imaging, preference for supine position, automatic mechanical chest percussion, staged extubation after mechanical ventilation, and the amount of total fluid ranging between 10–18 L. In our review of previous WLL reports, the most frequent complication was transient fever (18%), and the complication rate for pneumothorax was 0.8% [
8]. Although WLL is an invasive procedure, it has been determined to be safe and is associated with a low procedure-related morbidity rate.
In conclusion, we experienced an unexpected pneumothorax, which might have been caused by a previous attempt at WLL and was managed by pleural drainage; we were subsequently able to successfully perform a second WLL. Therefore, if sudden high airway resistance is encountered during ventilation in a patient with previous WLL history, it is necessary to assume the possibility of pneumothorax for the patient's safety.
Go to :






 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download