Abstract
Serotonin syndrome is an unexpected fatal adverse event related to serotonergic medication. This case report is the first report describing the possible treatment effect of famotidine on serotonin syndrome. Furthermore, this is the first case report of serotonin syndrome induced by meperidine alone in a patient with no previous history suggesting a susceptibility to serotonin syndrome. A 70-year-old male with no recent history of serotonergic drug use presented with severe serotonin syndrome following ureteroscopy, possibly due to postoperative meperidine administration. The patient's symptoms included hypertension, tachycardia, tachypnea, hyperthermia, myoclonus, diaphoresis, retching, nausea, agitation, and semicoma mentality with no pupillary light reflex. Symptoms began to subside immediately after the administration of intravenous famotidine for prevention of aspiration pneumonia, with mental and neurological symptoms showing improvement initially, followed by autonomic symptoms. This case report suggests that the histamine type 2 receptor antagonist famotidine may be an effective emergency treatment for serotonin syndrome.
Go to : 
Meperidine-induced serotonin syndrome is a very rare adverse event that may occur during anesthesia that is often missed or treated inadequately. Untreated serotonin syndrome can be fatal. The mortality rate of severe serotonin syndrome ranges from 2% to 12% [1]. The syndrome usually occurs in the context of usage of antidepressants or other medications that increase serotonin prior to surgery. However, a previous report described the occurrence of meperidine-induced serotonin syndrome in a patient with a past history of clomipramine-induced serotonin syndrome [2]. The present report is the first case of meperidine-induced serotonin syndrome in a patient with no use of other serotonergic medication and also with no history of susceptibility. Furthermore, an unexpected paradoxical rapid reversal of the neurologic symptoms of serotonin syndrome was observed in this case in association with the administration of famotidine.
A 70-year-old male was admitted for the ureteroscopic removal of ureter stones. He had been receiving treatment with glimepiride for diabetes; atorvastatin for hyperlipidemia; and aspirin, thiazide, valsartan, and carvedilol for hypertension and atrial fibrillation for several years prior to admission. The patient had undergone two previous surgeries, knee arthroplasty and cataract operation, with no report of significant perioperative events. He had not taken serotonergic medications for at least 4 weeks prior to admission. Atrial fibrillation was well controlled before surgery. His physical status classification was American Society of Anesthesiologists class II.
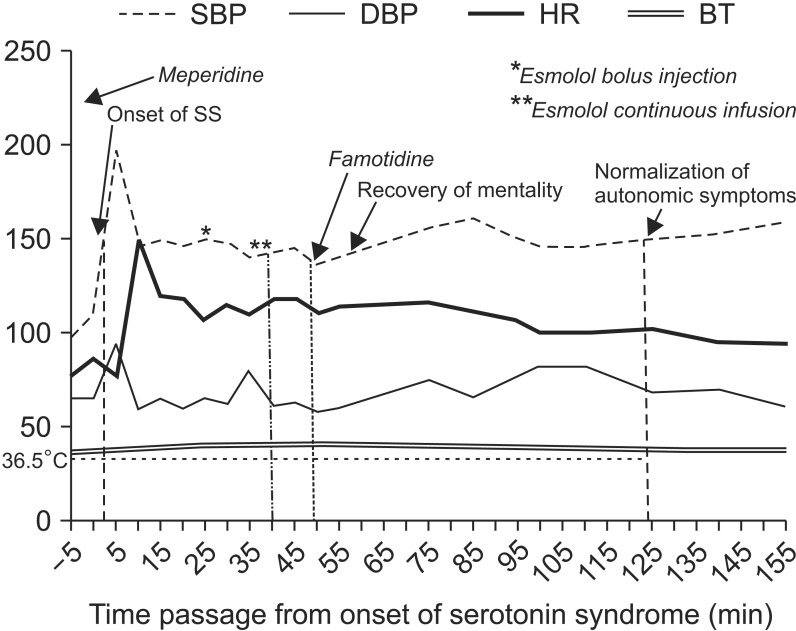
Spinal anesthesia was achieved with the administration of hyperbaric bupivacaine (12.5 mg). Surgery required 40 min and was uneventful. Stable vital signs and alert mentality were maintained in the postanesthesia care unit for more than 30 min. Intravenous meperidine (25 mg) was injected to relieve shivering. Fig. 1 illustrates changes in vital signs with time following meperidine treatment. Five minutes after the injection of meperidine, the patient complained of the sudden onset of chest discomfort and difficulty breathing. Diaphoresis, agitation, and tachypnea (28 breaths/min) were observed at the same time. Severe rigidity and tremors along with myoclonus began within 10 min, but were limited to the upper extremities because of the prior administration of spinal anesthesia. The patient soon became drowsy, confused, and uncooperative with staff. Blood pressure (BP) was elevated from 98/65 mmHg at postoperative baseline to 199/95 mmHg, and pulse rate increased from 77 beats/min to 150 beats/min. Invasive BP monitoring was initiated at the radial artery. Body temperature measured 25 min after meperidine injection was 39.8℃. Mental status deteriorated to stupor. Arterial blood gas analysis showed a pH of 7.436, PaCO2 of 27.2 mmHg, PaO2 of 114.6 mmHg, SaO2 of 98.4%, Na+ of 137 mEq/L, K+ of 4.46 mEq/L, and Ca2+ of 3.64 mg/dl. Esmolol (15 mg) was injected to lower the heart rate (HR), and ipratropium bromide inhalation was initiated for bronchodilation. Despite supportive care, hypertension and tachycardia continued and body temperature increased further to 40.1℃. Esmolol infusion was initiated at 0.5 mg/kg/min. Despite this treatment, mental deterioration progressed to semicoma. Pupils were dilated (8 mm) and unresponsive to light. At 50 min after meperidine injection, we decided to perform emergency brain computed tomography (CT).
Immediately prior to transfer for CT, the patient was administered intravenous injections of metoclopramide (10 mg) and famotidine (20 mg) for retching and vomiting. During transfer for CT and within 15 min of famotidine administration, his mental state demonstrated marked improvement. He was able to recognize people and even appeared awake to the nursing staff. The results of the brain CT were unremarkable. Following the CT examination, the patient was transferred to the intensive care unit. Immediately after arrival, his mental and neurological status were assessed, and he was found to be alert, with no neurological abnormalities (myoclonus, tremor, agitation, or mydriasis). Vital signs slowly improved over the next hour with continued supportive care. Only systolic BP and HR remained elevated at 2 h after the onset of serotonin syndrome (Fig. 1).
Go to : 
This case met Sternbach's diagnostic criteria for serotonin toxicity [3], and the medical history, laboratory data, neurological examination, and neuroimaging excluded other possible diagnoses. Meperidine was the most likely causative agent in this case because of the close temporal relationship between meperidine injection and the onset of serotonin syndrome. No other potentially causative medication was administered before the onset of the syndrome. It is very rare that meperidine alone induces serotonin syndrome. This is the first case report of serotonin syndrome induced by meperidine alone in a patient with no history to suggest a susceptibility to serotonin syndrome.
Although serotonin syndrome is a potentially life-threatening situation, specific treatment for serotonin syndrome has not yet been established. Serotonin syndrome is caused by hyperactivity of central and/or peripheral serotonin receptors [4]; therefore, several previous treatment attempts have aimed to suppress serotonergic transmission using chlorpromazine [5], cyproheptadine [6], risperidone [7], propranolol [8], or even electroconvulsive therapy [9]. However, the efficacy of these treatments has not been proven, and none are routinely recommended because of side effects and the availability of the above-mentioned pharmaceutical agents only in the oral form.
The present report describes a case of serotonin syndrome exhibiting immediate paradoxical reversal of unconsciousness and neurological symptoms following the intravenous administration of famotidine. Famotidine is a histamine receptor antagonist with high selectivity for histamine 2 (H2) receptors. It has been reported to be associated with several unexpected central nervous system (CNS) effects such as delirium, mania, and seizures [10]. Delirium associated with famotidine has been reported in several cases, possibly associated with central anticholinergic effects [11].
The mechanisms underlying famotidine-mediated reversal of serotonin syndrome are a matter of speculation. Perhaps this H2-selective blocker increases the histamine concentration at CNS synapses, resulting in hyperactivation of histamine H1 receptors and mental arousal. Another possible explanation is that histamine H2 antagonists may have an effect on reduction of blood serotonin levels [12].
Famotidine, a drug that has been the subject of attention at times, has been reported to result in a paradoxical treatment response via an unknown mechanism in the CNS. The present case did not confirm whether the pharmacological effects of famotidine alone caused a dramatic recovery of neurologic symptoms or whether the interaction of famotidine and the patient's individual genetic specificity resulted in an improvement of the symptoms. However, it is useful to note that this is the first report that famotidine may be an effective treatment for serotonin syndrome. It is also worthwhile to note that the intravenous formulation of famotidine enables rapid medication administration in non-cooperative patients. In addition, famotidine is known to be a relatively safe drug with few drug interactions. Further preclinical and clinical studies are necessary to confirm the efficacy and safety of this treatment.
This case had two idiosyncratic features. First, the patient's mental and neurological state improved immediately following famotidine administration. The half-life of meperidine is 2.5–4 h. The patient's neurological symptoms recovered beginning approximately 60 min after the administration of meperidine. In addition, the recovery from moderate to severe serotonin syndrome takes 24 h to several days. Therefore, the course in this case is not thought to represent the natural course of recovery.
Although the mechanisms are uncertain, the close temporal relationship between the administration of the medication and the recovery of the neurological symptoms strongly suggests that famotidine contributed to symptom reversal in this case. While metoclopramide was also administered, it is unlikely to have contributed to recovery because metoclopramide has been reported to actually cause or exacerbate serotonin syndrome [1314]. Second, the recovery of individual symptoms followed a distinct time course, with mental condition showing immediate improvement, followed by mitigation of neurological symptoms and the more gradual remission of autonomic symptoms. In contrast, recovery from serotonin syndrome is generally gradual, spanning a period of over several hours.
In summary, anesthesiologists should keep in mind that meperidine alone can induce serotonin syndrome and the administration of famotidine, a relatively safe drug with few drug interactions, may be useful in critical patients with suspected serotonin syndrome.
Go to : 
References
1. Frank C. Recognition and treatment of serotonin syndrome. Can Fam Physician. 2008; 54:988–992. PMID: 18625822.
2. Guo SL, Wu TJ, Liu CC, Ng CC, Chien CC, Sun HL. Meperidine-induced serotonin syndrome in a susceptible patient. Br J Anaesth. 2009; 103:369–370. PMID: 19556270.

3. Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991; 148:705–713. PMID: 2035713.
4. Volpi-Abadie J, Kaye AM, Kaye AD. Serotonin syndrome. Ochsner J. 2013; 13:533–540. PMID: 24358002.
5. Gillman PK. Serotonin syndrome treated with chlorpromazine. J Clin Psychopharmacol. 1997; 17:128–129. PMID: 10950482.

6. Horowitz BZ, Mullins ME. Cyproheptadine for serotonin syndrome in an accidental pediatric sertraline ingestion. Pediatr Emerg Care. 1999; 15:325–327. PMID: 10532660.

7. Shioda K, Nisijima K, Yoshino T, Kuboshima K, Iwamura T, Yui K, et al. Risperidone attenuates and reverses hyperthermia induced by 3,4-methylenedioxymethamphetamine (MDMA) in rats. Neurotoxicology. 2008; 29:1030–1036. PMID: 18722468.

8. Guzé BH, Baxter LR Jr. The serotonin syndrome: case responsive to propranolol. J Clin Psychopharmacol. 1986; 6:119–120. PMID: 3700697.
9. Nisijima K, Nibuya M, Kato S. Toxic serotonin syndrome successfully treated with electroconvulsive therapy. J Clin Psychopharmacol. 2002; 22:338–339. PMID: 12006909.

10. von Einsiedel RW, Roesch-Ely D, Diebold K, Sartor K, Mundt C, Bergemann N. H(2)-histamine antagonist (famotidine) induced adverse CNS reactions with long-standing secondary mania and epileptic seizures. Pharmacopsychiatry. 2002; 35:152–154. PMID: 12163986.

11. Catalano G, Catalano MC, Alberts VA. Famotidine-associated delirium. A series of six cases. Psychosomatics. 1996; 37:349–355. PMID: 8701013.
12. Lai KH, Cho CH, Ogle CW, Wang JY. Effects of eight-week treatment with histamine H2-antagonists or an antacid on plasma levels of histamine and serotonin in duodenal ulcer patients. Pharmacol Res Commun. 1986; 18:807–812. PMID: 2432622.

13. Fisher AA, Davis MW. Serotonin syndrome caused by selective serotonin reuptake-inhibitors-metoclopramide interaction. Ann Pharmacother. 2002; 36:67–71. PMID: 11816261.

14. Vandemergel X, Beukinga I, Nève P. Serotonin syndrome secondary to the use of sertraline and metoclopramide. Rev Med Brux. 2000; 21:161–163. PMID: 10925598.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download